The Effects of Ventilation-Perfusion Scatter on Gas Exchange During Nitrous Oxide Anaesthesia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Competency Framework for Anesthesia Assistance
National Competency Framework In Anesthesia Assistance Validated June 2016 201-2460 Lancaster Road Ottawa, Ontario K1B 4S5 1 INTRODUCTION ................................................................................................................ 3 ACKNOWLEDGEMENTS .................................................................................................. 3 HISTORICAL PERSPECTIVE ............................................................................................ 4 UNDERSTANDING THIS DOCUMENT ........................................................................... 6 SECTION 1: PROFESSIONAL AND ORGANIZATIONAL COMPETENCIES ............. 7 A. Demonstrate professionalism toward patients and their families, co-workers and the public .................................................................................................................................... 7 B. Demonstrate effective communication with the patient and their families, co-workers and the public ........................................................................................................................ 7 C. Demonstrate critical thinking and reasoning ............................................................... 7 D. Ensure the health and safety of the patient, co-workers and self ................................ 8 E. Use evidence to inform practice .................................................................................. 8 F. Perform administrative duties ..................................................................................... -

Pharmacology – Inhalant Anesthetics
Pharmacology- Inhalant Anesthetics Lyon Lee DVM PhD DACVA Introduction • Maintenance of general anesthesia is primarily carried out using inhalation anesthetics, although intravenous anesthetics may be used for short procedures. • Inhalation anesthetics provide quicker changes of anesthetic depth than injectable anesthetics, and reversal of central nervous depression is more readily achieved, explaining for its popularity in prolonged anesthesia (less risk of overdosing, less accumulation and quicker recovery) (see table 1) Table 1. Comparison of inhalant and injectable anesthetics Inhalant Technique Injectable Technique Expensive Equipment Cheap (needles, syringes) Patent Airway and high O2 Not necessarily Better control of anesthetic depth Once given, suffer the consequences Ease of elimination (ventilation) Only through metabolism & Excretion Pollution No • Commonly administered inhalant anesthetics include volatile liquids such as isoflurane, halothane, sevoflurane and desflurane, and inorganic gas, nitrous oxide (N2O). Except N2O, these volatile anesthetics are chemically ‘halogenated hydrocarbons’ and all are closely related. • Physical characteristics of volatile anesthetics govern their clinical effects and practicality associated with their use. Table 2. Physical characteristics of some volatile anesthetic agents. (MAC is for man) Name partition coefficient. boiling point MAC % blood /gas oil/gas (deg=C) Nitrous oxide 0.47 1.4 -89 105 Cyclopropane 0.55 11.5 -34 9.2 Halothane 2.4 220 50.2 0.75 Methoxyflurane 11.0 950 104.7 0.2 Enflurane 1.9 98 56.5 1.68 Isoflurane 1.4 97 48.5 1.15 Sevoflurane 0.6 53 58.5 2.5 Desflurane 0.42 18.7 25 5.72 Diethyl ether 12 65 34.6 1.92 Chloroform 8 400 61.2 0.77 Trichloroethylene 9 714 86.7 0.23 • The volatile anesthetics are administered as vapors after their evaporization in devices known as vaporizers. -

Low-Flow, Minimal-Flow and Metabolic-Flow Anaesthesia Clinical Techniques for Use with Rebreathing Systems ACKNOWLEDGEMENT: AHEAD of HIS TIME Professor Jan A
Low-flow, minimal-flow and metabolic-flowLow-flow, anaesthesia D-38293-2015 Low-flow, minimal-flow and metabolic-flow anaesthesia Clinical techniques for use with rebreathing systems Christian Hönemann Bert Mierke Drägerwerk KGaA & Co. AG IMPORTANT NOTES Medical expertise is continually undergoing change due to research and clinical experience. The authors of this book intend to ensure that the views, opinions and assumptions in this book, especially those concerning applications and effects, correspond to the current state of knowledge. But this does not relieve the reader from the duty to personally carry the responsibilities for clinical measures. The use of registered names, trademarks, etc. in this publication does not mean that such names are exempt from the applicable protection laws and regulations, even if there are no related specific statements. All rights to this book, especially the rights to reproduce and copy, are reserved by Drägerwerk AG & Co. KGaA. No part of this book may be reproduced or stored mechanically, electronically or photographically without prior written authorization by Drägerwerk AG & Co. KGaA. Fabius®, Primus®, Zeus® and Perseus® are trademarks of Dräger. AUTHORS Christian Hönemann Bert Mierke PhD, MD PhD, MD Vice Medical Director Medical Director Chief physician in the collegiate system of Chief physician of the Clinic for the department of Anaesthesia and Operative Anesthesiology and Intensive Care Intensive Care, St. Marienhospital Vechta St. Elisabeth GmbH, Lindenstraße 3–7, Catholic Clinics Oldenburger Münsterland, 49401 Damme, Germany Marienstraβe 6–8, 49377 Vechta, Germany Low-flow, minimal-flow and metabolic-flow anaesthesia Clinical techniques for use with rebreathing systems ACKNOWLEDGEMENT: AHEAD OF HIS TIME Professor Jan A. -

Pharmacokinetics and Pharmacology of Drugs Used in Children
Drug and Fluid Th erapy SECTION II Pharmacokinetics and Pharmacology of Drugs Used CHAPTER 6 in Children Charles J. Coté, Jerrold Lerman, Robert M. Ward, Ralph A. Lugo, and Nishan Goudsouzian Drug Distribution Propofol Protein Binding Ketamine Body Composition Etomidate Metabolism and Excretion Muscle Relaxants Hepatic Blood Flow Succinylcholine Renal Excretion Intermediate-Acting Nondepolarizing Relaxants Pharmacokinetic Principles and Calculations Atracurium First-Order Kinetics Cisatracurium Half-Life Vecuronium First-Order Single-Compartment Kinetics Rocuronium First-Order Multiple-Compartment Kinetics Clinical Implications When Using Short- and Zero-Order Kinetics Intermediate-Acting Relaxants Apparent Volume of Distribution Long-Acting Nondepolarizing Relaxants Repetitive Dosing and Drug Accumulation Pancuronium Steady State Antagonism of Muscle Relaxants Loading Dose General Principles Central Nervous System Effects Suggamadex The Drug Approval Process, the Package Insert, and Relaxants in Special Situations Drug Labeling Opioids Inhalation Anesthetic Agents Morphine Physicochemical Properties Meperidine Pharmacokinetics of Inhaled Anesthetics Hydromorphone Pharmacodynamics of Inhaled Anesthetics Oxycodone Clinical Effects Methadone Nitrous Oxide Fentanyl Environmental Impact Alfentanil Oxygen Sufentanil Intravenous Anesthetic Agents Remifentanil Barbiturates Butorphanol and Nalbuphine 89 A Practice of Anesthesia for Infants and Children Codeine Antiemetics Tramadol Metoclopramide Nonsteroidal Anti-infl ammatory Agents 5-Hydroxytryptamine -
BASIC Examination Questions with Answer
BASIC Examination Questions 1. Which of the following nerves should be blocked for an operation at the medial aspect of the lower leg? A. Femoral B. Sciatic C. Common peroneal D. Tibial 2. A patient is scheduled to undergo laparoscopic cholecystectomy. Thirty minutes after receiving premedication with morphine and midazolam, she suddenly develops right upper quadrant abdominal pain and nausea. Which of the following is the most appropriate therapy for this patient’s pain? A. Flumazenil B. Ketorolac C. Naloxone D. Ranitidine 3. The relaxant effect of vecuronium on the neuromuscular system is augmented by adding a volatile anesthetic to a nitrous oxide/opioid anesthetic because of a decrease in: A. Muscle blood flow. B. Release of acetylcholine at the motor end-plate. C. Reuptake of acetylcholine at the motor end-plate. D. Sensitivity of the postjunctional membrane to depolarization. 4. An 85-kg, 35-year-old woman has persistent somnolence after a prolonged lower extremity orthopedic procedure during spinal anesthesia. During the last two hours of surgery, midazolam 5 mg and fentanyl 150 µg were administered for increasing restlessness and discomfort. Which of the following is most likely to result from administration of flumazenil? A. Grand mal seizure B. Hypertension and tachycardia C. Reversal of somnolence followed by resedation D. Sudden onset of pulmonary edema 5. A 68-year-old woman with primary hyperparathyroidism is scheduled to undergo parathyroidectomy. Her serum calcium concentration is 15 mg/dL. The most appropriate initial management is intravenous administration of: A. Indomethacin B. Magnesium sulfate C. Methylprednisolone D. Normal saline 6. Which of the following tests most reliably predicts the likelihood that a patient will develop malignant hyperthermia? A. -

Inhalational Anesthetics
UPTAKE AND DISTRIBUTION OF INHALATIONAL ANESTHETICS Dr.J.Edward Johnson.M.D.(Anaes),D.C.H. Asst.Professor, Kanyakumari Govt. Medical College Hospital. INTRODUCTION The modern anesthetist expeditiously develops and then sustains anesthetic concentrations in the central nervous system that are sufficient for surgery with agents and techniques that usually permit rapid recovery from anesthesia. Understanding the factors that govern the relationship between the delivered anesthetic and brain concentrations enhances the optimum conduct of anesthesia. I. UPTAKE OF INHALED ANESTHETICS. A. Factors raising the alveolar concentration, assuming a constant inspired anesthetic concentration, and no uptake by blood: 1. The inspired concentration (FI). a. The rate of rise is directly proportional to the inspired concentration. 2. The alveolar ventilation (Valveolar) a. The larger the minute alveolar ventilation (Valveolar), the more rapid the rise in alveolar concentration (FA) . b. Inspired gas is diluted by the FRC, so the larger the FRC, as a fraction of Valveolar, the slower the alveolar rise in anesthetic concentration. c. For ventilatory rates over 4 breaths, the ventilatory rate does not make any difference at the same Valveolar. 3. The time constant The time required for flow through a container to equal the capacity of the container. Time constant = volume (capacity)/flow Time Constant % washin/washout 1 63% 2 86% 3 95% 4 98% For example; If 10 liter box is initially filled with oxygen and 5 l/min of nitrogen flow into box then, the TC is volume (capacity)/flow. TC = 10 / 5 = 2 minutes. So, the nitrogen concentration at end of 2 minutes is 63%. -
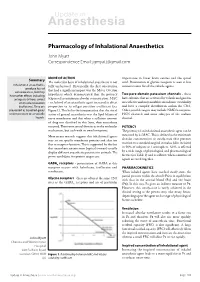
Pharmacology of Inhalational Anaesthetics John Myatt Correspondence Email: [email protected]
Update in Anaesthesia Pharmacology of Inhalational Anaesthetics John Myatt Correspondence Email: [email protected] MODE OF ACTION Summary importance in lower brain centres and the spinal The molecular basis of inhalational anaesthesia is not cord. Potentiation of glycine receptors is seen at low Inhalational anaesthetics fully understood. Historically, the first observation concentrations for all the volatile agents. produce loss of consciousness, but may that had a significant impact was the Meyer-Overton Two-pore-domain potassium channels have other effects including hypothesis which demonstrated that the potency - these analgesia (nitrous oxide) (expressed as minimum alveolar concentration, MAC have subunits that are activated by volatile and gaseous or muscle relaxation - see below) of an anaesthetic agent increased in direct anaesthetics and may modulate membrane excitability (isoflurane). They are proportion to its oil:gas partition coefficient (see and have a complex distribution within the CNS. presented as liquefied gases Figure 1). This led to the interpretation that the site of Other possible targets may include NMDA receptors, under pressure or as volatile action of general anaesthetics was the lipid bilayer of HCN channels and some subtypes of the sodium liquids. nerve membranes and that when a sufficient amount channel. of drug was dissolved in this layer, then anaesthesia occurred. There were several theories as to the molecular POTENCY mechanism, but each with its own limitations. The potency of an inhalational anaesthetic agent can be More recent research suggests that inhalational agents measured by its MAC. This is defined as the minimum may act on specific membrane proteins and alter ion alveolar concentration at steady-state that prevents flux or receptor function. -

Nitrous Oxide Diffusion and the Second Gas Effect on Emergence from Anesthesia
Nitrous Oxide Diffusion and the Second Gas Effect on Emergence from Anesthesia Philip J. Peyton, M.D.,* Ian Chao, M.B.B.S.,† Laurence Weinberg, F.A.N.Z.C.A.,‡ Gavin J. B. Robinson, F.A.N.Z.C.A.,§ Bruce R. Thompson, Ph.D. ABSTRACT What We Already Know about This Topic Downloaded from http://pubs.asahq.org/anesthesiology/article-pdf/114/3/596/253394/0000542-201103000-00026.pdf by guest on 27 September 2021 • The increase in the partial pressures of the other gases in the Background: Rapid elimination of nitrous oxide from the alveolar mixture resulting from the rapid uptake of high con- lungs at the end of inhalational anesthesia dilutes alveolar centrations of nitrous oxide during inhalational anesthesia in- duction is known as the second gas effect. oxygen, producing “diffusion hypoxia.” A similar dilutional effect on accompanying volatile anesthetic agent has not been evaluated and may impact the speed of emergence. Methods: Twenty patients undergoing surgery were ran- What This Article Tells Us That Is New domly assigned to receive an anesthetic maintenance gas • The second gas effect also occurs during emergence, with the mixture of sevoflurane adjusted to bispectral index, in air- rapid removal of nitrous oxide increasing the removal of other oxygen (control group) versus a 2:1 mixture of nitrous oxide- volatile anesthetics. oxygen (nitrous oxide group). After surgery, baseline arterial and tidal gas samples were taken. Patients were ventilated reduction of concentrations of the accompanying volatile with oxygen, and arterial and tidal gas sampling was repeated agents, contributing to the speed of emergence observed after at 2 and 5 min. -

Nitrous Oxide Use in Children
Rev Bras Anestesiol SPECIAL ARTICLE 2012; 62: 3: 451-467 SPECIAL ARTICLE Nitrous Oxide Use in Children Leonardo Teixeira Domingues Duarte 1, Gastão Fernandes Duval Neto 2, Florentino Fernandes Mendes 3 Summary: Duarte LTD, Duval Neto GF, Mendes FF – Nitrous Oxide Use in Children. ©2012 Elsevier Editora Ltda. All rights reserved. DESCRIPTION OF THE EVIDENCE COLLECTION 11. Nitrous Oxide [MeSH] AND Anesthesia, General METHOD [MeSH] AND Child [MeSH] AND Randomized Con- trolled Trial[ptyp] Searches were carried out in multiple databases (Medline 12. Pediatrics [MeSH] OR Neonatology [MeSH] AND Ni- 1965 to 2009, Cochrane Library, LILACS) and cross-referenc- trous Oxide [MeSH] es with the collected material to identify articles with better 13. Nitrous Oxide [MeSH] AND Anesthesia, General methodological design, followed by critical evaluation of their [MeSH] AND Pediatrics [MeSH] AND Randomized content and classification according with the strength of evi- Controlled Trial[ptyp] dence. 14. Nitrous Oxide [MeSH] AND Anesthesia, General Searches occurred between December 2007 and April [MeSH] AND Neonatology [MeSH] AND Randomized 2008. The following search strategies were used for searches Controlled Trial[ptyp] in PubMed: 15. Cerebral Palsy [MeSH] AND Child [MeSH] AND Ni- trous Oxide [MeSH] 1. Nitrous Oxide [MeSH] AND Pharmacology [MeSH] AND Toxicology [MeSH] Studies comparing different classes of anesthetic drugs or 2. Nitrous Oxide [MeSH] AND Toxicology [MeSH] sedation techniques in children undergoing diagnostic tests 3. Nitrous Oxide [MeSH] AND toxicity [subheading] or procedures with the use of sedation or anesthesia were 4. Nitrous Oxide [MeSH] AND Acute Toxicity Tests selected. Also selected were studies that evaluated the phar- [MeSH] OR Toxicity Tests [MeSH] macological effects of nitrous oxide, its interaction with other 5. -

The Use of Midazolam, Isoflurane, and Nitrous Oxide for Sedation and Anesthesia of Ball Pythons (Python Regius)
The Use of Midazolam, Isoflurane, and Nitrous Oxide for Sedation and Anesthesia of Ball Pythons (Python regius) by Cédric B. Larouche A Thesis presented to The University of Guelph In partial fulfilment of requirements for the degree of Doctor of Veterinary Science in Pathobiology Guelph, Ontario, Canada © Cédric B. Larouche, August, 2019 ABSTRACT THE USE OF MIDAZOLAM, ISOFLURANE, AND NITROUS OXIDE FOR SEDATION AND ANESTHESIA OF BALL PYTHONS (PYTHON REGIUS) Cédric B. Larouche Co-advisors: University of Guelph, 2019 Nicole Nemeth Dorothee Bienzle The objectives of this project were to characterize the pharmacodynamics and pharmacokinetics of midazolam in the ball python (Python regius), and to evaluate the effects of midazolam and nitrous oxide (N2O) on the minimum anesthetic concentration of isoflurane (MACIso) in this species. The pharmacodynamics of midazolam were evaluated in a blinded, randomized, crossover study comparing two dosages (1 and 2 mg/kg intramuscular [IM]) in ten ball pythons. There were no significant differences between the two dosages for any parameter evaluated. Midazolam provided moderate sedation and muscle relaxation in all snakes starting 10-15 min post-injection and lasting up to 3-5 days, with a peak effect 60 min post-injection. Heart rates were significantly lower than baseline from 30 min to 5.3 days post-injection with both dosages. In an open trial using 9 ball pythons, the reversal effect of flumazenil was evaluated by administering 0.08 mg/kg IM 60 min after the administration of 1 mg/kg IM of midazolam. Sedation and muscle relaxation were fully reversed within 10 min of administration, but all snakes fully resedated within 3 h. -

Inhalant Anesthesia
Inhalant Anesthesia Horatiu V. Vinerean DVM, DACLAM Director, Laboratory Animal Research Attending Veterinarian 1 Inhalation Anesthesia - History 2 Inhalation Anesthesia • This is the technique of administering anesthetic agents to the animals via the lungs. • This consists of a volatile agent being vaporized by oxygen in a vaporizer and then being administered to the patient through an anesthetic breathing circuit. 3 Vaporization of volatile anesthetics • A vapor is a gas below its critical temperature. Both liquid and gaseous phases exist simultaneously and in a closed container a state of equilibrium is attained when the number of molecules leaving the liquid phase equals the number of molecules re-entering it. • In this situation, the vapor is said to be saturated and the partial pressure that the vapor exerts is the saturated vapor pressure (s.v.p.) that depends only upon the nature of the liquid and the temperature. 4 Anesthetic Uptake • The depth of anesthesia is related to the partial pressure of anesthetic agents in the brain. This is in turn related to the partial pressure in the blood and this, in turn, is related to the partial pressure of the agent in the alveoli of the lungs. • The mechanism for a gas to dissolve in the patients blood and other tissues relies on pressure and pressure gradients between the tissues or phases. • For an anesthetic action to occur the anesthetic agent must be capable of crossing the blood brain barrier to the central nervous system (lipid soluble). 5 Physics laws of anesthetic uptake • Dalton's Law of Partial Pressure: The constituent gases in gas mixtures act independently of each other and exert the pressure that each would have exerted in isolation in the given volume. -

The Effects of Ventilation-Perfusion Scatter on Gas Exchange During Nitrous Oxide Anaesthesia
The effects of ventilation-perfusion scatter on gas exchange during nitrous oxide anaesthesia A thesis submitted in total fulfilment of the requirements for the degree of Doctor of Philosophy By Dr. Philip John Peyton MD MBBS FANZCA Department of Anaesthesia Austin Hospital and University Department of Surgery Austin Hospital and University of Melbourne 2011 Printed on Archival Quality Paper ii Abstract Nitrous oxide (N2O) is the oldest anaesthetic agent still in clinical use. Due to its weak anaesthetic potency, it is customarily administered at concentrations as high as 70%, in combination with the more potent volatile anaesthetic agents. It allows a dose reduction of these agents and, unlike them, is characterised by remarkable cardiovascular and respiratory stability and has analgesic properties. Its low solubility in blood and body tissues produces rapid washin into the body on induction and rapid washout on emergence at the end of surgery. Its rapid early uptake by the lungs is known to produce a concentrating effect on the accompanying alveolar oxygen (O2) and volatile agent, increasing their alveolar concentration and enhancing their uptake, which speeds induction of anaesthesia. This is called the “second gas effect”. The place of N2O in modern anaesthetic practice has increasingly been criticised. It has a number of potential adverse effects, such as immunosuppression with prolonged exposure, and the possibility of cardiovascular complications due to acute elevation of plasma homocysteine levels is currently being investigated. It has been implicated as a cause of post-operative nausea and vomiting (PONV), and is a greenhouse gas pollutant. Its continued use relies largely on its perceived pharmacokinetic advantages, but these have been questioned.