Satisfied Result of Modified Knapp Procedure for a Rare Case of Isolated Superior Rectus Muscle Rupture: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Atlas of the Facial Nerve and Related Structures
Rhoton Yoshioka Atlas of the Facial Nerve Unique Atlas Opens Window and Related Structures Into Facial Nerve Anatomy… Atlas of the Facial Nerve and Related Structures and Related Nerve Facial of the Atlas “His meticulous methods of anatomical dissection and microsurgical techniques helped transform the primitive specialty of neurosurgery into the magnificent surgical discipline that it is today.”— Nobutaka Yoshioka American Association of Neurological Surgeons. Albert L. Rhoton, Jr. Nobutaka Yoshioka, MD, PhD and Albert L. Rhoton, Jr., MD have created an anatomical atlas of astounding precision. An unparalleled teaching tool, this atlas opens a unique window into the anatomical intricacies of complex facial nerves and related structures. An internationally renowned author, educator, brain anatomist, and neurosurgeon, Dr. Rhoton is regarded by colleagues as one of the fathers of modern microscopic neurosurgery. Dr. Yoshioka, an esteemed craniofacial reconstructive surgeon in Japan, mastered this precise dissection technique while undertaking a fellowship at Dr. Rhoton’s microanatomy lab, writing in the preface that within such precision images lies potential for surgical innovation. Special Features • Exquisite color photographs, prepared from carefully dissected latex injected cadavers, reveal anatomy layer by layer with remarkable detail and clarity • An added highlight, 3-D versions of these extraordinary images, are available online in the Thieme MediaCenter • Major sections include intracranial region and skull, upper facial and midfacial region, and lower facial and posterolateral neck region Organized by region, each layered dissection elucidates specific nerves and structures with pinpoint accuracy, providing the clinician with in-depth anatomical insights. Precise clinical explanations accompany each photograph. In tandem, the images and text provide an excellent foundation for understanding the nerves and structures impacted by neurosurgical-related pathologies as well as other conditions and injuries. -

Anatomy of the Periorbital Region Review Article Anatomia Da Região Periorbital
RevSurgicalV5N3Inglês_RevistaSurgical&CosmeticDermatol 21/01/14 17:54 Página 245 245 Anatomy of the periorbital region Review article Anatomia da região periorbital Authors: Eliandre Costa Palermo1 ABSTRACT A careful study of the anatomy of the orbit is very important for dermatologists, even for those who do not perform major surgical procedures. This is due to the high complexity of the structures involved in the dermatological procedures performed in this region. A 1 Dermatologist Physician, Lato sensu post- detailed knowledge of facial anatomy is what differentiates a qualified professional— graduate diploma in Dermatologic Surgery from the Faculdade de Medician whether in performing minimally invasive procedures (such as botulinum toxin and der- do ABC - Santo André (SP), Brazil mal fillings) or in conducting excisions of skin lesions—thereby avoiding complications and ensuring the best results, both aesthetically and correctively. The present review article focuses on the anatomy of the orbit and palpebral region and on the important structures related to the execution of dermatological procedures. Keywords: eyelids; anatomy; skin. RESU MO Um estudo cuidadoso da anatomia da órbita é muito importante para os dermatologistas, mesmo para os que não realizam grandes procedimentos cirúrgicos, devido à elevada complexidade de estruturas envolvidas nos procedimentos dermatológicos realizados nesta região. O conhecimento detalhado da anatomia facial é o que diferencia o profissional qualificado, seja na realização de procedimentos mini- mamente invasivos, como toxina botulínica e preenchimentos, seja nas exéreses de lesões dermatoló- Correspondence: Dr. Eliandre Costa Palermo gicas, evitando complicações e assegurando os melhores resultados, tanto estéticos quanto corretivos. Av. São Gualter, 615 Trataremos neste artigo da revisão da anatomia da região órbito-palpebral e das estruturas importan- Cep: 05455 000 Alto de Pinheiros—São tes correlacionadas à realização dos procedimentos dermatológicos. -

Double-Bellied Superior Rectus Muscle
Surgical and Radiologic Anatomy (2019) 41:713–715 https://doi.org/10.1007/s00276-019-02211-0 ANATOMIC VARIATIONS Double-bellied superior rectus muscle Satheesha B. Nayak1 · Surekha D. Shetty1 · Naveen Kumar1 · Ashwini P. Aithal1 Received: 3 September 2018 / Accepted: 23 February 2019 / Published online: 7 March 2019 © Springer-Verlag France SAS, part of Springer Nature 2019 Abstract Congenital variations of extraocular muscles are rare. We report a double-bellied superior rectus muscle, observed in an adult male cadaver aged 70 years. The superior rectus muscle had two equal-sized bellies, which took separate origins from the common tendinous ring and united to form a common belly 1 cm before the insertion. Due to the duplication, the muscle extended laterally beyond the levator palpebrae superioris. Both its bellies were supplied by oculomotor nerve. To the best of our knowledge, this is the first report on doubling of the belly of the superior rectus muscle. Keywords Extraocular · Orbit · Superior rectus muscle · Eye movement · Strabismus Introduction Case report Voluntary movements of the eyeball are performed by six During dissection classes for the first-year medical students, extraocular muscles, namely superior rectus muscle, the we observed a unique variation in the right orbit of an adult inferior rectus muscle, medial rectus muscle, lateral rectus male cadaver aged 70 years. The cadaver was donated to the muscle, superior oblique muscle, and inferior oblique mus- department for teaching and research purpose. No history of cles. Variations of these muscles can result in restrictions of strabismus or visual defects is available. The variation was movements of eyeball, causing strabismus. -

SŁOWNIK ANATOMICZNY (ANGIELSKO–Łacinsłownik Anatomiczny (Angielsko-Łacińsko-Polski)´ SKO–POLSKI)
ANATOMY WORDS (ENGLISH–LATIN–POLISH) SŁOWNIK ANATOMICZNY (ANGIELSKO–ŁACINSłownik anatomiczny (angielsko-łacińsko-polski)´ SKO–POLSKI) English – Je˛zyk angielski Latin – Łacina Polish – Je˛zyk polski Arteries – Te˛tnice accessory obturator artery arteria obturatoria accessoria tętnica zasłonowa dodatkowa acetabular branch ramus acetabularis gałąź panewkowa anterior basal segmental artery arteria segmentalis basalis anterior pulmonis tętnica segmentowa podstawna przednia (dextri et sinistri) płuca (prawego i lewego) anterior cecal artery arteria caecalis anterior tętnica kątnicza przednia anterior cerebral artery arteria cerebri anterior tętnica przednia mózgu anterior choroidal artery arteria choroidea anterior tętnica naczyniówkowa przednia anterior ciliary arteries arteriae ciliares anteriores tętnice rzęskowe przednie anterior circumflex humeral artery arteria circumflexa humeri anterior tętnica okalająca ramię przednia anterior communicating artery arteria communicans anterior tętnica łącząca przednia anterior conjunctival artery arteria conjunctivalis anterior tętnica spojówkowa przednia anterior ethmoidal artery arteria ethmoidalis anterior tętnica sitowa przednia anterior inferior cerebellar artery arteria anterior inferior cerebelli tętnica dolna przednia móżdżku anterior interosseous artery arteria interossea anterior tętnica międzykostna przednia anterior labial branches of deep external rami labiales anteriores arteriae pudendae gałęzie wargowe przednie tętnicy sromowej pudendal artery externae profundae zewnętrznej głębokiej -

A- and V-Patterns and Oblique Muscle Overaction A- and V-Patterns
18 A- and V-Patterns and Oblique Muscle Overaction A- and V-Patterns Clinical Features Etiology Management with Horizontal Rectus Muscle Offsets Inferior Oblique Overaction Etiology Clinical Features Differential Diagnosis Management Superior Oblique Overaction Etiology Clinical Features Differential Diagnosis Management Superior Oblique Weakening Procedures Complications A- and V-patterns of strabismus are changes in the horizontal deviation as the patient looks up and down. They are usually associated with oblique dysfunction, either overaction or paresis. Primary oblique muscle overaction is when an oblique muscle is too strong for its antagonist and there is no known cause. Secondary oblique overaction is caused by a paresis of the antagonist muscle. A superior oblique paresis results in inferior oblique overaction, and inferior oblique paresis results in superior oblique overaction. This chapter covers the management of A- and V- patterns and primary oblique muscle overaction. A- and V-Patterns CLINICAL FEATURES A-patterns are defined as increasing divergence in down gaze (>10 prism diopters [PD]), whereas Vpatterns are increased divergence (>15 prism diopters) in up gaze. The type of A- or V-pattern helps identify the cause. Superior oblique paresis produces a V-pattern, arrow subtype, with convergence in down gaze. The arrow pattern subtype indicates a lack of abduction in down gaze, the field of action of the superior oblique muscles. Inferior oblique overaction, on the other hand, has a V-pattern, Y subtype, with increased abduction in up gaze. The Y-pattern occurs because the field of action of the inferior oblique muscles is up gaze and they are abductors. Lambda subtype is typically associated with superior oblique overaction, with increased abduction in down gaze, because the field of action is in down gaze. -

Atlas of Topographical and Pathotopographical Anatomy of The
Contents Cover Title page Copyright page About the Author Introduction Part 1: The Head Topographic Anatomy of the Head Cerebral Cranium Basis Cranii Interna The Brain Surgical Anatomy of Congenital Disorders Pathotopography of the Cerebral Part of the Head Facial Head Region The Lymphatic System of the Head Congenital Face Disorders Pathotopography of Facial Part of the Head Part 2: The Neck Topographic Anatomy of the Neck Fasciae, Superficial and Deep Cellular Spaces and their Relationship with Spaces Adjacent Regions (Fig. 37) Reflex Zones Triangles of the Neck Organs of the Neck (Fig. 50–51) Pathography of the Neck Topography of the neck Appendix A Appendix B End User License Agreement Guide 1. Cover 2. Copyright 3. Contents 4. Begin Reading List of Illustrations Chapter 1 Figure 1 Vessels and nerves of the head. Figure 2 Layers of the frontal-parietal-occipital area. Figure 3 Regio temporalis. Figure 4 Mastoid process with Shipo’s triangle. Figure 5 Inner cranium base. Figure 6 Medial section of head and neck Figure 7 Branches of trigeminal nerve Figure 8 Scheme of head skin innervation. Figure 9 Superficial head formations. Figure 10 Branches of the facial nerve Figure 11 Cerebral vessels. MRI. Figure 12 Cerebral vessels. Figure 13 Dural venous sinuses Figure 14 Dural venous sinuses. MRI. Figure 15 Dural venous sinuses Figure 16 Venous sinuses of the dura mater Figure 17 Bleeding in the brain due to rupture of the aneurism Figure 18 Types of intracranial hemorrhage Figure 19 Different types of brain hematomas Figure 20 Orbital muscles, vessels and nerves. Topdown view, Figure 21 Orbital muscles, vessels and nerves. -

Differences in Extrinsic Eye Muscles and Dissection Protocols
Iowa State University Capstones, Theses and Creative Components Dissertations Spring 2020 Comparative anatomy case study: differences in extrinsic eye muscles and dissection protocols Erin Ruden Follow this and additional works at: https://lib.dr.iastate.edu/creativecomponents Part of the Animal Structures Commons, and the Body Regions Commons Recommended Citation Ruden, Erin, "Comparative anatomy case study: differences in extrinsic eye muscles and dissection protocols" (2020). Creative Components. 543. https://lib.dr.iastate.edu/creativecomponents/543 This Creative Component is brought to you for free and open access by the Iowa State University Capstones, Theses and Dissertations at Iowa State University Digital Repository. It has been accepted for inclusion in Creative Components by an authorized administrator of Iowa State University Digital Repository. For more information, please contact [email protected]. P a g e | 1 Comparative anatomy case study: differences in extrinsic eye muscles and dissection protocols Abstract: There have been notable studies comparing the eye placement between predators and prey, which can be further categorized as omnivore, carnivore, and herbivore. The purpose of this study was to determine if eye placement correlated with extrinsic eye muscle differences among the classification of animals (predator vs. prey and omnivore vs. carnivore vs. herbivore). For an omnivore, a human orbit was dissected. A cat was dissected to represent a carnivore and a goat was dissected to represent an herbivore. Dissection protocol for the cat and goat were created due to the lack of dissections of these muscles. Unfortunately, data collection was incomplete due to the social distancing policy on Iowa State University’s campus because of COVID-19. -
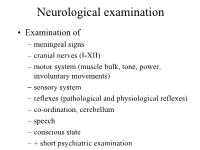
Neurological Examination
Neurological examination • Examination of – meningeal signs – cranial nerves (I-XII) – motor system (muscle bulk, tone, power, involuntary movements) – sensory system – reflexes (pathological and physiological reflexes) – co-ordination, cerebellum – speech – conscious state – + short psychiatric examination MENINGEAL SIGNS • may be caused by: – meningitis (bacterial or viral infection of meninges) – blood in the subarachnoidal space – infiltration of meninges by carcinoma cells – increased intracranial pressure – dehydration Optic nerve (II) Visual acuity Visual field Fundus - Optic disc • Retina • Optic nerve • Chiasm • Optic tract • Lateral geniculate body • Optic radiation • Visual (occipital) cortex VISUAL FIELD - LENS - reversed image 1. The lens produces reversed image 2. Fibers, originating from the upper part of the retina keeps their superior/upper position through the whole optic pathway Visual field Oculomotor (III), trochlear (IV), and abducent (VI) nerves • Oculomotor nerve (III) innervates: medial rectus, superior rectus, inferior rectus, inferior oblique muscles + superior palpebral levator muscle, ciliary muscle, pupillary constrictor muscle • Trochlear nerve (IV) innervates: superior oblique muscle • Abducent nerve (VI) innervates: lateral rectus muscle Nuclei of culomotor (III), trochlear (IV), and abducent (VI) nerves • Oculomotor nerve – Main nucleus (mesencephalon) of oculomotor nerve controls medial rectus, superior rectus, inferior rectus, inferior oblique muscles + superior palpebral levator muscle – Edinger-Westphal -

FIPAT-TA2-Part-2.Pdf
TERMINOLOGIA ANATOMICA Second Edition (2.06) International Anatomical Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TA2, PART II Contents: Systemata musculoskeletalia Musculoskeletal systems Caput II: Ossa Chapter 2: Bones Caput III: Juncturae Chapter 3: Joints Caput IV: Systema musculare Chapter 4: Muscular system Bibliographic Reference Citation: FIPAT. Terminologia Anatomica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, 2019 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Anatomica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput II: OSSA Chapter 2: BONES Latin term Latin synonym UK English US English English synonym Other 351 Systemata Musculoskeletal Musculoskeletal musculoskeletalia systems systems -

High-Resolution Magnetic Resonance Imaging of the Normal Extraocular Musculature
HIGH-RESOLUTION MAGNETIC RESONANCE IMAGING OF THE NORMAL EXTRAOCULAR MUSCULATURE l 2 3 4 2 A. ETTL , J. KRAMER, A. DAXER and L. KOORNNEEF St Patten, Linz and Innsbruck, Austria and Amsterdam, The Netherlands SUMMARY Magnetic resonance imaging (MRI) is a good method for evaluating extraocular muscle disorders.l Purpose: Magnetic resonance imaging (MRI) of the Most pUblications focus on MRI of orbital disease,1 extraocular muscles has attracted growing interest for but do not provide enough information on normal the evaluation of complex motility disorders. However, orbital imaging anatomy. Since the early anatomical little information is available on the high-resolution MRI studies of the orbit,2 advanced MRI technology MRI anatomy of the normal extraocular muscles and has led to a marked improvement in the resolution of their connective tissue system. The study describes the orbital MR images, although motion artifacts still imaging anatomy of the recti and oblique muscles and represent a significant problem. The present study the levator palpebrae superioris muscle. was performed to describe the MRI anatomy of the Methods: MRI of the orbit at 1 tesla was performed in normal extraocular muscles under resting conditions four normal volunteers using a surface coil. in vivo. Results: Many anatomical details such as Zinn's tendinous annulus, the trochlea, the superior oblique MATERIALS AND METHODS tendon, the intermuscular septa, the check ligaments, Six orbits from four normal volunteers aged from 26 Lockwood's ligament and the common sheath between to 32 years were examined. MRI was performed the superior rectus muscle and the levator muscle were using a 1 tesla scanner (Impact, Siemens, Germany) visualised. -

Abnormal Insertion of the Inferior Oblique Muscle Is Rare
Dohvoma VA, et al., J Ophthalmic Clin Res 2019, 6: 061 DOI: 10.24966/OCR-8887/100061 HSOA Journal of Ophthalmology & Clinical Research Case Report There was no under-action or over-¬action of any muscle, includ- Abnormal Insertion of the ing the inferior oblique. The right eye was the fixating eye. Under general anesthesia, the position of the fixating eye was unchanged, Inferior Oblique Muscle: A while the non-fixating eye showed less divergence. Unilateral re- cess-resect procedure on the no-fixating eye was our carried out. A 7 Report of 2 Cases mm medial rectus resection was done through a limbal incision. The lateral rectus muscle was also approached by a limbal incision. After Dohvoma VA1,2*, Ebana Mvogo SR1, Mvilongo TC2, Chilla F2 dissection, a thick fleshy tendon was hooked (Figure 2). Full-thick- 1,2 and Ebana Mvogo C ness bites were passed at the edges to secure the muscle. The muscle 1Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, was cut close to the insertion. An anomalous insertion of the inferior Cameroon oblique muscle was noticed along an oblique line (upward and back- 2Yaoundé Central Hospital, Yaoundé, Cameroon ward), just beneath the lateral rectus muscle with partial fusion to the inferior border of the lateral muscle tendon. No other belly was found upon careful examination of the inferior temporal quadrant. The infe- rior oblique muscle was secured and cut, to allow for the lateral rectus Abstract to be recessed. A 10mm recession of the lateral rectus was done. The Abnormal insertion of the inferior oblique muscle is rare. -

Primary Oblique Muscle Overaction the Brain Throws a Wild Pitch
CLINICAL SCIENCES Primary Oblique Muscle Overaction The Brain Throws a Wild Pitch Michael C. Brodsky, MD; Sean P. Donahue, MD, PhD Background: Sensorimotor and orbital anatomical inferior oblique overaction, which corresponds to a for- mechanisms have been invoked to explain primary ob- ward pitch in lateral-eyed animals, may result from vi- lique muscle overaction. sual disinhibition of central vestibular pathways to the extraocular muscle subnuclei that modulate upward ex- Methods: Review of primitive visuo-vestibular re- traocular muscle tonus. flexes and neuroanatomical pathways corresponding to vestibulo-ocular reflexes, and correlation with known Conclusions: Primary oblique muscle overaction reca- clinical abnormalities in patients with primary oblique pitulates the torsional eye movements that occur in lateral- muscle overaction. eyed animals during body movements or directional lu- minance shifts in the pitch plane. These primitive ocular Results: Bilateral superior oblique muscle overaction, motor reflexes become manifest in humans when early- which corresponds to a backward pitch in lateral-eyed onset strabismus or structural lesions within the poste- animals, can occur when structural lesions involving the rior fossa alter central vestibular tone in the pitch plane. brainstem or cerebellum increase central otolithic input to the extraocular muscle subnuclei that modu- late downward extraocular muscle tonus. Bilateral Arch Ophthalmol. 2001;119:1307-1314 RIMARY oblique muscle over- tropia but no other overt neurologic ab- action is a common ocular normalities. Surgical weakening of the motility disorder character- overacting oblique muscles improves ver- ized by vertical incomitance sions, eliminates the associated A or V pat- of the eyes in lateral gaze.1 In tern, and reduces torsion.