Case Report Sarcomatoid Carcinoma of Male Urethra with Bone and Lung Metastases Presenting As Urethral Stricture
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Melanoma of Urinary Bladder Presented As Acute Urine Retention. Nirmal Lamichhane1, Hari P Dhakal2 1Department of Surgical Oncology and 2Pathology, B
dd] fl] /on Sof fnf G;/ O] / c f : =s k L t k f = n L a B L . P A . T K I O P S IR O Nepalese Journal of Cancer (NJC) Volume 1 Issue 1 Page 67 - 70 A 2049BS/1992AD H BPKMCH LA BPKMCH,NEPAL R M CE EMORIAL CAN Case report Melanoma of Urinary Bladder presented as acute urine retention. Nirmal Lamichhane1, Hari P Dhakal2 1Department of Surgical Oncology and 2Pathology, B. P. Koirala Memorial Cancer Hospital, Bharatpur, Chitwan, Nepal. ABSTRACT This report is of a 50-year-old man with a rare urinary bladder melanoma. He presented with hematuria followed by bladder outlet obstruction at the time of presentation. Ultrasonogram of the pelvis revealed a mass in the bladder outlet, suggestive of enlarged prostate. Suprapubic cystostomy was then performed. Subsequent transvesical exploration revealed a dark coloured mass at the outlet of bladder, which on histopathology confirmed to be melanoma. After ruling out other possible primary sites, he underwent radical cysto-urethrectomy with urinary diversion. Disease was confirmed with immunohistochemistry. Patient died after 3 months with bilateral lung metastasis. Keywords: Melanoma, Urinary bladder, Cystectomy, Prognosis. INTRODUCTION but was not successful. Sonography was performed Malignant melanoma of urinary bladder is a very rare which showed enlarged prostate and distended bladder. entity and scantly reported in medical literature. Wheelock Suprapubic cystostomy was performed that comforted was the first to report a primary melanoma of the urinary the patient. bladder in 1942, and Su et al. reported the next case in 1962.1, 2 Approximately 50 patients with this tumour On asking, he had voiding type lower urinary tract have been reported in the literature shown by Medline symptoms for 2 and half months, but had no haematuria search. -

Part 2-Organ-Sparing Procedures in Testicular and Penile Tumors
International Urology and Nephrology (2019) 51:1699–1708 https://doi.org/10.1007/s11255-019-02182-6 UROLOGY - REVIEW Organ‑sparing procedures in GU cancer: part 2‑organ‑sparing procedures in testicular and penile tumors Mohamed H. Kamel1,3 · Mahmoud I. Khalil1,3 · Ehab Eltahawy1,3 · Rodney Davis1 · Nabil K. Bissada2 Received: 1 May 2019 / Accepted: 23 May 2019 / Published online: 2 July 2019 © Springer Nature B.V. 2019 Abstract Purpose Organ-sparing surgery (OSS) is recommended in selected patients with testicular tumors and penile cancer (PC). The functional and psychological impacts of organ excision for these genital tumors are profound. In this review, we sum- marize the indications, techniques and outcomes of OSS for these two tumors. Methods PubMed® was searched for relevant articles up to December 2018. For Testicular sparing surgery (TSS) search, keywords used were; testicular tumors alone and in combination with “testicular sparing surgery”, “partial orchiectomy” and outcomes. For penile conserving surgery (PCS), keywords used were: penile cancer alone and in combination with “penile conserving surgery”, “partial penectomy” and outcomes. Because of the low quality of available evidence, a narrative rather that systematic review has been performed. Results Indications of TSS are tumors ≤ 2 cm in solitary testis or bilateral tumors and no rete testis invasion. Prerequisites include normal testosterone and luteinizing hormone levels and patient compliance with follow-up. Indications for PCS are distal penile lesions with clinical stage ≤ T1. Adequate penile stump (3 cm) is required after surgery to maintain forward urine stream. Frozen section helps to reduce the risk of recurrence. Local recurrence after PCS is not associated with reduced survival and can be managed with another PCS in selected patients. -

2005 Tumori Della Vescica Visualizza
Basi scientifiche per la definizione di linee-guida in ambito clinico per i Tumori della Vescica Luglio 2005 1 2 PREFAZIONE Le “Basi scientifiche per la definizione di linee guida in ambito clinico per i Tumori della Vescica” rappresentano un ulteriore risultato del progetto editoriale sponsorizzato e finanziato dai Progetti Strategici Oncologia del CNR-MIUR. Anche in questo caso il proposito degli estensori è stato mirato non già alla costruzione di vere e proprie linee guida, ma a raccogliere in un unico compendio le principali evidenze scientifiche sull’epidemiologia, la diagnosi, l’inquadramento anatomo-patologico e biologico, la stadiazione, il trattamento e il follow-up delle neoplasie della vescica, che sono tra le patologie urologiche più frequenti e di maggiore rilevanza, anche sociale. Il materiale scientifico è ordinato in maniera sinottica, in modo da favorire la consultazione da parte di un’ampia utenza, non solo specialistica, ed è corredato dalle raccomandazioni scaturite dall’esperienza degli esperti qualificati che sono stati coinvolti nella estensione e nella revisione dei diversi capitoli. Tali raccomandazioni hanno lo scopo di consentire al lettore di costruire un proprio percorso diagnostico-terapeutico, alla luce anche delle evidenze fornite. Lasciamo pertanto al lettore il compito di integrare queste raccomandazioni con quanto proviene dalla personale esperienza e di conformarle con le linee guida già esistenti, in relazione anche alle specifiche esigenze. Vista la matrice di questa iniziativa, rappresentata dal CNR e MIUR, non potevano mancare nell’opera specifici riferimenti alle problematiche scientifiche, in grado di fornire spunti per le ricerche future. Certi che anche questa monografia potrà riscuotere lo stesso successo di quelle dedicate in precedenza al carcinoma della prostata e agli altri tumori solidi, sentiamo ancora una volta il dovere di esprimere la nostra gratitudine, per l’impegno e l’essenziale contributo, a tutti gli esperti coinvolti nel Gruppo di Studio e nel Gruppo di Consenso. -

EAU Guidelines on Penile Cancer 2001
European Association of Urology GUIDELINES ON PENILE CANCER* F. Algaba, S. Horenblas, G. Pizzocaro, E. Solsona, T. Windahl TABLE OF CONTENTS PAGE 1. Background 3 2. Classification 3 2.1 Pathology 3 2.2 References 4 3. Risk factors 5 3.1 References 5 4. Diagnosis 6 4.1 Primary lesion 6 4.2 Regional nodes 6 4.3 Distant metastases 7 4.4 Guidelines on the diagnosis of penile cancer 8 4.5 References 8 5. Treatment 9 5.1 Primary lesion 9 5.2 Regional nodes 9 5.3 Guidelines on the treatment of penile carcinoma 11 5.4 Integrated therapy 11 5.5 Distant metastases 11 5.6 Quality life 11 5.7 Technical aspects 12 5.8 Chemotherapy 12 5.9 References 14 6. Follow-up 15 6.1 Why follow-up? 15 6.2 How to follow-up 16 6.3 When to follow-up 16 6.4 Guidelines for follow-up in penile cancer 17 6.5 References 18 7. Abbreviations used in the text 19 2 1. BACKGROUND Penile carcinoma is an uncommon malignant disease with an incidence ranging from 0.1 to 7.9 per 100,000 males. In Europe, the incidence is 0.1–0.9 and in the US, 0.7–0.9 per 100,000 (1). In some areas, such as Asia, Africa and South America, penile carcinoma accounts for as many as 10–20% of male cancers. Phimosis and chronic irritation processes related to poor hygiene are commonly associated with this tumour, whereas neonatal circumcision gives protection against the disease. -

Suprapubic Cystostomy: Urinary Tract Infection and Other Short Term Complications A.T
Suprapubic Cystostomy: Urinary Tract Infection and other short term Complications A.T. Hasan,Q. Fasihuddin,M.A. Sheikh ( Department of Urological Surgery and Transplantation, Jinnah Postgraduate Medical Center, Karachi. ) Abstract Aims: To evaluate the frequency of urinary tract infection in patients with suprapubic cystostomy and other complications of the procedure within 30 days of placement. Methods: Patients characteristics, indication and types of cystostomy and short term (within 30 days); complications were analyzed in 91 patients. Urine analysis and culture was done in all patients to exclude those with urinary tract infection. After 15 and 30 days of the procedure, urine analysis and culture was repeated to evaluate the frequency of urinary tract infection. The prevalence of symptomatic bacteriuria with its organisms was assessed. Antibiotics were given to the postoperative and symptomatic patients and the relationship of antibiotics on the prevention of urinary tract infection was determined. Results: Of the 91 cases 88 were males and 3 females. The mean age was 40.52 ± 18.95 with a range of 15 to 82 years.Obstructive uropathy of lower urinary tract.was present in 81% cases and 17(18.6%) had history of trauma to urethra. All these cases had per-urethral bleeding on examination while x-ray urethrogram showed grade H or grade III injury of urethra. Eighty two of the procedures were performed per-cutaneously and 7 were converted to open cystostomies due to failure of per-cutaneous approach. Nine patients had exploratory laparotomy. Duration of catheterization was the leading risk factor for urinary tract infection found in 24.1% at 15 days and 97.8% at 30 days. -

Bladder Cancer
Clinical Practice in Urology Series Editor: Geoffrey D. Chisholm Titles in the series already published Urinary Diversion Edited by Michael Handley Ashken Chemotherapy and Urological Malignancy Edited by A. S. D. Spiers Urodynamics Paul Abrams, Roger Feneley and Michael Torrens Male Infertility Edited by T. B. Hargreave The Pharmacology of the Urinary Tract Edited by M. Caine Forthcoming titles in the series Urological Prostheses, Appliances and Catheters Edited by J. P. Pryor Percutaneous and Interventional Uroradiology Edited by Erich K. Lang Adenocarcinoma of the Prostate Edited by Andrew W. Bruce and John Trachtenberg Bladder Cancer Edited by E. J. Zingg and D. M. A. Wallace With 50 Figures Springer-Verlag Berlin Heidelberg New York Tokyo E. J. Zingg, MD Professor and Chairman, Department of Urology, Univ~rsity of Berne, Inselspital, 3010 Berne, Switzerland D. M. A. Wallace, FRCS Consultant Urologist, Department of Urology, Queen Elizabeth Medical Centre, Birmingham, England Series Editor Geoffrey D. Chisholm, ChM, FRCS, FRCSEd Professor of Surgery, University of Edinburgh; Consultant Urological Surgeon, Western General Hospital, Edinburgh, Scotland ISBN -13: 978-1-4471-1364-5 e-ISBN -13: 978-1-4471-1362-1 DOI: 10.1007/978-1-4471-1362-1 Library of Congress Cataloging in Publication Data Main entry under title: Bladder Cancer (Clinical Practice in Urology) Includes bibliographies and index. 1. Bladder - Cancer. I. Zingg, Ernst J. II. Wallace, D.M.A. (David Michael Alexander), 1946- DNLM: 1. Bladder Neoplasms. WJ 504 B6313 RC280.B5B632 1985 616.99'462 85-2572 ISBN-13:978-1-4471-1364-5 (U.S.) This work is subject to copyright. -

Long-Term Indwelling Double-J Stent and Multiple Encrusted Stones in the Ureter and Bladder: a Case Report on Holmium Laser Treatment
Pediatr Urol Case Rep 2018; 5(6):161-164 DOI: 10.14534/j-pucr.2018645052 PEDIATRIC UROLOGY CASE REPORTS ISSN 2148-2969 http://www.pediatricurologycasereports.com Long-term indwelling double-J stent and multiple encrusted stones in the ureter and bladder: A case report on Holmium laser treatment Mehmet Hanifi Okur, Selcuk Otcu Department of Pediatric Surgery, Dicle University, School of Medicine, Diyarbakir, Turkey ABSTRACT Double-J (D-J) stents are widely used in a variety of urological interventions. Forgotten D-J stents may lead to complications, such as migration, fragmentation and encrustation. We report the case of a forgotten stent, concomitant with ureteral and bladder stones. The forgotten D-J stent was placed four years prior to our intervention, during treatment for multiple right renal stones. Holmium laser lithotripsy was used to disrupt encrustations on a ureteral orifice and the ureteral stent. The percutaneous suprapubic cystostomy was removed without breaking the stent. The patient was discharged without further complications. Key Words: Double-J (D-J) stents; forgotten stent; encrustation; stone; Holmium laser lithotripsy. Copyright © 2018 pediatricurologycasereports.com Corresponding Author: Dr. Mehmet Hanifi Okur. endourological and open surgical methods Department of Pediatric Surgery, Dicle University, have been reported for the management of School of Medicine, Diyarbakir, Turkey. forgotten D-J stents, there is no standardized E mail: [email protected] ORCID ID: https://orcid.org/0000-0002-6720-1515 approach for their removal in adults and Received 2018-10-09, Accepted 2018-10-21 children [4]. Publication Date 2018-11-01 We report on a case of a forgotten D-J ureteral stent that had been placed during a Introduction percutaneous nephrolithotomy, four years Although Double-J (D-J) stents are widely prior to our intervention. -

Gender Affirming Surgery and Related Procedures State(S): LOB(S): Idaho Montana Oregon Washington Other: Commercial Medicare Medicaid
Gender Affirming Surgery and Related Procedures State(s): LOB(s): Idaho Montana Oregon Washington Other: Commercial Medicare Medicaid Enterprise Policy BACKGROUND The American Psychiatric Association’s Diagnostic and Statistical Manual, 5th Edition (DSM 5) defines criterion A of Gender Dysphoria as “a marked incongruence between one’s experience/expressed gender and assigned gender.” These individuals must meet additional criteria which include persistence over time and clinically significant distress or impairment in social, occupational or other important areas of functioning. Benefits must be verified by reviewing the plan’s contract or plan document (PD). Some PacificSource benefit plans do not include coverage of gender affirming surgery, procedures or other related treatment. Groups may elect to customize these benefits; therefore, benefit determinations are based on specific contract language. CRITERIA The member should be placed into case management by Health Services as a way to help the member understand their benefits and required criteria related to gender affirming surgery and treatment, and to assist her/him to navigate the system and promote an optimal outcome. Covered Services and Exclusions – Commercial, Medicaid 1. The following are considered medically necessary gender affirming surgeries. a. Core surgical procedures considered medically necessary for females transitioning to males include: hysterectomy, vaginectomy, salpingo-oophorectomy, metoidioplasty, phalloplasty, urethroplasty, scrotoplasty, perineal electrolysis, and placement of testicular implant and mastectomy including nipple reconstruction. b. Core surgical procedures considered medically necessary for males transitioning to females include: penectomy, orchiectomy, vaginoplasty, clitoroplasty, perineal electrolysis, labiaplasty, and mammoplasty when 12 continuous months of hormonal (estrogen) therapy has failed to result in breast tissue growth of Tanner Stage 5 on the puberty scale or there is any contraindication to, or intolerance of, or patient refusal of hormone therapy. -
Delineation of Privileges Urology Privileges Provider Name
Delineation Of Privileges Urology Privileges Provider Name: Privilege Requested Deferred Approved UROLOGY PRIVILEGES Criteria - New Applicants:: Board Certification or qualified for certification by the American Board of Urology. Criteria - Current Staff Members Only: Successful completion of an ACGME or AOA approved training program; OR demonstrated acceptable practice in the privileges being requested for a minimum of five (5) years. Proctoring Requirements: A minimum of eight (8) cases, in accordance with the Medical Staff Proctoring Protocol. GENERAL PRIVILEGES: Admit ___ ___ ___ Consultation Only Privileges ___ ___ ___ Surgical Assist Only ___ ___ ___ Local block anesthesia ___ ___ ___ Regional block anesthesia ___ ___ ___ Sedation analgesia ___ ___ ___ Criteria: Requires successful completion of the Sedation Assessment test. Additional criteria effective April 1, 2015: a) Evidence of current ACLS and/or PALS certification from the American Heart Association; AND b) Evidence of completion of an Airway Management Course a) Adult Sedation ___ ___ ___ b) Pediatric Sedation (17 years and under) ___ ___ ___ CATEGORY 1 - UROLOGY PRIVILEGES ___ ___ ___ Includes the management and coordination of care, treatment and services, including: medical history and physical evaluations, consultations and prescribing medication in accordance with DEA certificate. Urethral, bladder catheterization ___ ___ ___ Suprapubic, bladder aspiration ___ ___ ___ Page 1 Printed on Wednesday, December 10, 2014 Delineation Of Privileges Urology Privileges Provider -

A Comprehensive Review of a Rare Subclass of Mucosal Melanoma with Emphasis on Differential Diagnosis and Therapeutic Approaches
cancers Review Urological Melanoma: A Comprehensive Review of a Rare Subclass of Mucosal Melanoma with Emphasis on Differential Diagnosis and Therapeutic Approaches Gerardo Cazzato 1,*,† , Anna Colagrande 1,†, Antonietta Cimmino 1, Concetta Caporusso 1, Pragnell Mary Victoria Candance 1, Senia Maria Rosaria Trabucco 1, Marcello Zingarelli 2, Alfonso Lorusso 2, Maricla Marrone 3 , Alessandra Stellacci 3 , Francesca Arezzo 4, Andrea Marzullo 1, Gabriella Serio 1, Angela Filoni 5, Domenico Bonamonte 5, Paolo Romita 5, Caterina Foti 5, Teresa Lettini 1 , Vera Loizzi 4, Gennaro Cormio 4 , Leonardo Resta 1 , Roberta Rossi 1,‡ and Giuseppe Ingravallo 1,‡ 1 Section of Pathology, Department of Emergency and Organ Transplantation (DETO), University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (A.C.); [email protected] (A.C.); [email protected] (C.C.); [email protected] (P.M.V.C.); [email protected] (S.M.R.T.); [email protected] (A.M.); [email protected] (G.S.); [email protected] (T.L.); [email protected] (L.R.); [email protected] (R.R.); [email protected] (G.I.) 2 Section of Urology, Deparment of Emergency and Organ Transplantation (DETO), University of Bari “Aldo Moro”, 70124 Bari, Italy; [email protected] (M.Z.); [email protected] (A.L.) 3 Section of Legal Medicine, Interdisciplinary Department of Medicine, Bari Policlinico Hospital, Citation: Cazzato, G.; Colagrande, University of Bari Aldo Moro, Piazza Giulio Cesare 11, 70124 Bari, Italy; [email protected] (M.M.); A.; Cimmino, A.; Caporusso, C.; [email protected] (A.S.) Candance, P.M.V.; Trabucco, S.M.R.; 4 Section of Ginecology and Obstetrics, Department of Biomedical Sciences and Human Oncology, Zingarelli, M.; Lorusso, A.; Marrone, University of Bari Aldo Moro, Piazza Giulio Cesare 11, 70124 Bari, Italy; [email protected] (F.A.); M.; Stellacci, A.; et al. -

Urology & Incontinence
Urology & Incontinence - Glossary of Terms Anti-reflux Refers to a tube or collapsible material within a urine collection device to help prevent urine from reentering the tubing. Applicator collar Found on some Hollister male external catheters, a plastic guide with notches for the thumb and forefinger to assist proper placement against the tip of the penis. Aseptic intermittent catheterization The process of performing intermittent catheterization using sterile equipment and inserting the catheter in a sterile way. This would include a sterile ready-to-use product that can be inserted with gloves using a no-touch technique (e.g., the Advance Plus intermittent catheter or a VaPro hydrophilic catheter). Benzalkonium chloride (BZK) An antimicrobial solution used for cleansing the urethral opening prior to inserting an intermittent catheter. Does not stain skin or clothing. Bladder A collapsible balloon-like muscular organ that lies in the pelvis and functions to store and expel urine. Bladder catheterization A procedure in which a catheter is passed through the urethra or stoma into the bladder, usually for the purpose of draining urine. Bladder control The ability to control urination. Bladder diary A printed or electronic form to keep track of when one urinates or leaks urine. Catheter (urinary) A special type of hollow tube inserted through the urethra or a stoma to the bladder to withdraw urine or instill medication. Catheterization The process of inserting a tube into the bladder to drain urine. Clean intermittent catheterization The process of emptying the bladder using a clean intermittent catheter. It involves inserting and removing a catheter, typically several times a day. -
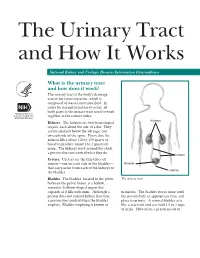
The Urinary Tract and How It Works
The Urinary Tract and How It Works National Kidney and Urologic Diseases Information Clearinghouse What is the urinary tract and how does it work? The urinary tract is the body’s drainage system for removing urine, which is composed of wastes and extra fluid. In order for normal urination to occur, all body parts in the urinary tract need to work together in the correct order. Kidneys Kidneys. The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine. The kidneys work around the clock; a person does not control what they do. Ureters Ureters. Ureters are the thin tubes of muscle—one on each side of the bladder— Bladder that carry urine from each of the kidneys to Urethra the bladder. Bladder. The bladder, located in the pelvis The urinary tract between the pelvic bones, is a hollow, muscular, balloon-shaped organ that expands as it fills with urine. Although a urination. The bladder stores urine until person does not control kidney function, the person finds an appropriate time and a person does control when the bladder place to urinate. A normal bladder acts empties. Bladder emptying is known as like a reservoir and can hold 1.5 to 2 cups of urine. How often a person needs to urinate depends on how quickly the kidneys Why is the urinary tract produce the urine that fills the bladder.