INHALED ANESTHETICS 7 Rachel Eshima Mckay
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Competency Framework for Anesthesia Assistance
National Competency Framework In Anesthesia Assistance Validated June 2016 201-2460 Lancaster Road Ottawa, Ontario K1B 4S5 1 INTRODUCTION ................................................................................................................ 3 ACKNOWLEDGEMENTS .................................................................................................. 3 HISTORICAL PERSPECTIVE ............................................................................................ 4 UNDERSTANDING THIS DOCUMENT ........................................................................... 6 SECTION 1: PROFESSIONAL AND ORGANIZATIONAL COMPETENCIES ............. 7 A. Demonstrate professionalism toward patients and their families, co-workers and the public .................................................................................................................................... 7 B. Demonstrate effective communication with the patient and their families, co-workers and the public ........................................................................................................................ 7 C. Demonstrate critical thinking and reasoning ............................................................... 7 D. Ensure the health and safety of the patient, co-workers and self ................................ 8 E. Use evidence to inform practice .................................................................................. 8 F. Perform administrative duties ..................................................................................... -

Pharmacology – Inhalant Anesthetics
Pharmacology- Inhalant Anesthetics Lyon Lee DVM PhD DACVA Introduction • Maintenance of general anesthesia is primarily carried out using inhalation anesthetics, although intravenous anesthetics may be used for short procedures. • Inhalation anesthetics provide quicker changes of anesthetic depth than injectable anesthetics, and reversal of central nervous depression is more readily achieved, explaining for its popularity in prolonged anesthesia (less risk of overdosing, less accumulation and quicker recovery) (see table 1) Table 1. Comparison of inhalant and injectable anesthetics Inhalant Technique Injectable Technique Expensive Equipment Cheap (needles, syringes) Patent Airway and high O2 Not necessarily Better control of anesthetic depth Once given, suffer the consequences Ease of elimination (ventilation) Only through metabolism & Excretion Pollution No • Commonly administered inhalant anesthetics include volatile liquids such as isoflurane, halothane, sevoflurane and desflurane, and inorganic gas, nitrous oxide (N2O). Except N2O, these volatile anesthetics are chemically ‘halogenated hydrocarbons’ and all are closely related. • Physical characteristics of volatile anesthetics govern their clinical effects and practicality associated with their use. Table 2. Physical characteristics of some volatile anesthetic agents. (MAC is for man) Name partition coefficient. boiling point MAC % blood /gas oil/gas (deg=C) Nitrous oxide 0.47 1.4 -89 105 Cyclopropane 0.55 11.5 -34 9.2 Halothane 2.4 220 50.2 0.75 Methoxyflurane 11.0 950 104.7 0.2 Enflurane 1.9 98 56.5 1.68 Isoflurane 1.4 97 48.5 1.15 Sevoflurane 0.6 53 58.5 2.5 Desflurane 0.42 18.7 25 5.72 Diethyl ether 12 65 34.6 1.92 Chloroform 8 400 61.2 0.77 Trichloroethylene 9 714 86.7 0.23 • The volatile anesthetics are administered as vapors after their evaporization in devices known as vaporizers. -

Low-Flow, Minimal-Flow and Metabolic-Flow Anaesthesia Clinical Techniques for Use with Rebreathing Systems ACKNOWLEDGEMENT: AHEAD of HIS TIME Professor Jan A
Low-flow, minimal-flow and metabolic-flowLow-flow, anaesthesia D-38293-2015 Low-flow, minimal-flow and metabolic-flow anaesthesia Clinical techniques for use with rebreathing systems Christian Hönemann Bert Mierke Drägerwerk KGaA & Co. AG IMPORTANT NOTES Medical expertise is continually undergoing change due to research and clinical experience. The authors of this book intend to ensure that the views, opinions and assumptions in this book, especially those concerning applications and effects, correspond to the current state of knowledge. But this does not relieve the reader from the duty to personally carry the responsibilities for clinical measures. The use of registered names, trademarks, etc. in this publication does not mean that such names are exempt from the applicable protection laws and regulations, even if there are no related specific statements. All rights to this book, especially the rights to reproduce and copy, are reserved by Drägerwerk AG & Co. KGaA. No part of this book may be reproduced or stored mechanically, electronically or photographically without prior written authorization by Drägerwerk AG & Co. KGaA. Fabius®, Primus®, Zeus® and Perseus® are trademarks of Dräger. AUTHORS Christian Hönemann Bert Mierke PhD, MD PhD, MD Vice Medical Director Medical Director Chief physician in the collegiate system of Chief physician of the Clinic for the department of Anaesthesia and Operative Anesthesiology and Intensive Care Intensive Care, St. Marienhospital Vechta St. Elisabeth GmbH, Lindenstraße 3–7, Catholic Clinics Oldenburger Münsterland, 49401 Damme, Germany Marienstraβe 6–8, 49377 Vechta, Germany Low-flow, minimal-flow and metabolic-flow anaesthesia Clinical techniques for use with rebreathing systems ACKNOWLEDGEMENT: AHEAD OF HIS TIME Professor Jan A. -

Pharmacokinetics and Pharmacology of Drugs Used in Children
Drug and Fluid Th erapy SECTION II Pharmacokinetics and Pharmacology of Drugs Used CHAPTER 6 in Children Charles J. Coté, Jerrold Lerman, Robert M. Ward, Ralph A. Lugo, and Nishan Goudsouzian Drug Distribution Propofol Protein Binding Ketamine Body Composition Etomidate Metabolism and Excretion Muscle Relaxants Hepatic Blood Flow Succinylcholine Renal Excretion Intermediate-Acting Nondepolarizing Relaxants Pharmacokinetic Principles and Calculations Atracurium First-Order Kinetics Cisatracurium Half-Life Vecuronium First-Order Single-Compartment Kinetics Rocuronium First-Order Multiple-Compartment Kinetics Clinical Implications When Using Short- and Zero-Order Kinetics Intermediate-Acting Relaxants Apparent Volume of Distribution Long-Acting Nondepolarizing Relaxants Repetitive Dosing and Drug Accumulation Pancuronium Steady State Antagonism of Muscle Relaxants Loading Dose General Principles Central Nervous System Effects Suggamadex The Drug Approval Process, the Package Insert, and Relaxants in Special Situations Drug Labeling Opioids Inhalation Anesthetic Agents Morphine Physicochemical Properties Meperidine Pharmacokinetics of Inhaled Anesthetics Hydromorphone Pharmacodynamics of Inhaled Anesthetics Oxycodone Clinical Effects Methadone Nitrous Oxide Fentanyl Environmental Impact Alfentanil Oxygen Sufentanil Intravenous Anesthetic Agents Remifentanil Barbiturates Butorphanol and Nalbuphine 89 A Practice of Anesthesia for Infants and Children Codeine Antiemetics Tramadol Metoclopramide Nonsteroidal Anti-infl ammatory Agents 5-Hydroxytryptamine -

Accidental Awareness During General Anaesthesia (AAGA) in Obstetrics
O B S T E T R I C A N A E S T H E S I A Tutorial 388 Accidental Awareness during General Anaesthesia (AAGA) in Obstetrics Dr. Rezaur Rahman Specialty Registrar in Anaesthetics, Queen Alexandra Hospital, Portsmouth, United Kingdom Dr. Samantha Wilson Consultant Anaesthetist, Basingstoke and North Hampshire Hospital, Basingstoke, United Kingdom Edited by Dr James Brown,i Dr Gill Abirii i Consultant Anesthesiologist, BC Women’s Hospital, Canada ii Clinical Associate Professor, Stanford University School of Medicine, USA nd Correspondence to [email protected] 2 Oct 2018 An online test is available for self-directed Continuous Medical Education (CME). A certificate will be awarded upon passing the test. Please refer to the accreditation policy here. Take online quiz KEY POINTS Accidental awareness during general anaesthesia is more common in obstetric practice than in any other discipline of anaesthesia Factors contributing to an increased risk of accidental awareness during general anaesthesia include maternal stress or anxiety, emergency surgery and the “intravenous-inhalational” interval Accidental awareness during general anaesthesia can be associated with considerable physiological and psychological harm Strategies to minimise the risk of accidental awareness during general anaesthesia include an appropriate dose of anaesthetic induction agent, and use of nitrous oxide to achieve an adequate depth of anaesthesia INTRODUCTION Accidental awareness during general anaesthesia (AAGA) is defined as the unintended experience and subsequent recall of intra-operative events. In recent decades, the incidence of AAGA has been reported as between 1–2:1,000 general anaesthetics (1). The landmark NAP5 report (Fifth National Audit Project) - a national survey conducted by The Royal College of Anaesthetists (RCOA) which investigated spontaneous reports of AAGA - demonstrated an incidence of 1:19,000 in the general population. -
BASIC Examination Questions with Answer
BASIC Examination Questions 1. Which of the following nerves should be blocked for an operation at the medial aspect of the lower leg? A. Femoral B. Sciatic C. Common peroneal D. Tibial 2. A patient is scheduled to undergo laparoscopic cholecystectomy. Thirty minutes after receiving premedication with morphine and midazolam, she suddenly develops right upper quadrant abdominal pain and nausea. Which of the following is the most appropriate therapy for this patient’s pain? A. Flumazenil B. Ketorolac C. Naloxone D. Ranitidine 3. The relaxant effect of vecuronium on the neuromuscular system is augmented by adding a volatile anesthetic to a nitrous oxide/opioid anesthetic because of a decrease in: A. Muscle blood flow. B. Release of acetylcholine at the motor end-plate. C. Reuptake of acetylcholine at the motor end-plate. D. Sensitivity of the postjunctional membrane to depolarization. 4. An 85-kg, 35-year-old woman has persistent somnolence after a prolonged lower extremity orthopedic procedure during spinal anesthesia. During the last two hours of surgery, midazolam 5 mg and fentanyl 150 µg were administered for increasing restlessness and discomfort. Which of the following is most likely to result from administration of flumazenil? A. Grand mal seizure B. Hypertension and tachycardia C. Reversal of somnolence followed by resedation D. Sudden onset of pulmonary edema 5. A 68-year-old woman with primary hyperparathyroidism is scheduled to undergo parathyroidectomy. Her serum calcium concentration is 15 mg/dL. The most appropriate initial management is intravenous administration of: A. Indomethacin B. Magnesium sulfate C. Methylprednisolone D. Normal saline 6. Which of the following tests most reliably predicts the likelihood that a patient will develop malignant hyperthermia? A. -

Inhalational Anesthetics
UPTAKE AND DISTRIBUTION OF INHALATIONAL ANESTHETICS Dr.J.Edward Johnson.M.D.(Anaes),D.C.H. Asst.Professor, Kanyakumari Govt. Medical College Hospital. INTRODUCTION The modern anesthetist expeditiously develops and then sustains anesthetic concentrations in the central nervous system that are sufficient for surgery with agents and techniques that usually permit rapid recovery from anesthesia. Understanding the factors that govern the relationship between the delivered anesthetic and brain concentrations enhances the optimum conduct of anesthesia. I. UPTAKE OF INHALED ANESTHETICS. A. Factors raising the alveolar concentration, assuming a constant inspired anesthetic concentration, and no uptake by blood: 1. The inspired concentration (FI). a. The rate of rise is directly proportional to the inspired concentration. 2. The alveolar ventilation (Valveolar) a. The larger the minute alveolar ventilation (Valveolar), the more rapid the rise in alveolar concentration (FA) . b. Inspired gas is diluted by the FRC, so the larger the FRC, as a fraction of Valveolar, the slower the alveolar rise in anesthetic concentration. c. For ventilatory rates over 4 breaths, the ventilatory rate does not make any difference at the same Valveolar. 3. The time constant The time required for flow through a container to equal the capacity of the container. Time constant = volume (capacity)/flow Time Constant % washin/washout 1 63% 2 86% 3 95% 4 98% For example; If 10 liter box is initially filled with oxygen and 5 l/min of nitrogen flow into box then, the TC is volume (capacity)/flow. TC = 10 / 5 = 2 minutes. So, the nitrogen concentration at end of 2 minutes is 63%. -

Midazolam Injection, USP
Midazolam Injection, USP Rx only PHARMACY BULK PACKAGE – NOT FOR DIRECT INFUSION WARNING ADULTS AND PEDIATRICS: Intravenous midazolam has been associated with respiratory depression and respiratory arrest, especially when used for sedation in noncritical care settings. In some cases, where this was not recognized promptly and treated effectively, death or hypoxic encephalopathy has resulted. Intravenous midazolam should be used only in hospital or ambulatory care settings, including physicians’ and dental offices, that provide for continuous monitoring of respiratory and cardiac function, i.e., pulse oximetry. Immediate availability of resuscitative drugs and age- and size-appropriate equipment for bag/valve/mask ventilation and intubation, and personnel trained in their use and skilled in airway management should be assured (see WARNINGS). For deeply sedated pediatric patients, a dedicated individual, other than the practitioner performing the procedure, should monitor the patient throughout the procedures. The initial intravenous dose for sedation in adult patients may be as little as 1 mg, but should not exceed 2.5 mg in a normal healthy adult. Lower doses are necessary for older (over 60 years) or debilitated patients and in patients receiving concomitant narcotics or other central nervous system (CNS) depressants. The initial dose and all subsequent doses should always be titrated slowly; administer over at least 2 minutes and 1 allow an additional 2 or more minutes to fully evaluate the sedative effect. The dilution of the 5 mg/mL formulation is recommended to facilitate slower injection. Doses of sedative medications in pediatric patients must be calculated on a mg/kg basis, and initial doses and all subsequent doses should always be titrated slowly. -

The Effects of Ventilation-Perfusion Scatter on Gas Exchange During Nitrous Oxide Anaesthesia
The effects of ventilation-perfusion scatter on gas exchange during nitrous oxide anaesthesia A thesis submitted in total fulfilment of the requirements for the degree of Doctor of Philosophy By Dr. Philip John Peyton MD MBBS FANZCA Department of Anaesthesia Austin Hospital and University Department of Surgery Austin Hospital and University of Melbourne 2011 Printed on Archival Quality Paper ii Abstract Nitrous oxide (N2O) is the oldest anaesthetic agent still in clinical use. Due to its weak anaesthetic potency, it is customarily administered at concentrations as high as 70%, in combination with the more potent volatile anaesthetic agents. It allows a dose reduction of these agents and, unlike them, is characterised by remarkable cardiovascular and respiratory stability and has analgesic properties. Its low solubility in blood and body tissues produces rapid washin into the body on induction and rapid washout on emergence at the end of surgery. Its rapid early uptake by the lungs is known to produce a concentrating effect on the accompanying alveolar oxygen (O2) and volatile agent, increasing their alveolar concentration and enhancing their uptake, which speeds induction of anaesthesia. This is called the “second gas effect”. The place of N2O in modern anaesthetic practice has increasingly been criticised. It has a number of potential adverse effects, such as immunosuppression with prolonged exposure, and the possibility of cardiovascular complications due to acute elevation of plasma homocysteine levels is currently being investigated. It has been implicated as a cause of post-operative nausea and vomiting (PONV), and is a greenhouse gas pollutant. Its continued use relies largely on its perceived pharmacokinetic advantages, but these have been questioned. -
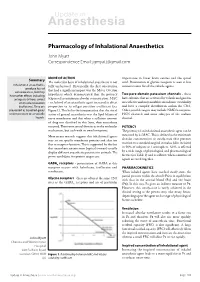
Pharmacology of Inhalational Anaesthetics John Myatt Correspondence Email: [email protected]
Update in Anaesthesia Pharmacology of Inhalational Anaesthetics John Myatt Correspondence Email: [email protected] MODE OF ACTION Summary importance in lower brain centres and the spinal The molecular basis of inhalational anaesthesia is not cord. Potentiation of glycine receptors is seen at low Inhalational anaesthetics fully understood. Historically, the first observation concentrations for all the volatile agents. produce loss of consciousness, but may that had a significant impact was the Meyer-Overton Two-pore-domain potassium channels have other effects including hypothesis which demonstrated that the potency - these analgesia (nitrous oxide) (expressed as minimum alveolar concentration, MAC have subunits that are activated by volatile and gaseous or muscle relaxation - see below) of an anaesthetic agent increased in direct anaesthetics and may modulate membrane excitability (isoflurane). They are proportion to its oil:gas partition coefficient (see and have a complex distribution within the CNS. presented as liquefied gases Figure 1). This led to the interpretation that the site of Other possible targets may include NMDA receptors, under pressure or as volatile action of general anaesthetics was the lipid bilayer of HCN channels and some subtypes of the sodium liquids. nerve membranes and that when a sufficient amount channel. of drug was dissolved in this layer, then anaesthesia occurred. There were several theories as to the molecular POTENCY mechanism, but each with its own limitations. The potency of an inhalational anaesthetic agent can be More recent research suggests that inhalational agents measured by its MAC. This is defined as the minimum may act on specific membrane proteins and alter ion alveolar concentration at steady-state that prevents flux or receptor function. -

Performance of Anesthetic Depth Indexes in Rabbits Under Propofol Anesthesia Prediction Probabilities and Concentration-Effect Relations
Performance of Anesthetic Depth Indexes in Rabbits under Propofol Anesthesia Prediction Probabilities and Concentration-effect Relations Aura Silva, M.Sc.,* So´ nia Campos, M.Sc.,† Joaquim Monteiro, Ph.D.,‡ Carlos Venaˆ ncio, M.Sc.,* Bertinho Costa, Ph.D.,§ Paula Guedes de Pinho, Ph.D.,ʈ Luis Antunes, Ph.D.# Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/115/2/303/255162/0000542-201108000-00017.pdf by guest on 30 September 2021 ABSTRACT What We Already Know about This Topic • A number of electroencephalogram-based measures have Background: The permutation entropy, the approximate been studied to determine their usefulness for intraoperative entropy, and the index of consciousness are some of the most monitoring of anesthetic depth • recently studied electroencephalogram-derived indexes. In In rats anesthetized with a potent volatile anesthetic, burst suppression-corrected permutation entropy had the best cor- this work, a thorough comparison of these indexes was per- relation with anesthetic dose formed using propofol anesthesia in a rabbit model. Methods: Six rabbits were anesthetized with three propofol Ϫ Ϫ infusion rates: 70, 100, and 130 mg ⅐ kg 1 ⅐ h 1, each main- tained for 30 min, in a random order for each animal. What This Article Tells Us That Is New Data recording was performed in the awake animals 20, • In rabbits receiving propofol by infusion, burst suppression- 25, and 30 min after each infusion rate was begun in the corrected permutation entropy and burst suppression-cor- rected composite multiscale permutation entropy had the recovered animals and consisted of electroencephalogram best propofol concentration-effect relationships and predic- recordings, evaluation of depth of anesthesia according to a clinical tions of clinical signs scale, and arterial blood samples for plasma propofol determination. -

Nitrous Oxide Diffusion and the Second Gas Effect on Emergence from Anesthesia
Nitrous Oxide Diffusion and the Second Gas Effect on Emergence from Anesthesia Philip J. Peyton, M.D.,* Ian Chao, M.B.B.S.,† Laurence Weinberg, F.A.N.Z.C.A.,‡ Gavin J. B. Robinson, F.A.N.Z.C.A.,§ Bruce R. Thompson, Ph.D. ABSTRACT What We Already Know about This Topic Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/114/3/596/253394/0000542-201103000-00026.pdf by guest on 27 September 2021 • The increase in the partial pressures of the other gases in the Background: Rapid elimination of nitrous oxide from the alveolar mixture resulting from the rapid uptake of high con- lungs at the end of inhalational anesthesia dilutes alveolar centrations of nitrous oxide during inhalational anesthesia in- duction is known as the second gas effect. oxygen, producing “diffusion hypoxia.” A similar dilutional effect on accompanying volatile anesthetic agent has not been evaluated and may impact the speed of emergence. Methods: Twenty patients undergoing surgery were ran- What This Article Tells Us That Is New domly assigned to receive an anesthetic maintenance gas • The second gas effect also occurs during emergence, with the mixture of sevoflurane adjusted to bispectral index, in air- rapid removal of nitrous oxide increasing the removal of other oxygen (control group) versus a 2:1 mixture of nitrous oxide- volatile anesthetics. oxygen (nitrous oxide group). After surgery, baseline arterial and tidal gas samples were taken. Patients were ventilated reduction of concentrations of the accompanying volatile with oxygen, and arterial and tidal gas sampling was repeated agents, contributing to the speed of emergence observed after at 2 and 5 min.