The Five Diaphragms in Osteopathic Manipulative Medicine: Myofascial Relationships, Part 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Gross Anatomy ABDOMEN/SESSION 4 Dr. Firas M. Ghazi Posterior
Gross Anatomy ABDOMEN/SESSION 4 Dr. Firas M. Ghazi Posterior Abdominal Wall and the Diaphragm PAW : Posterior Abdominal Wall Curricular Objectives By the end of this session students are expected to: Practical 1. Identify the bones forming the PAW and their main markings 2. Distinguish the muscles forming the PAW and their fascial coverings 3. Trace the nerves of the PAW to their terminations 4. Identify the diaphragm and discriminate structures arising from its vertebral origin 5. Locate the major foramina of the diaphragm and the structures they transmit 6. Identify the retroperitoneal organs related to PAW Theory 1. State the framework of PAW 2. Name the bones forming the PAW and describe their main markings 3. Outline the muscles forming the PAW, their attachment and actions 4. Define the para-vertebral gutter and list the retroperitoneal organs related to it 5. Acknowledge the close relation of abdominal aorta to AAW 6. List the nerves related to PAW and their main distribution 7. Review the cremasteric reflex and acknowledge its physiological importance 8. Recall the patellar reflex and follow its pathway 9. Recall the attachment of the diaphragm and describe its vertebral origin 10. Underline the major foramina of the diaphragm and the structures they transmit 11. Review the innervation of diaphragm and the possible sites of referred pain 12. Summarize the fascial and peritoneal linings of the abdominal cavity Selected references and suggested resources Clinical Anatomy by Regions, Richard S. Snell, 9th edition Grant's Atlas of Anatomy, 13th Edition McMinn's Clinical Atlas of Human Anatomy, 7th Edition Anatomy for Babylon medical students (facebook page) Human Anatomy Education (facebook page) Human anatomy education (you tube channel) This session has been reviewed by Anatomy team at the Department of Anatomy and Histology/ College of Medicine/ University of Babylon/ 2016 Session check list Clinical importance Irritation of peritoneum on PAW can stimulate the related nerves and result in characteristic clinical manifestations. -
The Muscular System Views
1 PRE-LAB EXERCISES Before coming to lab, get familiar with a few muscle groups we’ll be exploring during lab. Using Visible Body’s Human Anatomy Atlas, go to the Views section. Under Systems, scroll down to the Muscular System views. Select the view Expression and find the following muscles. When you select a muscle, note the book icon in the content box. Selecting this icon allows you to read the muscle’s definition. 1. Occipitofrontalis (epicranius) 2. Orbicularis oculi 3. Orbicularis oris 4. Nasalis 5. Zygomaticus major Return to Muscular System views, select the view Head Rotation and find the following muscles. 1. Sternocleidomastoid 2. Scalene group (anterior, middle, posterior) 2 IN-LAB EXERCISES Use the following modules to guide your exploration of the head and neck region of the muscular system. As you explore the modules, locate the muscles on any charts, models, or specimen available. Please note that these muscles act on the head and neck – those that are located in the neck but act on the back are in a separate section. When reviewing the action of a muscle, it will be helpful to think about where the muscle is located and where the insertion is. Muscle physiology requires that a muscle will “pull” instead of “push” during contraction, and the insertion is the part that will move. Imagine that the muscle is “pulling” on the bone or tissue it is attached to at the insertion. Access 3D views and animated muscle actions in Visible Body’s Human Anatomy Atlas, which will be especially helpful to visualize muscle actions. -

Biology 152 – Brain/Spinal Cord/Ear/Eye Objectives
Biology 152 – Brain/Spinal Cord/Ear/Eye Objectives Items will be identified on a sheep's brain dissection, human brain models, sagittal/coronal sections of human brains in plastic, ear and eye models, and an eye dissection. You will need to learn a proper function for each listed item for the practical. BRAIN REGIONS – learn their names, position in the brain, and functions Meninges – protective tissue layers around the brain and spinal cord Dura mater strong mother, collagenous layer with dural sinuses, protects brain and allows reabsorption of CSF into blood stream Arachnoid arachnoid villi “pooch” into dural sinus to allow CSF loss to blood, holds membrane CSF and allows circulation around brain/spine Pia mater weak mother, holds shape of brain and allows diffusion of nutrients and wastes between tissues and CSF Cerebrum – two hemispheres where all conscious thought occurs L/R Hemispheres dual hard drives that control behavior and store all memory Cerebral cortex thin gray matter (nonmyelinated) layer that stores information Frontal lobe site of voluntary motor control, behavior, and intelligence Parietal lobe site of gustatory (taste) storage, special sense/navigation ability Temporal lobe site of olfactory and auditory memory storage Occipital lobe site of visual memory storage Precentral gyrus primary motor cortex router connecting frontal lobe to muscles Postcentral gyrus primary somatosensory router connecting senses to posterior brain regions Central sulcus low spot in cerebrum dividing all motor from all sensory areas Gyri/sulci -
Pubid-1446077038.Pdf
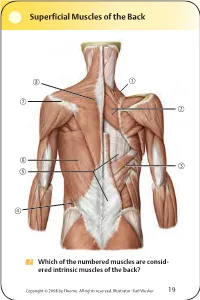
Superficial Muscles of the Back Which of the numbered muscles are consid- ered intrinsic muscles of the back? Copyright © 2008 by Thieme. All rights reserved. Illustrator: Karl Wesker 19 Superficial Muscles of the Back Posterior view. A Levator scapulae S Rhomboideus major D Serratus posterior inferior F Lumbar triangle, internal oblique G Thoracolumbar fascia, superficial layer H Latissimus dorsi J Scapular spine K Trapezius, transverse part Only the serratus posterior inferior is an intrinsic muscle of the back. The trapezius, latissimus dorsi, leva- tor scapulae, and rhomboideus muscles assist in move- ment of the shoulder or arm and are considered muscles of the upper limb. Fig. 2.1. Gilroy, MacPherson, Ross, Atlas of Anatomy, p. 22. Course of the Intercostal Nerves Copyright © 2008 by Thieme. All rights reserved. Illustrator: Markus Voll 39 Course of the Intercostal Nerves Coronal section. Anterior view. A Visceral pleura S Parietal pleura, diaphragmatic part D Diaphragm F Costodiaphragmatic recess G Endothoracic fascia H External intercostal J Costal groove K Intercostal vein, artery, and nerve Abnormal fluid collection in the pleural space (e.g., pleural effusion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the 7th or 8th intercostal space on the posterior axillary line. The drain should always be introduced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve. Fig. 5.24. From Atlas of Anatomy, p. 59. Copyright ©2008 byThieme. Allrightsreserved. Illustrator: Markus Voll Right Lung 74 Right Lung Lateral and medial views. -

Axis Scientific Skull with Muscle Origins and Insertions A-108851
Axis Scientific Skull with Muscle Origins and Insertions A-108851 *Muscle Origins = RED Anterior View Occipital Bone Posterior View *Muscle Insertions = BLUE Posterior Cerebral Artery Frontal Bone Basilar Artery Pontine Arteries Parietal Bone Nasal Bone Temporal Bone Sphenoid Bone Temporalis Parietal Bone Occipitofrontalis Occipital Bone Lacrimal Bone Sternocleidomastoid Trapezius Temporalis Semispinalis Capitis Temporal Bone Corrugator Supercilii Splenius Capitis Longissimus Capitis Orbicularis Oculi Obliquus Capitis Superior Temporal Basilar Artery Bone Procerus Rectis Capitis C1 Posterior Major Vertebral Artery Levator Labii Superioris C2 Alaeque Nasi Rectis Capitis Posterior Minor Sphenoid Levator Labii Superioris Posterior Digastric Zygomatic Bone Bone C3 Nasalis (Transverse Part) Rectis Capitis C4 Masseter Lateralis Spinal Nerve Zygomaticus Major C5 Zygomatic Medial Pterygoid Bone Zygomaticus Minor C6 Temporalis Mylohyoid C7 Mandible Levator Anguli Oris Vomer Nasalis (Alar Part) Spinal Nerve Spinal Cord Maxilla Orbicularis Oris Depressor Septi Nasi Masseter Medial Superior Masseter Mandible Orbicularis Oris Constrictor Pterygoid Inferior View Styloglossus Platysma Mylohyoid Depressor Stylohyoid Anguli Oris Anterior Stylopharyngeus Spinal Nerve Depressor Digastric Labii Inferioris Posterior Geniohyoid Digastric Vertebral Artery Mentalis Rectis Capitis Genioglossus Lateralis Rectis Capitis Buccinator Mandible Posterior Major Rectis Capitis Posterior Minor Frontal Bone Corrugator Supercilii Orbicularis Oculi Lacrimal Bone Depressor -

Questions on Human Anatomy
Standard Medical Text-books. ROBERTS’ PRACTICE OF MEDICINE. The Theory and Practice of Medicine. By Frederick T. Roberts, m.d. Third edi- tion. Octavo. Price, cloth, $6.00; leather, $7.00 Recommended at University of Pennsylvania. Long Island College Hospital, Yale and Harvard Colleges, Bishop’s College, Montreal; Uni- versity of Michigan, and over twenty other medical schools. MEIGS & PEPPER ON CHILDREN. A Practical Treatise on Diseases of Children. By J. Forsyth Meigs, m.d., and William Pepper, m.d. 7th edition. 8vo. Price, cloth, $6.00; leather, $7.00 Recommended at thirty-five of the principal medical colleges in the United States, including Bellevue Hospital, New York, University of Pennsylvania, and Long Island College Hospital. BIDDLE’S MATERIA MEDICA. Materia Medica, for the Use of Students and Physicians. By the late Prof. John B Biddle, m.d., Professor of Materia Medica in Jefferson Medical College, Phila- delphia. The Eighth edition. Octavo. Price, cloth, $4.00 Recommended in colleges in all parts of the UnitedStates. BYFORD ON WOMEN. The Diseases and Accidents Incident to Women. By Wm. H. Byford, m.d., Professor of Obstetrics and Diseases of Women and Children in the Chicago Medical College. Third edition, revised. 164 illus. Price, cloth, $5.00; leather, $6.00 “ Being particularly of use where questions of etiology and general treatment are concerned.”—American Journal of Obstetrics. CAZEAUX’S GREAT WORK ON OBSTETRICS. A practical Text-book on Midwifery. The most complete book now before the profession. Sixth edition, illus. Price, cloth, $6.00 ; leather, $7.00 Recommended at nearly fifty medical schools in the United States. -

The Femoral Hernia: Some Necessary Additions
International Journal of Clinical Medicine, 2014, 5, 752-765 Published Online July 2014 in SciRes. http://www.scirp.org/journal/ijcm http://dx.doi.org/10.4236/ijcm.2014.513102 The Femoral Hernia: Some Necessary Additions Ljubomir S. Kovachev Department of General Surgery, Medical University, Pleven, Bulgaria Email: [email protected] Received 28 April 2014; revised 27 May 2014; accepted 26 June 2014 Copyright © 2014 by author and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Purpose: The anatomic region through which most inguinal hernias emerge is overcrowded by various anatomical structures with intricate relationships. This is reflected by the wide range of anatomic interpretations. Material and Methods: A prospective anatomic study of over 100 fresh cadavers and 47 patients operated on for femoral hernias. Results: It was found that the transver- salis fascia did not continue distally into the lymphatic lacuna. Medially this fascia did not reach the lacunar ligament, but was rather positioned above it forming laterally the vascular sheath. Here the fascia participates in the formation of a fossa, which varies in width and depth—the pre- peritoneal femoral fossa. The results did not confirm the presence of a femoral canal. The dis- tances were measured between the pubic tubercle and the medial margin of the femoral vein, and between the inguinal and the Cooper’s ligaments. The results clearly indicate that in women with femoral hernias these distances are much larger. Along the course of femoral hernia exploration we established the presence of three zones that are rigid and narrow. -

Neuromuscular Organisation of Mammalian Extraocular Muscles
Rapporter fra Høgskolen i Buskerud nr. 36 RAPPORT RAPPORT Neuromuscular organisation of mammalian extraocular muscles Inga-Britt Kjellevold Haugen (M.Phil) Rapporter fra Høgskolen i Buskerud Nr. 36 Neuromuscular organisation of mammalian extraocular muscles Inga-Britt Kjellevold Haugen (M.Phil) Kongsberg 2002 HiBus publikasjoner kan kopieres fritt og videreformidles til andre interesserte uten avgift. En forutsetning er at navn på utgiver og forfatter(e) angis - og angis korrekt. Det må ikke foretas endringer i verket. ISBN 82-91116-52-0 ISSN 0807-4488 2 CONTENTS 1. PREFACE ...................................................................................................................................... 4 2. ACKNOWLEDGEMENT............................................................................................................. 5 3. INTRODUCTION ......................................................................................................................... 6 4. LITERATURE REVIEW OF MAMMALIAN EXTRAOCULAR MUSCLES .................... 10 4.1 MUSCLE HISTOLOGY .................................................................................................................. 14 4.1.1 Ultrastructure and physiology ............................................................................................. 14 4.1.2 Fibre classification and distribution .................................................................................... 21 4.1.3 Motor innervation ............................................................................................................... -

Bilateral Scarpa's Fascia Advancement Flaps to Improve The
Egypt, J. Plast. Reconstr. Surg., Vol. 35, No. 1, January: 133-140, 2011 Bilateral Scarpa’s Fascia Advancement Flaps to Improve the Waistline in Abdominoplasty WAEL M. ELSHAER, M.D.*; SAMEH ELNOAMANI, M.D.** and HOSSAM HOSNI, M.D.** The Department of Plastic and General surgery, Faculty of Medicine, Bani-Suef * and Cairo** Universities. ABSTRACT better sculpting or to hide the abdominal scar [1] . With the advent and popularity of the liposuction The goal of most abdominoplasty procedures is not only to improve the contour and shape of the abdomen, but to procedure and with a better understanding of skin achieve a smooth, flowing, harmonious contour by improving retraction post-liposuction surgery, many of the the overall silhouette and appearance of the region. The waist previously abdominoplasty procedures are now is an area of paramount importance for the feminine figure, treated by the less invasive and more rapid recovery which begins at the level of the lower ribs and ends at the procedure of liposuction surgery. Nevertheless, level of the iliac crest; its narrowest point is approximately 4cm above the navel. The purpose of this study was to report abdominoplasty still holds a very intricate and self- our results on 30 patients who underwent abdominoplasty satisfying place in the world of cosmetic surgery and improvement of the waistline utilizing Scarpa’s fascial [2] . The goal of most abdominoplasty procedures advancement flaps and plication in the midline. is not only to improve the contour and shape of the abdomen, but to achieve a smooth, flowing, Patients and Technique: During a 13-month period from January 2009 to February 2010 we operated on 30 patients. -

Inguinofemoral Area
Inguinofemoral Area Inguinal Canal Anatomy of the Inguinal Canal in Infants and Children There are readily apparent differences between the inguinal canals of infants and adults. In infants, the canal is short (1 to 1.5 cm), and the internal and external rings are nearly superimposed upon one another. Scarpa's fascia is so well developed that the surgeon may mistake it for the aponeurosis of the external oblique muscle, resulting in treating a superficial ectopic testicle as an inguinal cryptorchidism. There also may be a layer of fat between the fascia and the aponeurosis. We remind surgeons of the statement of White that the external oblique fascia has not been reached as long as fat is encountered. In a newborn with an indirect inguinal hernia, there is nothing wrong with the posterior wall of the inguinal canal. Removal of the sac, therefore, is the only justifiable procedure. However, it is extremely difficult to estimate the weakness of the newborn's posterior inguinal wall by palpation. If a defect is suspected, a few interrupted permanent sutures might be used to perform the repair. Adult Anatomy of the Inguinal Canal The inguinal canal in the adult is an oblique rift in the lower part of the anterior abdominal wall. It measures approximately 4 cm in length. It is located 2 to 4 cm above the inguinal ligament, between the opening of the external (superficial) and internal (deep) inguinal rings. The boundaries of the inguinal canal are as follows: Anterior: The anterior boundary is the aponeurosis of the external oblique muscle and, more laterally, the internal oblique muscle. -

Postoperative Pain Treatment with Transmuscular Quadratus
Postoperative Pain Treatment with Transmuscular Quadratus Lumborum Block and Fascia Iliaca Compartment Block in Patients Undergoing Total Hip Arthroplasty: A Randomized Controlled Trial Qin Xia Xuzhou Medical College Aliated Hospital Department of Anaesthesiology Wenping Ding Xuzhou Central Hospital Chao Lin Shanghai Jiaotong University School of Medicine Xinhua Hospital Chongming Branch Jiayi Xia Xuzhou Medical College Aliated Hospital Department of Anaesthesiology Yahui Xu Xuzhou Medical College Aliated Hospital Department of Anaesthesiology Mengxing Jia ( [email protected] ) Xuzhou Medical College Aliated Hospital Department of Anaesthesiology https://orcid.org/0000- 0003-2279-0333 Research article Keywords: Multimodal analgesia, Transmuscular quadratus lumborum block(T-QLB), Fascia iliaca compartment block(FICB), Total hip arthroplasty(THA) Posted Date: January 23rd, 2021 DOI: https://doi.org/10.21203/rs.3.rs-152378/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at BMC Anesthesiology on July 10th, 2021. See the published version at https://doi.org/10.1186/s12871-021-01413-7. Page 1/21 Abstract Background: Patients after total hip arthroplasty (THA) often suffered moderate or even severe pain, seriously affecting the early postoperative recovery. This study aimed to investigate the analgesic ecacy of ultrasound-guided transmuscular quadratus lumborum block (T-QLB) combined with fascia iliaca compartment block (FICB) for elderly patients undergoing THA. Methods: Sixty-four patients scheduled for THA were included in this randomized controlled study. The patients were divided into two groups: group Q and group QF. Before anesthesia induction, group Q was injected with 0.375% ropivacaine 40ml. -

A Device to Measure Tensile Forces in the Deep Fascia of the Human Abdominal Wall
A Device to Measure Tensile Forces in the Deep Fascia of the Human Abdominal Wall Sponsored by Dr. Raymond Dunn of the University of Massachusetts Medical School A Major Qualifying Report Submitted to the Faculty Of the WORCESTER POLYTECHNIC INSTITUTE In partial fulfillment of the requirements for the Degree of Bachelor of Science By Olivia Doane _______________________ Claudia Lee _______________________ Meredith Saucier _______________________ April 18, 2013 Advisor: Professor Kristen Billiar _______________________ Co-Advisor: Dr. Raymond Dunn _______________________ Table of Contents Table of Figures ............................................................................................................................. iv List of Tables ................................................................................................................................. vi Authorship Page ............................................................................................................................ vii Acknowledgements ...................................................................................................................... viii Abstract .......................................................................................................................................... ix Chapter 1: Introduction ................................................................................................................... 1 Chapter 2: Literature Review .........................................................................................................