Primary Urethral Carcinoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2005 Tumori Della Vescica Visualizza
Basi scientifiche per la definizione di linee-guida in ambito clinico per i Tumori della Vescica Luglio 2005 1 2 PREFAZIONE Le “Basi scientifiche per la definizione di linee guida in ambito clinico per i Tumori della Vescica” rappresentano un ulteriore risultato del progetto editoriale sponsorizzato e finanziato dai Progetti Strategici Oncologia del CNR-MIUR. Anche in questo caso il proposito degli estensori è stato mirato non già alla costruzione di vere e proprie linee guida, ma a raccogliere in un unico compendio le principali evidenze scientifiche sull’epidemiologia, la diagnosi, l’inquadramento anatomo-patologico e biologico, la stadiazione, il trattamento e il follow-up delle neoplasie della vescica, che sono tra le patologie urologiche più frequenti e di maggiore rilevanza, anche sociale. Il materiale scientifico è ordinato in maniera sinottica, in modo da favorire la consultazione da parte di un’ampia utenza, non solo specialistica, ed è corredato dalle raccomandazioni scaturite dall’esperienza degli esperti qualificati che sono stati coinvolti nella estensione e nella revisione dei diversi capitoli. Tali raccomandazioni hanno lo scopo di consentire al lettore di costruire un proprio percorso diagnostico-terapeutico, alla luce anche delle evidenze fornite. Lasciamo pertanto al lettore il compito di integrare queste raccomandazioni con quanto proviene dalla personale esperienza e di conformarle con le linee guida già esistenti, in relazione anche alle specifiche esigenze. Vista la matrice di questa iniziativa, rappresentata dal CNR e MIUR, non potevano mancare nell’opera specifici riferimenti alle problematiche scientifiche, in grado di fornire spunti per le ricerche future. Certi che anche questa monografia potrà riscuotere lo stesso successo di quelle dedicate in precedenza al carcinoma della prostata e agli altri tumori solidi, sentiamo ancora una volta il dovere di esprimere la nostra gratitudine, per l’impegno e l’essenziale contributo, a tutti gli esperti coinvolti nel Gruppo di Studio e nel Gruppo di Consenso. -

Bladder Cancer
Clinical Practice in Urology Series Editor: Geoffrey D. Chisholm Titles in the series already published Urinary Diversion Edited by Michael Handley Ashken Chemotherapy and Urological Malignancy Edited by A. S. D. Spiers Urodynamics Paul Abrams, Roger Feneley and Michael Torrens Male Infertility Edited by T. B. Hargreave The Pharmacology of the Urinary Tract Edited by M. Caine Forthcoming titles in the series Urological Prostheses, Appliances and Catheters Edited by J. P. Pryor Percutaneous and Interventional Uroradiology Edited by Erich K. Lang Adenocarcinoma of the Prostate Edited by Andrew W. Bruce and John Trachtenberg Bladder Cancer Edited by E. J. Zingg and D. M. A. Wallace With 50 Figures Springer-Verlag Berlin Heidelberg New York Tokyo E. J. Zingg, MD Professor and Chairman, Department of Urology, Univ~rsity of Berne, Inselspital, 3010 Berne, Switzerland D. M. A. Wallace, FRCS Consultant Urologist, Department of Urology, Queen Elizabeth Medical Centre, Birmingham, England Series Editor Geoffrey D. Chisholm, ChM, FRCS, FRCSEd Professor of Surgery, University of Edinburgh; Consultant Urological Surgeon, Western General Hospital, Edinburgh, Scotland ISBN -13: 978-1-4471-1364-5 e-ISBN -13: 978-1-4471-1362-1 DOI: 10.1007/978-1-4471-1362-1 Library of Congress Cataloging in Publication Data Main entry under title: Bladder Cancer (Clinical Practice in Urology) Includes bibliographies and index. 1. Bladder - Cancer. I. Zingg, Ernst J. II. Wallace, D.M.A. (David Michael Alexander), 1946- DNLM: 1. Bladder Neoplasms. WJ 504 B6313 RC280.B5B632 1985 616.99'462 85-2572 ISBN-13:978-1-4471-1364-5 (U.S.) This work is subject to copyright. -

Clinical Radiation Oncology Review
Clinical Radiation Oncology Review Daniel M. Trifiletti University of Virginia Disclaimer: The following is meant to serve as a brief review of information in preparation for board examinations in Radiation Oncology and allow for an open-access, printable, updatable resource for trainees. Recommendations are briefly summarized, vary by institution, and there may be errors. NCCN guidelines are taken from 2014 and may be out-dated. This should be taken into consideration when reading. 1 Table of Contents 1) Pediatrics 6) Gastrointestinal a) Rhabdomyosarcoma a) Esophageal Cancer b) Ewings Sarcoma b) Gastric Cancer c) Wilms Tumor c) Pancreatic Cancer d) Neuroblastoma d) Hepatocellular Carcinoma e) Retinoblastoma e) Colorectal cancer f) Medulloblastoma f) Anal Cancer g) Epndymoma h) Germ cell, Non-Germ cell tumors, Pineal tumors 7) Genitourinary i) Craniopharyngioma a) Prostate Cancer j) Brainstem Glioma i) Low Risk Prostate Cancer & Brachytherapy ii) Intermediate/High Risk Prostate Cancer 2) Central Nervous System iii) Adjuvant/Salvage & Metastatic Prostate Cancer a) Low Grade Glioma b) Bladder Cancer b) High Grade Glioma c) Renal Cell Cancer c) Primary CNS lymphoma d) Urethral Cancer d) Meningioma e) Testicular Cancer e) Pituitary Tumor f) Penile Cancer 3) Head and Neck 8) Gynecologic a) Ocular Melanoma a) Cervical Cancer b) Nasopharyngeal Cancer b) Endometrial Cancer c) Paranasal Sinus Cancer c) Uterine Sarcoma d) Oral Cavity Cancer d) Vulvar Cancer e) Oropharyngeal Cancer e) Vaginal Cancer f) Salivary Gland Cancer f) Ovarian Cancer & Fallopian -

Urinary Bladder Neoplasia
Canine Urinary Tract Neoplasia Phyllis C Glawe DVM, MS The principal organs of the urinary tract are the kidneys, ureters, urinary bladder and urethra. The urinary bladder and urethra are the most commonly affected by cancer in the dog and the majority of cancers in these locations are malignant. The most common type of cancer is Transitional Cell Carcinoma (TCC). This handout reviews the facts about clinical symptoms, diagnosis and treatment of urinary tract cancer in the dog. Clinical Features More common in female dogs, urinary bladder and urethral cancer are typically associated with advanced age (9-10 years). Frequent urination, blood in the urine, and straining to urinate are typical symptoms. These signs are also similar to those of urinary tract infections, thus a cancer diagnosis can be missed early in the course of the disease. If the flow of urine is obstructed, abdominal pain, vomiting, depression and loss of appetite can occur. More rarely, dogs can present with back pain and weakness of the hind limbs due to metastases (spread) of the cancer to the spine and lymph nodes. Diagnosis Abdominal radiographs and abdominal ultrasound can be utilized to detect cancer in the lower urinary tract. Abdominal ultrasound is particularly helpful to assess whether other organs in the abdomen region are affected, such as the kidneys and ureters. Hydronephrosis and hydroureter are terms describing a back-up of urine flow due to the obstructive effects of a tumor. Regional lymph node enlargement and possible prostate enlargement in male dogs can be assessed quickly and accurately with ultrasound. Urine analysis is not very helpful as a diagnostic tool in most cases. -

Urology Clinical Privileges
Urology Clinical Privileges Name: _____________________________________________________ Effective from _______/_______/_______ to _______/_______/_______ ❏ Initial privileges (initial appointment) ❏ Renewal of privileges (reappointment) All new applicants should meet the following requirements as approved by the governing body, effective: February 18, 2015 Applicant: Check the “Requested” box for each privilege requested. Applicants are responsible for producing required documentation for a proper evaluation of current skill, current clinical activity, and other qualifications and for resolving any doubts related to qualifications for requested privileges. Please provide this supporting information separately. [Department/Program Head or Leaders/ Chief]: Check the appropriate box for recommendation on the last page of this form and include your recommendation for any required evaluation. If recommended with conditions or not recommended, provide the condition or explanation on the last page of this form. Current experience is an estimate of the level of activity below which a collegial discussion about support should be triggered. It is not a disqualifier. This discussion should be guided not only by the expectations and standards outlined in the dictionary but also by the risks inherent in the privilege being discussed and by similar activities that contribute to the skill under consideration. This is an opportunity to reflect with a respected colleague on one's professional practice and to deliberately plan an approach to skills maintenance. Other requirements • Note that privileges granted may only be exercised at the site(s) and/or setting(s) that have sufficient space, equipment, staffing, and other resources required to support the privilege. • This document is focused on defining qualifications related to competency to exercise clinical privileges. -

Sarcomatoid Urothelial Carcinoma Arising in the Female Urethral Diverticulum
Journal of Pathology and Translational Medicine 2021; 55: 298-302 https://doi.org/10.4132/jptm.2021.04.23 CASE STUDY Sarcomatoid urothelial carcinoma arising in the female urethral diverticulum Heae Surng Park Department of Pathology, Ewha Womans University Seoul Hospital, Seoul, Korea A sarcomatoid variant of urothelial carcinoma in the female urethral diverticulum has not been reported previously. A 66-year-old woman suffering from dysuria presented with a huge urethral mass invading the urinary bladder and vagina. Histopathological examination of the resected specimen revealed predominantly undifferentiated pleomorphic sarcoma with sclerosis. Only a small portion of conven- tional urothelial carcinoma was identified around the urethral diverticulum, which contained glandular epithelium and villous adenoma. The patient showed rapid systemic recurrence and resistance to immune checkpoint inhibitor therapy despite high expression of pro- grammed cell death ligand-1. We report the first case of urethral diverticular carcinoma with sarcomatoid features. Key Words: Sarcomatoid carcinoma; Urothelial carcinoma; Urethral diverticulum Received: March 9, 2021 Revised: April 16, 2021 Accepted: April 23, 2021 Corresponding Author: Heae Surng Park, MD, PhD, Department of Pathology, Ewha Womans University Seoul Hospital, Ewha Womans University College of Medicine, 260 Gonghang-daero, Gangseo-gu, Seoul 07804, Korea Tel: +82-2-6986-5253, Fax: +82-2-6986-3423, E-mail: [email protected] Urethral diverticular carcinoma (UDC) is extremely rare; the urinary bladder, and vagina with enlarged lymph nodes at both most common histological subtype is adenocarcinoma [1,2]. femoral, both inguinal, and both internal and external iliac areas Sarcomatoid urothelial carcinoma (UC) is also unusual. Due to (Fig. 1B). -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Bladder Cancer
PDF hosted at the Radboud Repository of the Radboud University Nijmegen The following full text is a publisher's version. For additional information about this publication click this link. http://hdl.handle.net/2066/19207 Please be advised that this information was generated on 2021-09-27 and may be subject to change. SUPERFICIAL BLADDER CANCER PROGNOSIS AND MANAGEMENT SUPERFICIAL BLADDER CANCER PROGNOSIS AND MANAGEMENT een wetenschappelijke proeve op het gebied van de Medische Wetenschappen Proefschrift ter verkrijging van de graad van doctor aan de Katholieke Universiteit Nijmegen op gezag van de Rector Magnificus Prof. dr. C. W. P. M. Blom, volgens besluit van het College van Decanen in het openbaar te verdedigen op woensdag 11 december 2002 des morgens om 11.00 uur precies door Necmettin Aydin Mungan geboren op 24 maart 1965 te Ankara Promotor : Prof. dr. F.M.J. Debruyne Co-Promotores : Dr. J.A. Witjes Dr. L.A.L.M. Kiemeney Manuscriptcommissie : Prof. dr. P. de Mulder Prof. dr. A.L.M. Lagro-Janssen Prof. dr. H. Boonstra Superficial bladder cancer: prognosis and management Necmettin Aydin Mungan ISBN 90-9016303-4 Printed by: ZES Tanitim, Ankara Cover design: Superficial bladder cancer Publication of this thesis was sponsored by: Onko&Koçsel Pharmaceuticals and Aventis Pasteur, Schering-Plough and Abbott Laboratories To my wife and kids Science is the truest guide for life, success and everything else in the world. Mustafa Kemal Ataturk Founder of Republic of Turkey CONTENTS Chapter Title Page 1 Introduction and outline of the thesis 9 2 Gender differences of (superficial) bladder cancer 21 3 Can sensitivity of voided urinary cytology or bladder 67 wash cytology be improved by the use of different urinary portions? 4 Detection of malignant cells: Can cytology be 79 replaced? 5 Comparison of the diagnostic value of the BTA Stat 101 Test with voided urinary cytology for detection of bladder cancer. -

Male Urethral Cancer May Be Primary Or Secondary
Urethral cancer Male urethral cancer May be primary or secondary: primary rare; secondary commonly a/w urothelial carcinoma of the bladder Primary urethral carcinoma usually arises secondary to chronic irritation Urethral stricture Frequent STI/urethritis Presentation haematuria urethral bleeding persistent urethral stricture urethrocutaneous fistula Histology 80% squamous cell carcinoma (a/w HPV 16) 15% transitional cell carcinoma 5% other (adenoCa, melanoma etc.) Location 60% bulbomembranous 30% penile 10% prostatic Generally anterior urethral tumours do better than posterior urethral tumours Spread Anterior urethra – superficial and deep inguinal LNs (unlike penile carcinoma palpable LNs almost always metastatic) Posterior urethra – pelvic LNs Staging (UICC) Tx Tumour cannot be assessed T0 No evidence of primary tumour Tis CIS Ta Papillary, polypoid or verucoid tumour T1 Tumour invades subepithelial connective tissue T2 Tumour invades corpus spongiosum or prostate stroma T3 Corpus cavernosum, vagina or bladder neck T4 Other adjacent structures Nx Nodal disease cannot be assessed N0 No evidence of nodal disease N1 Metastasis to a single LN < 2cm N2 Metastasis to LN 2-5cm, or multiple LNs < 5cm N3 Metastasis to LN > 5cm Mx Distant mets cannot be assessed M0 No distant mets M1 Distant mets Tom Walton January 2011 1 Urethral cancer Management Depends on location and tumour stage: (i) Penile urethra Superficial (<T2) Transurethral resection Local excision and anastomosis Local excision and perineal urostomy Penis tip tumours may be treated -

Cancer in Urinary Tract and Bladder Caiga Du* Vancouver Prostate Centre, Jack Bell Research Centre, Canada
Surgica OPEN ACCESS Freely available online l & l U a r ic o d lo e g y M Medical & Surgical Urology ISSN: 2168-9857 Commentary Cancer in Urinary Tract and Bladder Caiga Du* Vancouver Prostate Centre, Jack Bell Research Centre, Canada Cancer is when cells in the body outgrow control, regularly shaping To understand cancer of the ureter and renal pelvis, it assists with a mass or tumor. In upper urinary tract cancer, unusual cells are realizing how these organs normally work. found in the: • Bladder Cancer: Symptoms and Signs. • Renal pelvis (where urine gathers in the kidneys before it goes • Blood or blood clusters in the urine. to the ureters and bladder) • Pain or burning sensation during urine. • Renal calyces (spaces deep in the kidneys) • Frequent urine. • Ureters (thin tubes, made of muscle, which move urine from the kidney to the bladder) • Feeling the need to urinate many times throughout the night. Cancers of the upper urinary tract are moderately uncommon. The • Feeling the need to urine, not being able to pass urine. most common of all upper urinary tract cancers are those found in • Lower back pain on 1 side of the body. the renal pelvis and renal calyces. Cancer in the ureters makes up about a fourth of all upper urinary tract cancers. Bladder cancer is exceptionally treatable when it is analyzed in the beginning phases. The fundamental sorts of therapies for bladder Tumors of the renal calyces, renal pelvis and ureters start in the cancer include: Surgery: Bladder cancer therapy quite often has layer of tissue that lines the bladder and the upper urinary ptract, a careful part that might be joined with other non-obtrusive called the urothelium. -

Prostate Gland Biopsy
PROSTATE GLAND BIOPSY EUGENE F. POUTASSE, M.D. Department of Urology HE incidence of cancer of the prostate gland among men who have symp- Ttoms of bladder neck obstruction is about one out of five. The actual inci- dence of cancer is higher because many men are seen with symptoms unrelated to the urinary tract, such as bone pain, or who have evidence of the tumor without symptoms. It is the third most common cancer in men, exceeded only by cancer of the skin and alimentary tract in frequency of recognition. The chief methods by which a physician discovers prostatic cancer are rectal palpation of the gland, serum acid phosphatase determination, and roentgenographic study of the urinary tract and skeleton. These are satisfactory when the tumor has spread widely beyond the prostate. In this paper methods of biopsy for establishing the diagnosis when cancer of the prostate gland is suspected or when it is desirable to corroborate the clinical diagnosis of exten- sive cancer will be discussed. The actual diagnosis of cancer is made by micro- scopic definition, preferably on a block of tumor tissue. Under study is the cytologic examination of prostatic secretion for exfoliated tumor cells,1 which requires a great deal of time and experience. Methods of Biopsy A. Perineal. Exposure of the prostate gland through the perineum permits biopsy of any area of the gland which has been suspected of malignancy on rectal palpation. This approach is particularly useful because more than 90 per cent of all prostatic neoplasms arise in the posterior lobe accessible to rectal palpation. -
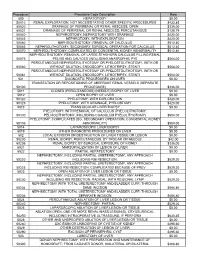
Procedure Procedure Code Description Rate 500
Procedure Procedure Code Description Rate 500 HEPATOTOMY $0.00 50010 RENAL EXPLORATION, NOT NECESSITATING OTHER SPECIFIC PROCEDURES $433.85 50020 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; OPEN $336.00 50021 DRAINAGE OF PERIRENAL OR RENAL ABSCESS; PERCUTANIOUS $128.79 50040 NEPHROSTOMY, NEPHROTOMY WITH DRAINAGE $420.00 50045 NEPHROTOMY, WITH EXPLORATION $420.00 50060 NEPHROLITHOTOMY; REMOVAL OF CALCULUS $512.40 50065 NEPHROLITHOTOMY; SECONDARY SURGICAL OPERATION FOR CALCULUS $512.40 50070 NEPHROLITHOTOMY; COMPLICATED BY CONGENITAL KIDNEY ABNORMALITY $512.40 NEPHROLITHOTOMY; REMOVAL OF LARGE STAGHORN CALCULUS FILLING RENAL 50075 PELVIS AND CALYCES (INCLUDING ANATROPHIC PYE $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50080 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 PERCUTANEOUS NEPHROSTOLITHOTOMY OR PYELOSTOLITHOTOMY, WITH OR 50081 WITHOUT DILATION, ENDOSCOPY, LITHOTRIPSY, STENTI $504.00 501 DIAGNOSTIC PROCEDURES ON LIVER $0.00 TRANSECTION OR REPOSITIONING OF ABERRANT RENAL VESSELS (SEPARATE 50100 PROCEDURE) $336.00 5011 CLOSED (PERCUTANEOUS) (NEEDLE) BIOPSY OF LIVER $0.00 5012 OPEN BIOPSY OF LIVER $0.00 50120 PYELOTOMY; WITH EXPLORATION $420.00 50125 PYELOTOMY; WITH DRAINAGE, PYELOSTOMY $420.00 5013 TRANSJUGULAR LIVER BIOPSY $0.00 PYELOTOMY; WITH REMOVAL OF CALCULUS (PYELOLITHOTOMY, 50130 PELVIOLITHOTOMY, INCLUDING COAGULUM PYELOLITHOTOMY) $504.00 PYELOTOMY; COMPLICATED (EG, SECONDARY OPERATION, CONGENITAL KIDNEY 50135 ABNORMALITY) $504.00 5014 LAPAROSCOPIC LIVER BIOPSY $0.00 5019 OTHER DIAGNOSTIC PROCEDURES