Low-Flow, Minimal-Flow and Metabolic-Flow Anaesthesia Clinical Techniques for Use with Rebreathing Systems ACKNOWLEDGEMENT: AHEAD of HIS TIME Professor Jan A
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

National Competency Framework for Anesthesia Assistance
National Competency Framework In Anesthesia Assistance Validated June 2016 201-2460 Lancaster Road Ottawa, Ontario K1B 4S5 1 INTRODUCTION ................................................................................................................ 3 ACKNOWLEDGEMENTS .................................................................................................. 3 HISTORICAL PERSPECTIVE ............................................................................................ 4 UNDERSTANDING THIS DOCUMENT ........................................................................... 6 SECTION 1: PROFESSIONAL AND ORGANIZATIONAL COMPETENCIES ............. 7 A. Demonstrate professionalism toward patients and their families, co-workers and the public .................................................................................................................................... 7 B. Demonstrate effective communication with the patient and their families, co-workers and the public ........................................................................................................................ 7 C. Demonstrate critical thinking and reasoning ............................................................... 7 D. Ensure the health and safety of the patient, co-workers and self ................................ 8 E. Use evidence to inform practice .................................................................................. 8 F. Perform administrative duties ..................................................................................... -

An Introduction to Fast Dissolving Oral Thin Film Drug Delivery Systems: a Review
Muthadi Radhika Reddy /J. Pharm. Sci. & Res. Vol. 12(7), 2020, 925-940 An Introduction to Fast Dissolving Oral Thin Film Drug Delivery Systems: A Review Muthadi Radhika Reddy1* 1School of pharmacy, Gurunanak Institute of Technical Campus, Hyderabad, Telangana, India and Department of Pharmacy, Gandhi Institute of Technology and Management University, Vizag, Andhra Pradesh, India INTRODUCTION 2. Useful in situations where rapid onset of action Fast dissolving drug delivery systems were first developed required such as in motion sickness, allergic attack, in the late 1970s as an alternative to conventional dosage coughing or asthma forms. These systems consist of solid dosage forms that 3. Has wide range of applications in pharmaceuticals, Rx disintegrate and dissolve quickly in the oral cavity without Prescriptions and OTC medications for treating pain, the need of water [1]. Fast dissolving drug delivery cough/cold, gastro-esophageal reflux disease,erectile systems include orally disintegrating tablets (ODTs) and dysfunction, sleep disorders, dietary supplements, etc oral thin films (OTFs). The Centre for Drug Evaluation [4] and Research (CDER) defines ODTs as,“a solid dosage 4. No water is required for the administration and hence form containing medicinal substances which disintegrates suitable during travelling rapidly, usually within a matter of seconds, when placed 5. Some drugs are absorbed from the mouth, pharynx upon the tongue” [2]. USFDA defines OTFs as, “a thin, and esophagus as the saliva passes down into the flexible, non-friable polymeric film strip containing one or stomach, enhancing bioavailability of drugs more dispersed active pharmaceutical ingredients which is 6. May offer improved bioavailability for poorly water intended to be placed on the tongue for rapid soluble drugs by offering large surface area as it disintegration or dissolution in the saliva prior to disintegrates and dissolves rapidly swallowing for delivery into the gastrointestinal tract” [3]. -

Preparation and Characterization of Oil-In-Water and Water-In-Oil Emulsions
1 Preparation and Characterization of Oil-in-Water and Water-in-Oil Emulsions Prepared For Dr. Reza Foudazi, Ph.D. Chemical and Materials Engineering New Mexico State University By Muchu Zhou May 10, 2016 2 1 Introduction 1.1 Purpose of This Report The objective of this report is to clarify what I have done this semester for research course CHME 498. The research interest is “Preparation and Characterization of Oil-in-Water and Water-in-Oil Emulsions”. Thus, I would like to talk about what is emulsion, what are the main characteristics of emulsions, what are the existing methods for preparations of emulsions and how to make simple emulsions. 1.2 Background of This Report Emulsion is a kind of mixture comprised of two or more liquids, which usually are immiscible, and surfactant. The common types of emulsions are oil-in-water emulsion and water-in-oil emulsion. According to Aronson (1988), the emulsions have important industrial value in the wide range of field and it has been studied extensively recently. The emulsions play an important role in the industrial production and it has been applied to many fields including food industry, cosmetics industry and pharmaceutical industry. In the food industry, emulsifier can function as dough conditioners in order to improve tolerance to variations in flour and other ingredient quality. In the cosmetic industry, the majority of facial creams and lotions are emulsions. 1.3 Scope of This Report 3 This report is going to cover the following contents. Introduction of emulsions. Effect of surfactant. Common materials for preparation of emulsions. -

Pharmacology – Inhalant Anesthetics
Pharmacology- Inhalant Anesthetics Lyon Lee DVM PhD DACVA Introduction • Maintenance of general anesthesia is primarily carried out using inhalation anesthetics, although intravenous anesthetics may be used for short procedures. • Inhalation anesthetics provide quicker changes of anesthetic depth than injectable anesthetics, and reversal of central nervous depression is more readily achieved, explaining for its popularity in prolonged anesthesia (less risk of overdosing, less accumulation and quicker recovery) (see table 1) Table 1. Comparison of inhalant and injectable anesthetics Inhalant Technique Injectable Technique Expensive Equipment Cheap (needles, syringes) Patent Airway and high O2 Not necessarily Better control of anesthetic depth Once given, suffer the consequences Ease of elimination (ventilation) Only through metabolism & Excretion Pollution No • Commonly administered inhalant anesthetics include volatile liquids such as isoflurane, halothane, sevoflurane and desflurane, and inorganic gas, nitrous oxide (N2O). Except N2O, these volatile anesthetics are chemically ‘halogenated hydrocarbons’ and all are closely related. • Physical characteristics of volatile anesthetics govern their clinical effects and practicality associated with their use. Table 2. Physical characteristics of some volatile anesthetic agents. (MAC is for man) Name partition coefficient. boiling point MAC % blood /gas oil/gas (deg=C) Nitrous oxide 0.47 1.4 -89 105 Cyclopropane 0.55 11.5 -34 9.2 Halothane 2.4 220 50.2 0.75 Methoxyflurane 11.0 950 104.7 0.2 Enflurane 1.9 98 56.5 1.68 Isoflurane 1.4 97 48.5 1.15 Sevoflurane 0.6 53 58.5 2.5 Desflurane 0.42 18.7 25 5.72 Diethyl ether 12 65 34.6 1.92 Chloroform 8 400 61.2 0.77 Trichloroethylene 9 714 86.7 0.23 • The volatile anesthetics are administered as vapors after their evaporization in devices known as vaporizers. -

Int. J. Environ. Res. Public Health
Int. J. Environ. Res. Public Health 2015, 12, 9988-10008; doi:10.3390/ijerph120809988 OPEN ACCESS International Journal of Environmental Research and Public Health ISSN 1660-4601 www.mdpi.com/journal/ijerph Review E-Cigarettes: A Review of New Trends in Cannabis Use Christian Giroud 1,2,3,*, Mariangela de Cesare 4, Aurélie Berthet 2,3,6, Vincent Varlet 1,2,3, Nicolas Concha-Lozano 2,3,6 and Bernard Favrat 2,3,5,7 1 Forensic Toxicology and Chemistry Unit, University Center of Legal Medicine (CURML), CH-1000 Lausanne 25, Switzerland; E-Mail: [email protected] 2 Department of Community Medicine and Health (DUMSC), Rue du Bugnon 44, CH-1011 Lausanne, Switzerland; E-Mails: [email protected] (A.B.); [email protected] (N.C.-L.); [email protected] (B.F.) 3 Lausanne University Hospital (CHUV), Rue du Bugnon 46, CH-1011, Lausanne, Switzerland 4 Unità di Medicina e Psicologia del Traffico, via Trevano 4, Casella postale 4044, CH-6904 Lugano, Switzerland; E-Mail: [email protected] 5 Unit of Traffic Medicine and Psychology, CURML, CH-1005 Lausanne, Switzerland 6 Institute for Work and Health (IST), Route de la Corniche 2, CH-1066 Epalinges - Lausanne, University of Lausanne and Geneva, Switzerland 7 Center of General Medicine, Department of Ambulatory Care and Community Medicine (PMU), University of Lausanne, Rue du Bugnon 44, CH-1011 Lausanne, Switzerland * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +41(0)-79-556-58-91; Fax: +41(0)-21-314-70-90. Academic Editor: Paul B. -

Grade 6 Science Mechanical Mixtures Suspensions
Grade 6 Science Week of November 16 – November 20 Heterogeneous Mixtures Mechanical Mixtures Mechanical mixtures have two or more particle types that are not mixed evenly and can be seen as different kinds of matter in the mixture. Obvious examples of mechanical mixtures are chocolate chip cookies, granola and pepperoni pizza. Less obvious examples might be beach sand (various minerals, shells, bacteria, plankton, seaweed and much more) or concrete (sand gravel, cement, water). Mechanical mixtures are all around you all the time. Can you identify any more right now? Suspensions Suspensions are mixtures that have solid or liquid particles scattered around in a liquid or gas. Common examples of suspensions are raw milk, salad dressing, fresh squeezed orange juice and muddy water. If left undisturbed the solids or liquids that are in the suspension may settle out and form layers. You may have seen this layering in salad dressing that you need to shake up before using them. After a rain fall the more dense particles in a mud puddle may settle to the bottom. Milk that is fresh from the cow will naturally separate with the cream rising to the top. Homogenization breaks up the fat molecules of the cream into particles small enough to stay suspended and this stable mixture is now a colloid. We will look at colloids next. Solution, Suspension, and Colloid: https://youtu.be/XEAiLm2zuvc Colloids Colloids: https://youtu.be/MPortFIqgbo Colloids are two phase mixtures. Having two phases means colloids have particles of a solid, liquid or gas dispersed in a continuous phase of another solid, liquid, or gas. -

Minty Mouthwash Launched
MARKETPLACE 2D LINGUAL Marketplace is provided as a service to readers using text and images from the manufacturer, supplier or distributor and does not imply endorsement by ORTHODONTICS Vital. Normal and prudent research should be exercised before purchase or Non-visible lingual braces have been available use of any product mentioned. for some time but despite the obvious aesthetic advantages for the wearer, ease of use, cost effec- tiveness and patient comfort have all been cited GIVE YOUR SURGERY Three pre-set positions, back and base as drawbacks by dentists and orthodontists. movements are operated by foot control thus A new 2D system by Forestadent has round A MODERN LOOK eliminating a cross infection risk. The seamless edges and smooth surfaces, allowing free- Not everyone wants to purchase a complete upholstery also benefi ts cross infection dom of movement for the tongue – enabling Treatment Centre when sometimes it’s only the control, providing no available hiding places patients to eat and speak without impairment chair that needs replacing. Takara Belmont’s Pro for bacteria, ensuring optimum hygiene. If your almost immediately after the appliance has been II chair can be sold independently of the Cleo chair is starting to date your surgery call Takara inserted. The self ligating brackets feature a ver- treatment centre and has some unique benefi ts. Belmont on 020 7515 0333 or email tical slot for quick and easy archwire insertion. The folding leg rest gives the chair a modern [email protected]. Alternatively, In addition, the 2D bracket, which has a look that is also extremely practical; its com- all products are available to view total thickness of 1.3 mm to 1.65 mm, can be pact size makes surgeries look less cramped and at either of Belmont’s showrooms bonded directly or indirectly and its clips have the design is a lot less intimidating for patients located in London (020 7515 0333) been designed to open and close easily. -

Novel Liposomes for Targeted Delivery of Drugs and Plasmids
Brigham Young University BYU ScholarsArchive Theses and Dissertations 2013-11-15 Novel Liposomes for Targeted Delivery of Drugs and Plasmids Marjan Javadi Brigham Young University - Provo Follow this and additional works at: https://scholarsarchive.byu.edu/etd Part of the Chemical Engineering Commons BYU ScholarsArchive Citation Javadi, Marjan, "Novel Liposomes for Targeted Delivery of Drugs and Plasmids" (2013). Theses and Dissertations. 3879. https://scholarsarchive.byu.edu/etd/3879 This Dissertation is brought to you for free and open access by BYU ScholarsArchive. It has been accepted for inclusion in Theses and Dissertations by an authorized administrator of BYU ScholarsArchive. For more information, please contact [email protected], [email protected]. Novel Liposomes for Targeted Delivery of Drugs and Plasmids Marjan Javadi A dissertation submitted to the faculty of Brigham Young University in partial fulfillment of the requirements for the degree of Doctor of Philosophy William G. Pitt, Chair Morris D. Argyle Brad C. Bundy Alonzo D. Cook Randy S. Lewis Department of Chemical Engineering Brigham Young University November 2013 Copyright © 2013 Marjan Javadi All Rights Reserved ABSTRACT Novel Liposomes for Targeted Delivery of Drugs and Plasmids Marjan Javadi Department of Chemical Engineering, BYU Doctor of Philosophy People receiving chemotherapy not only suffer from side effects of therapeutics but also must buy expensive drugs. Targeted drug and gene delivery directed to specific tumor-cells is one way to reduce the side effect of drugs and use less amount of therapeutics. In this research, two novel liposomal nanocarriers were developed. This nanocarrier, called an eLiposome, is basically one or more emulsion droplets inside a liposome. -

Emulsion and It's Applications in Food Processing
Adheeb Usaid A.S et al Int. Journal of Engineering Research and Applications www.ijera.com ISSN : 2248-9622, Vol. 4, Issue 4( Version 1), April 2014, pp.241-248 RESEARCH ARTICLE OPEN ACCESS Emulsion and it’s Applications in Food Processing – A Review Adheeb Usaid A.S1, Premkumar.J2 and T.V.Ranganathan3 1.Bachelor of Engineering, 2.Research Scholar, 3. Professor Department of Food Processing and Engineering School of Biotechnology and Health Sciences, Karunya University, Coimbatore-641114, Tamilnadu, India. ABSTRACT An emulsion is a heterogeneous system consisting of atleast one immiscible liquid dispersed in another in the form of droplets. Emulsions are classified based on the nature of the emulsifier or the structure of the system. The range of droplets size for each type of emulsion is quite arbitrary. Macro emulsions are the most common form of emulsions used in food industries than nano and micro emulsions. There are several methods are possible and a wide range of equipments are available for emulsion formations. These methods include shaking, stirring and injection, and the use of colloid mills, homogenizers and ultrasonics. The unique nature of emulsions with a narrow size distribution of different sized droplets has number of applications in food industries including bakery products, dairy, candy products, meat products and beverages. Still most applications are waiting for commercial exploitation. Key words: Applications, Colloid mills, Emulsions, Homogenizers, Ulrasonics. I. INTRODUCTION The definition of an emulsion has continued function of an emulsifier is to join together oily and to evolve since the 1930s. Becher (1957),developed aqueous phases of an emulsion in a an elaborate definition from several previous authors. -

Pharmacokinetics and Pharmacology of Drugs Used in Children
Drug and Fluid Th erapy SECTION II Pharmacokinetics and Pharmacology of Drugs Used CHAPTER 6 in Children Charles J. Coté, Jerrold Lerman, Robert M. Ward, Ralph A. Lugo, and Nishan Goudsouzian Drug Distribution Propofol Protein Binding Ketamine Body Composition Etomidate Metabolism and Excretion Muscle Relaxants Hepatic Blood Flow Succinylcholine Renal Excretion Intermediate-Acting Nondepolarizing Relaxants Pharmacokinetic Principles and Calculations Atracurium First-Order Kinetics Cisatracurium Half-Life Vecuronium First-Order Single-Compartment Kinetics Rocuronium First-Order Multiple-Compartment Kinetics Clinical Implications When Using Short- and Zero-Order Kinetics Intermediate-Acting Relaxants Apparent Volume of Distribution Long-Acting Nondepolarizing Relaxants Repetitive Dosing and Drug Accumulation Pancuronium Steady State Antagonism of Muscle Relaxants Loading Dose General Principles Central Nervous System Effects Suggamadex The Drug Approval Process, the Package Insert, and Relaxants in Special Situations Drug Labeling Opioids Inhalation Anesthetic Agents Morphine Physicochemical Properties Meperidine Pharmacokinetics of Inhaled Anesthetics Hydromorphone Pharmacodynamics of Inhaled Anesthetics Oxycodone Clinical Effects Methadone Nitrous Oxide Fentanyl Environmental Impact Alfentanil Oxygen Sufentanil Intravenous Anesthetic Agents Remifentanil Barbiturates Butorphanol and Nalbuphine 89 A Practice of Anesthesia for Infants and Children Codeine Antiemetics Tramadol Metoclopramide Nonsteroidal Anti-infl ammatory Agents 5-Hydroxytryptamine -

Drug Vaping Applied to Cannabis: Is “Cannavaping”
www.nature.com/scientificreports OPEN Drug vaping applied to cannabis: Is “Cannavaping” a therapeutic alternative to marijuana? Received: 26 January 2016 Vincent Varlet1, Nicolas Concha-Lozano2, Aurélie Berthet2, Grégory Plateel2, Accepted: 19 April 2016 Bernard Favrat3,4, Mariangela De Cesare3, Estelle Lauer1, Marc Augsburger1, Published: 26 May 2016 Aurélien Thomas1,5 & Christian Giroud1 Therapeutic cannabis administration is increasingly used in Western countries due to its positive role in several pathologies. Dronabinol or tetrahydrocannabinol (THC) pills, ethanolic cannabis tinctures, oromucosal sprays or table vaporizing devices are available but other cannabinoids forms can be used. Inspired by the illegal practice of dabbing of butane hashish oil (BHO), cannabinoids from cannabis were extracted with butane gas, and the resulting concentrate (BHO) was atomized with specific vaporizing devices. The efficiency of “cannavaping,” defined as the “vaping” of liquid refills for e-cigarettes enriched with cannabinoids, including BHO, was studied as an alternative route of administration for therapeutic cannabinoids. The results showed that illegal cannavaping would be subjected to marginal development due to the poor solubility of BHO in commercial liquid refills (especially those with high glycerin content). This prevents the manufacture of liquid refills with high BHO concentrations adopted by most recreational users of cannabis to feel the psychoactive effects more rapidly and extensively. Conversely, “therapeutic cannavaping” could be an efficient route for cannabinoids administration because less concentrated cannabinoids-enriched liquid refills are required. However, the electronic device marketed for therapeutic cannavaping should be carefully designed to minimize potential overheating and contaminant generation. The creativity of cannabis users leads to new methods of consumption. -
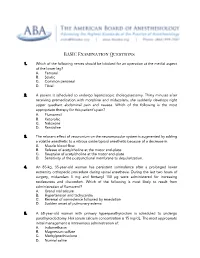
BASIC Examination Questions with Answer
BASIC Examination Questions 1. Which of the following nerves should be blocked for an operation at the medial aspect of the lower leg? A. Femoral B. Sciatic C. Common peroneal D. Tibial 2. A patient is scheduled to undergo laparoscopic cholecystectomy. Thirty minutes after receiving premedication with morphine and midazolam, she suddenly develops right upper quadrant abdominal pain and nausea. Which of the following is the most appropriate therapy for this patient’s pain? A. Flumazenil B. Ketorolac C. Naloxone D. Ranitidine 3. The relaxant effect of vecuronium on the neuromuscular system is augmented by adding a volatile anesthetic to a nitrous oxide/opioid anesthetic because of a decrease in: A. Muscle blood flow. B. Release of acetylcholine at the motor end-plate. C. Reuptake of acetylcholine at the motor end-plate. D. Sensitivity of the postjunctional membrane to depolarization. 4. An 85-kg, 35-year-old woman has persistent somnolence after a prolonged lower extremity orthopedic procedure during spinal anesthesia. During the last two hours of surgery, midazolam 5 mg and fentanyl 150 µg were administered for increasing restlessness and discomfort. Which of the following is most likely to result from administration of flumazenil? A. Grand mal seizure B. Hypertension and tachycardia C. Reversal of somnolence followed by resedation D. Sudden onset of pulmonary edema 5. A 68-year-old woman with primary hyperparathyroidism is scheduled to undergo parathyroidectomy. Her serum calcium concentration is 15 mg/dL. The most appropriate initial management is intravenous administration of: A. Indomethacin B. Magnesium sulfate C. Methylprednisolone D. Normal saline 6. Which of the following tests most reliably predicts the likelihood that a patient will develop malignant hyperthermia? A.