9Th EDITION CLINICIAN’S POCKET REFERENCE
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Childhood Functional Gastrointestinal Disorders: Child/Adolescent
Gastroenterology 2016;150:1456–1468 Childhood Functional Gastrointestinal Disorders: Child/ Adolescent Jeffrey S. Hyams,1,* Carlo Di Lorenzo,2,* Miguel Saps,2 Robert J. Shulman,3 Annamaria Staiano,4 and Miranda van Tilburg5 1Division of Digestive Diseases, Hepatology, and Nutrition, Connecticut Children’sMedicalCenter,Hartford, Connecticut; 2Division of Digestive Diseases, Hepatology, and Nutrition, Nationwide Children’s Hospital, Columbus, Ohio; 3Baylor College of Medicine, Children’s Nutrition Research Center, Texas Children’s Hospital, Houston, Texas; 4Department of Translational Science, Section of Pediatrics, University of Naples, Federico II, Naples, Italy; and 5Department of Gastroenterology and Hepatology, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina Characterization of childhood and adolescent functional Rome III criteria emphasized that there should be “no evi- gastrointestinal disorders (FGIDs) has evolved during the 2- dence” for organic disease, which may have prompted a decade long Rome process now culminating in Rome IV. The focus on testing.1 In Rome IV, the phrase “no evidence of an era of diagnosing an FGID only when organic disease has inflammatory, anatomic, metabolic, or neoplastic process been excluded is waning, as we now have evidence to sup- that explain the subject’s symptoms” has been removed port symptom-based diagnosis. In child/adolescent Rome from diagnostic criteria. Instead, we include “after appro- IV, we extend this concept by removing the dictum that priate medical evaluation, the symptoms cannot be attrib- “ ” fi there was no evidence for organic disease in all de ni- uted to another medical condition.” This change permits “ tions and replacing it with after appropriate medical selective or no testing to support a positive diagnosis of an evaluation the symptoms cannot be attributed to another FGID. -

General Signs and Symptoms of Abdominal Diseases
General signs and symptoms of abdominal diseases Dr. Förhécz Zsolt Semmelweis University 3rd Department of Internal Medicine Faculty of Medicine, 3rd Year 2018/2019 1st Semester • For descriptive purposes, the abdomen is divided by imaginary lines crossing at the umbilicus, forming the right upper, right lower, left upper, and left lower quadrants. • Another system divides the abdomen into nine sections. Terms for three of them are commonly used: epigastric, umbilical, and hypogastric, or suprapubic Common or Concerning Symptoms • Indigestion or anorexia • Nausea, vomiting, or hematemesis • Abdominal pain • Dysphagia and/or odynophagia • Change in bowel function • Constipation or diarrhea • Jaundice “How is your appetite?” • Anorexia, nausea, vomiting in many gastrointestinal disorders; and – also in pregnancy, – diabetic ketoacidosis, – adrenal insufficiency, – hypercalcemia, – uremia, – liver disease, – emotional states, – adverse drug reactions – Induced but without nausea in anorexia/ bulimia. • Anorexia is a loss or lack of appetite. • Some patients may not actually vomit but raise esophageal or gastric contents in the absence of nausea or retching, called regurgitation. – in esophageal narrowing from stricture or cancer; also with incompetent gastroesophageal sphincter • Ask about any vomitus or regurgitated material and inspect it yourself if possible!!!! – What color is it? – What does the vomitus smell like? – How much has there been? – Ask specifically if it contains any blood and try to determine how much? • Fecal odor – in small bowel obstruction – or gastrocolic fistula • Gastric juice is clear or mucoid. Small amounts of yellowish or greenish bile are common and have no special significance. • Brownish or blackish vomitus with a “coffee- grounds” appearance suggests blood altered by gastric acid. -

Observational Study of Children with Aerophagia
Clinical Pediatrics http://cpj.sagepub.com Observational Study of Children With Aerophagia Vera Loening-Baucke and Alexander Swidsinski Clin Pediatr (Phila) 2008; 47; 664 originally published online Apr 29, 2008; DOI: 10.1177/0009922808315825 The online version of this article can be found at: http://cpj.sagepub.com/cgi/content/abstract/47/7/664 Published by: http://www.sagepublications.com Additional services and information for Clinical Pediatrics can be found at: Email Alerts: http://cpj.sagepub.com/cgi/alerts Subscriptions: http://cpj.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav Citations (this article cites 18 articles hosted on the SAGE Journals Online and HighWire Press platforms): http://cpj.sagepub.com/cgi/content/refs/47/7/664 Downloaded from http://cpj.sagepub.com at Charite-Universitaet medizin on August 26, 2008 © 2008 SAGE Publications. All rights reserved. Not for commercial use or unauthorized distribution. Clinical Pediatrics Volume 47 Number 7 September 2008 664-669 © 2008 Sage Publications Observational Study of Children 10.1177/0009922808315825 http://clp.sagepub.com hosted at With Aerophagia http://online.sagepub.com Vera Loening-Baucke, MD, and Alexander Swidsinski, MD, PhD Aerophagia is a rare disorder in children. The diagnosis is stool and gas. The abdominal X-ray showed gaseous dis- often delayed, especially when it occurs concomitantly tention of the colon in all and of the stomach and small with constipation. The aim of this report is to increase bowel in 8 children. Treatment consisted of educating awareness about aerophagia. This study describes 2 girls parents and children about air sucking and swallowing, and 7 boys, 2 to 10.4 years of age, with functional consti- encouraging the children to stop the excessive air swal- pation and gaseous abdominal distention. -

Management of Specific Wounds
7 Management of Specific Wounds Bite Wounds 174 Hygroma 234 Burns 183 Snakebite 239 Inhalation Injuries 195 Brown Recluse Spider Bites 240 Chemical Burns 196 Porcupine Quills 240 Electrical Injuries 197 Lower Extremity Shearing Wounds 243 Radiation Injuries 201 Plate 10: Pipe Insulation Protective Frostbite 204 Device: Elbow 248 Projectile Injuries 205 Plate 11: Pipe Insulation to Protect Explosive Munitions: Ballistic, the Greater Trochanter 250 Blast, and Thermal Injuries 227 Plate 12: Vacuum Drain Impalement Injuries 227 Management of Elbow Pressure Ulcers 228 Hygromas 252 Atlas of Small Animal Wound Management and Reconstructive Surgery, Fourth Edition. Michael M. Pavletic. © 2018 John Wiley & Sons, Inc. Published 2018 by John Wiley & Sons, Inc. Companion website: www.wiley.com/go/pavletic/atlas 173 174 Atlas of Small Animal Wound Management and Reconstructive Surgery BITE WOUNDS to the skin. Wounds may be covered by a thick hair coat and go unrecognized. The skin and underlying Introduction issues can be lacerated, stretched, crushed, and avulsed. Circulatory compromise from the division of vessels and compromise to collateral vascular channels can result in Bite wounds are among the most serious injuries seen in massive tissue necrosis. It may take several days before small animal practice, and can account for 10–15% of all the severity of tissue loss becomes evident. All bites veterinary trauma cases. The canine teeth are designed are considered contaminated wounds: the presence of for tissue penetration, the incisors for grasping, and the bacteria in the face of vascular compromise can precipi- molars/premolars for shearing tissue. The curved canine tate massive infection. teeth of large dogs are capable of deep penetration, whereas the smaller, straighter canine teeth of domestic cats can penetrate directly into tissues, leaving a rela- tively small cutaneous hole. -

High B1a0d Pressure and Its Treatment in General
HIGH B1A0D PRESSURE AND ITS TREATMENT IN GENERAL PRACTICE WITH PARTICULAR REFERENCE TO A SERIES OF 100 CASES TREATED BY THE AUTHOR By HAROLD WILSON B01YBR IB.ffh.B. ProQuest Number: 13849841 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 13849841 Published by ProQuest LLC(2019). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 -CONTENTS SECTION 1. Introduction. SECTION 2. General Remarks. Definitions of General Interest. Present Views on Etiology. Pathology and Morbid Anatomy. Brief Historical Survey. SECTION 3. The Present Position. Prevalence. Clinical Manifestations. Prognosis. SECTION 4. Prevalence in Bolton. Summary of Cases. Symptomatology and Case Histories Prognosis. Treatment. SECTION 5. Conclusions. Bibliography. SECTION 1. INTRODUCTION. I think it can truthfully be said that the most interest ing problems in Medioine are those that are most baffling. Some years ago Ralph M a j o r ^ wrote these words, ”If our knowledge of the etiology of arterial hypertension is shrouded in a oertain haze, our knowledge of an effective therapy in this disease is enveloped in a dense fog.n A study of some of the vast literature on this subject does not greatly clarify the obscurity. -

Respiratory Examination Cardiac Examination Is an Essential Part of the Respiratory Assessment and Vice Versa
Respiratory examination Cardiac examination is an essential part of the respiratory assessment and vice versa. # Subject steps Pictures Notes Preparation: Pre-exam Checklist: A Very important. WIPE Be the one. 1 Wash your hands. Wash your hands in Introduce yourself to the patient, confirm front of the examiner or bring a sanitizer with 2 patient’s ID, explain the examination & you. take consent. Positioning of the patient and his/her (Position the patient in a 3 1 2 Privacy. 90 degree sitting position) and uncover Exposure. full exposure of the trunk. his/her upper body. 4 (if you could not, tell the examiner from the beginning). 3 4 Examination: General appearance: B (ABC2DEVs) Appearance: young, middle aged, or old, Begin by observing the and looks generally ill or well. patient's general health from the end of the bed. Observe the patient's general appearance (age, Around the bed I can't state of health, nutritional status and any other see any medications, obvious signs e.g. jaundice, cyanosis, O2 mask, or chest dyspnea). 1 tube(look at the lateral sides of chest wall), metered dose inhalers, and the presence of a sputum mug. 2 Body built: normal, thin, or obese The patient looks comfortable and he doesn't appear short of breath and he doesn't obviously use accessory muscles or any heard Connections: such as nasal cannula wheezes. To determine this, check for: (mention the medications), nasogastric Dyspnea: Assess the rate, depth, and regularity of the patient's 3 tube, oxygen mask, canals or nebulizer, breathing by counting the respiratory rate, range (16–25 breaths Holter monitor, I.V. -

DISEASES of ARTERIES ARTERIOSCLEROSIS (“Hardening of the Arteries”): General Term Reflecting Arterial Wall Thickening and Loss of Elasticity
DISEASES OF ARTERIES ARTERIOSCLEROSIS (“hardening of the arteries”): general term reflecting arterial wall thickening and loss of elasticity 3 patterns •Atherosclerosis: involves the the aorta and the large arteries •Mönckeberg sclerosis: calcific deposits in the media of middle-sized arteries in persons >age 50 •Arteriolosclerosis: involves the small arteries and arterioles in association with hypertension or diabetes ATHEROSCLEROSIS Multifactorial, slowly progressive chronic degenerative-inflammatory disease of the aorta and the large arteries, such as • coronary arteries • circle of Willis • popliteal and tibial arteries Significance: > 50% of all death is attributed to atherosclerosis in well-developed countries Morphology Gross • Atheromatous plaque (pathognomic) - raised white-yellow lesion in the intima, protruding into the lumen • Large plaques in the aorta (> 2 cm) contain a yellow, grumous debris (”atheroma” - Greek word for gruel) Atheromatous plaque in the middle cerebral artery: raised white-yellow lesion in the intima, protruding into the lumen (formol-fixed brain) Aorta: the plaques contain a yellow, grumous debris (arrow) Structure of atheroma on LM • Intimal lesion • Central lipid core • Fibrous ”cap” subendothelially Central lipid core composed of lipids, cholesterol clefts, necrotic debris + calcium-salts, surrounded by foamy macrophages, T-lymphocytes, fibroblasts, small capillaries, and collagens and proteoglycans Types of plaques • Vulnerable plaques have large atheromatous cores, increased inflammatory cell content and thin fibrous caps high risk of rupture thrombosis • Stable plaques have minimal atheromatous cores and inflammation and thick fibrous caps 70% stenosis (critical stenosis) chronic ischemia distally Vulnerable plaque in the coronary artery Inflammatory infiltrates and capillaries around the lipid core. Lumen Intima Media Pathogenesis Response to chronic endocardial injury hypothesis • Cholesterol can’t dissolve in the blood. -

Reconstructive
RECONSTRUCTIVE Muscle versus Nonmuscle Flaps in the Reconstruction of Chronic Osteomyelitis Defects Christopher J. Salgado, Background: Surgical treatment of chronic osteomyelitis requires aggressive M.D. debridement followed by wound coverage and obliteration of dead space with Samir Mardini, M.D. vascularized tissue. Controversy remains as to the effectiveness of different tissue Amir A. Jamali, M.D. types in achieving these goals and in the eradication of disease. Juan Ortiz, M.D. Methods: Chronic osteomyelitis was induced in 26 goat tibias using Staphylo- Raoul Gonzales, D.V.M., coccus aureus as an infecting inoculum. In a single stage, debridement followed Ph.D. by reconstruction using either a muscle flap (n ϭ 13) or a fasciocutaneous flap Hung-Chi Chen, M.D. (n ϭ 13) was performed. Flap donor sites were closed primarily and antibiotics El Paso, Texas; Kaohsiung, Taiwan; were given for 5 days postoperatively. Daily clinical evaluation for 1 year was and Sacramento, Calif. performed and monthly radiographs were obtained for 9 months and 1 year after the reconstruction. Results: Twenty-five flaps survived completely, and one nonmuscle flap under- went partial flap loss following a period of venous congestion. There were no postoperative complications in the muscle flap group. Two goats (15 percent) in the nonmuscle group developed superficial wounds in the immediate post- operative period that resolved with conservative management. No limbs had recurrent osteomyelitis wounds at 1 year of clinical follow-up examination. Radiographic evidence of osteomyelitis was present in two goats (15 percent) in the muscle group and one goat (8 percent) in the nonmuscle group. -

Visual Examination
Visual Examination • Consider the impact of chest shape on the respiratory condition of the patient – Barrel chest – Kyphosis – Scoliosis – Pectus excavatum (funnel chest) – Pectus carinatum Visual Assessment of Thorax • Thoracic scars from previous surgery • Chest symmetry • Use of accessory muscles • Bruising • In drawing of ribs • Flail segment www.nejm.org/doi/full/10.1056/NEJMicm0904437 • Paradoxical breathing /seesaw breathing • Pursed lip breathing • Nasal flaring Palpation • For vibration of secretion • Surgical emphysema • Symmetry of chest movement • Tactile vocal fremitus • Check for a tracheal tug • Palpate Nodes http://www.ncbi.nlm.nih.gov/books/NBK368/ https://m.youtube.com/watch?v=uzgdaJCf0Mk Auscultation • Is there any air entry? • Differentiate – Normal vesicular sounds – Bronchial breathing – Wheeze – Distinguish crackles • Fine • Coarse • During inspiration or expiration • Profuse or scanty – Absent sounds – Vocal resonance http://www.easyauscultation.com/lung-sounds.aspx Percussion • Tapping of the middle phalanx of the left middle finger with the right middle finger • Sounds should be resonant but may be – Hyper resonant – Dull – Stony Dull http://stanfordmedicine25.stanford.edu/the25/pulmonary.html Pathological Expansion Mediastinal Percussion Breath Further Process Displacement Note Sounds Examination Consolidation Reduced on None Dull Bronchial affected side breathing Vocal resonance Whispering pectoriloquy Collapse Reduced on Towards Dull Reduced None affected side affected side Pleural Reduced on Towards Stony dull Reduced/ Occasional rub effusion affected side opposite side Absent Empyema Asthma Reduced None Resonant Normal/ Wheeze throughout Reduced COPD Reduced None Resonant/ Normal/ Wheeze throughout Hyper-resonant Reduced Pulmonary Normal or None Normal Normal Bibasal crepitations Fibrosis reduced throughout Pneumothorax Reduced on Towards Hyper-resonant Reduced/ None affected side opposite side Absent http://www.cram.com/flashcards/test/lung-sounds-886428 sign up and test yourself.. -

THE DUBLIN MEDICAL SCHOOL and ITS INFLUENCE UPON MEDICINE in AMERICA1 by DAVID RIESMAN, M.D
THE DUBLIN MEDICAL SCHOOL AND ITS INFLUENCE UPON MEDICINE IN AMERICA1 By DAVID RIESMAN, M.D. PROFESSOR OF CLINICAL MEDICINE IN THE UNIVERSITY OF PENNSYLVANIA PHILADELPHIA, PA. HE Irish, a mixture of primitive universal genius like Robert Boyle, Ireland pre-Celtic peoples and of Goidelic did not produce a perpetuating body of Celts coming from the European learned men who made their influence felt T continent, developed in the early beyond the confines of the Green Island. Middle Ages, out of their own resources Of the history of Irish medicine in the and untouched in any marked degree by the Middle Ages, little is known and the all-pervading influence of Rome, a remark subject is largely an untilled field. Norman able indigenous culture. In particular they Moore (St. Barth. Hosp. Rep., 1875, it elaborated a native type of Christianity 145) has resuscitated a few of the original which with characteristic energy and manuscripts in the Irish language. Most wandering spirit they carried to Scotland, of them are translations from the works of to Northern England—to Northumbria—to Bernard de Gordon, especially from his France, to Belgium, and to Switzerland. “Lilium Medicinae”; of John of Gaddes- St. Columba, of Iona, and St. Columbanus, den’s “Rosa Anglica”; of the works of of Luxeuil, stand forth as the great militant Avicenna, of A verroes, of Isaac, and of the missionaries of that first flowering period Salernitan School. Much space is given to of Irish civilization. Although they and their the writings of Isidorus. This Isidorus is successors had to succumb to the greater the famous Spanish churchman, bishop might of Latin Christianity,2 they left of Seville, who not only was a master of dotted over Europe a number of large theology but a writer upon every branch of monasteries which became active centers of knowledge of his day. -

(TECA) Surgery
Audit of Total Ear Canal Ablation-Lateral Bulla Osteotomy Procedures Performed by One Surgeon Audit project lead: D G Bentley Subject/area of practice: Surgery/Dermatology Date: January 2nd 2018 Reasons for Audit: To determine how complication rate of this procedure, both short and long term, compare with that in recently published literature and to be sure this procedure should be still be offered in-house rather than being referred to a surgical specialist. Background Total Ear Canal Ablation-Lateral Bulla Osteotomy (TECA-LBO) procedures on dogs (and cats) have been performed by this surgeon since 1991 and since that time over 260 procedures have been performed. The surgeon also runs a dermatology service with special interest in ear disease and wishes to provide a complete service whereby cases that are beyond medical treatment can go to surgery without being referred to a specialist surgeon. Indications for TECA-LBO are “end stage otitis”, where there is chronic irreversible change to the ear canal, intractable ear infections particularly as a result of middle ear infection and changes in the vicinity of the tympanic membrane/lower horizontal ear canal, and tumours in the ear canal which cannot be dealt with either by Lateral Wall Resection or Vertical Canal Ablation. Also sometimes, due to financial reasons, a client may prefer surgery to lengthy courses of treatment, requiring several anaesthetics and ear flushings, with no guarantee of success at the outset. The surgeon first learnt the technique that was published in video format in the “In Practice” series around 1991. This involved the use of an osteotome to separate the ear canal from the bulla and also looking for the facial nerve and pulling it out of the way using penrose drain material. -
DSM III and ICD 9 Codes 11-2004
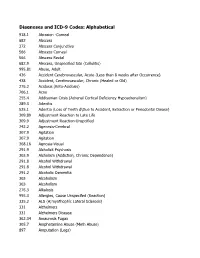
Diagnoses and ICD-9 Codes: Alphabetical 918.1 Abrasion -Corneal 682 Abscess 372 Abscess Conjunctiva 566 Abscess Corneal 566 Abscess Rectal 682.9 Abscess, Unspecified Site (Cellulitis) 995.81 Abuse, Adult 436 Accident Cerebrovascular, Acute (Less than 8 weeks after Occurrence) 438 Accident, Cerebrovascular, Chronic (Healed or Old) 276.2 Acidosis (Keto-Acidosis) 706.1 Acne 255.4 Addisonian Crisis (Adrenal Cortical Deficiency Hypoadrenalism) 289.3 Adenitis 525.1 Adentia (Loss of Teeth d\Due to Accident, Extraction or Periodontal Diease) 309.89 Adjustment Reaction to Late Life 309.9 Adjustment Reaction-Unspcified 742.2 Agenesis-Cerebral 307.9 Agitation 307.9 Agitation 368.16 Agnosia-Visual 291.9 Alcholick Psychosis 303.9 Alcholism (Addiction, Chronic Dependence) 291.8 Alcohol Withdrawal 291.8 Alcohol Withdrawal 291.2 Alcoholic Dementia 303 Alcoholism 303 Alcoholism 276.3 Alkalosis 995.3 Allergies, Cause Unspecifed (Reaction) 335.2 ALS (A;myothophic Lateral Sclerosis) 331 Alzheimers 331 Alzheimers Disease 362.34 Amaurosis Fugax 305.7 Amphetamine Abuse (Meth Abuse) 897 Amputation (Legs) 736.89 Amputation, Leg, Status Post (Above Knee, Below Knee) 736.9 Amputee, Site Unspecified (Acquired Deformity) 285.9 Anemia 284.9 Anemia Aplastic (Hypoplastic Bone Morrow) 280 Anemia Due to loss of Blood 281 Anemia Pernicious 280.9 Anemia, Iron Deficiency, Unspecified 285.9 Anemia, Unspecified (Normocytic, Not due to blood loss) 281.9 Anemia, Unspecified Deficiency (Macrocytic, Nutritional 441.5 Aneurysm Aortic, Ruptured 441.1 Aneurysm, Abdominal 441.3 Aneurysm,