Respiratory Examination Cardiac Examination Is an Essential Part of the Respiratory Assessment and Vice Versa
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nasal Septum Deviation by Age and Sex in a Study Population of Poles
Journal of Rhinolaryngo-Otologies, 2019, 7, 1-6 1 Nasal Septum Deviation by Age and Sex in a Study Population of Poles O. Wojas, P. Szczęsnowicz-Dąbrowska, A. Grzanka, E. Krzych-Fałta* and B . Samoliński Unit of Environmental Hazard Prevention and Allergology, Medical University of Warsaw, Poland Abstract: Introduction: Nasal septum deviation is found in nearly 79% of all autopsies. A displacement of the nasal septum is caused by developmental disorders, which result in growth disproportions between different skeletal structures, as well as hereditary factors, and injuries to the nose and the facial skeleton. Aims: This study aims is to estimate the incidence of nasal septum deviation in a study population of Poles, with a breakdown by age and sex. Subjects and method(s): The people involved in the study were a group of 950 randomly selected residents of a large city. The subjects were aged between 6 and 76 years. The method used in the study was anterior rhinoscopy in combination with clinical history taking. Results: The investigation revealed that the number of cases of nasal septum deviation diagnosed on the basis of anterior rhinoscopy increases steadily with age, from 15% in children aged 7-8 years to 39.7% in adults (p<0.05). The results of the study show that men are more frequently diagnosed with nasal septum deviations than women are (p<0.05). Conclusions: A relatively large percentage of nasal septum deviations was observed in a population of Poles, with a breakdown by age and sex. Keywords: Nasal cavity, nasal septum deviation. INTRODUCTION accompanies and contributes to diseases such as snoring, obstructive sleep apnea syndrome (OSAS) or The nasal cavity, enclosed by the inner surface of the chronic inflammatory paranasal sinus disease [5]. -

The Child with Altered Respiratory Status
Path: K:/LWW-BOWDEN-09-0101/Application/LWW-BOWDEN-09-0101-016.3d Date: 3rd July 2009 Time: 16:31 User ID: muralir 1BlackLining Disabled CHAPTER 16 The Child With Altered Respiratory Status Do you remember the Diaz fam- Case History leave Lela, the baby sister, ily from Chapter 9, in which with Claudia’s mother, Selma, Jose has trouble taking his asthma medication, and head to the hospital. and in Chapter 4, in which Jose’s little sister, At the hospital the emergency department Lela, expresses her personality even as a new- nurse observes Jose sitting cross-legged and born? Jose is 4 years old and was diagnosed leaning forward on his hands. His mouth is with asthma this past fall, about 6 months ago. open and he is breathing hard with an easily Since that time Claudia, his mother, has audible inspiratory wheeze. He is using his noticed several factors that trigger his asthma subclavicular accessory muscles with each including getting sick, pollen, and cold air. breath. His respiratory rate is 32 breaths per One evening following a warm early-spring minute, his pulse is 112 beats per minutes, day, Jose is outside playing as the sun sets and and he is afebrile. Claudia explains that he the air cools. When he comes inside he was fine; he was outside running and playing, begins to cough. Claudia sets up his nebulizer and then came in and began coughing and and gives him a treatment of albuterol, which wheezing, and she gave him an albuterol lessens his coughing. Within an hour, Jose is treatment. -
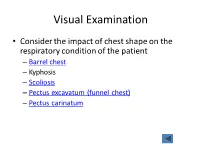
Visual Examination
Visual Examination • Consider the impact of chest shape on the respiratory condition of the patient – Barrel chest – Kyphosis – Scoliosis – Pectus excavatum (funnel chest) – Pectus carinatum Visual Assessment of Thorax • Thoracic scars from previous surgery • Chest symmetry • Use of accessory muscles • Bruising • In drawing of ribs • Flail segment www.nejm.org/doi/full/10.1056/NEJMicm0904437 • Paradoxical breathing /seesaw breathing • Pursed lip breathing • Nasal flaring Palpation • For vibration of secretion • Surgical emphysema • Symmetry of chest movement • Tactile vocal fremitus • Check for a tracheal tug • Palpate Nodes http://www.ncbi.nlm.nih.gov/books/NBK368/ https://m.youtube.com/watch?v=uzgdaJCf0Mk Auscultation • Is there any air entry? • Differentiate – Normal vesicular sounds – Bronchial breathing – Wheeze – Distinguish crackles • Fine • Coarse • During inspiration or expiration • Profuse or scanty – Absent sounds – Vocal resonance http://www.easyauscultation.com/lung-sounds.aspx Percussion • Tapping of the middle phalanx of the left middle finger with the right middle finger • Sounds should be resonant but may be – Hyper resonant – Dull – Stony Dull http://stanfordmedicine25.stanford.edu/the25/pulmonary.html Pathological Expansion Mediastinal Percussion Breath Further Process Displacement Note Sounds Examination Consolidation Reduced on None Dull Bronchial affected side breathing Vocal resonance Whispering pectoriloquy Collapse Reduced on Towards Dull Reduced None affected side affected side Pleural Reduced on Towards Stony dull Reduced/ Occasional rub effusion affected side opposite side Absent Empyema Asthma Reduced None Resonant Normal/ Wheeze throughout Reduced COPD Reduced None Resonant/ Normal/ Wheeze throughout Hyper-resonant Reduced Pulmonary Normal or None Normal Normal Bibasal crepitations Fibrosis reduced throughout Pneumothorax Reduced on Towards Hyper-resonant Reduced/ None affected side opposite side Absent http://www.cram.com/flashcards/test/lung-sounds-886428 sign up and test yourself.. -

Breathing Sounds – Determination of Extremely Low Spl
MATEC Web of Conferences 217, 03001 (2018) https://doi.org/10.1051/matecconf/201821703001 ICVSSD 2018 BREATHING SOUNDS – DETERMINATION OF EXTREMELY LOW SPL M. Harun1*, R. Teoh Y. S1, M. ‘A. A. Ahmad, M. Mohd. Mokji1, You K. Y1, S. A. R. Syed Abu Bakar1, P. I. Khalid1, S. Z. Abd. Hamid1 and R. Arsat1 1 School of Electrical Engineering, Universiti Teknologi Malaysia, *Email: [email protected] Phone: +6075535358 ABSTRACT Breathing sound is an extremely low SPL that results from inspiration and expiration process in the lung. Breathing sound can be used to diagnose persons with complications with breathing. Also, the sound can indicate the effectiveness of treatment of lung disease such as asthma. The purpose of this study was to identify SPL of breathing sounds, over six one octave center frequencies from 63 Hz to 4000 Hz, from the recorded breathing sounds in .wav files. Breathing sounds of twenty participants with normal weight BMI had been recorded in an audiometry room. The breathing sound was acquired in two states: at rest and after a 300 meters walk. Matlab had been used to process the breathing sounds that are in .wav files to come up with SPL (in dB). It has been found out that the SPL of breathing sound of all participants are positive at frequencies 63 Hz and 125 Hz. On the other hand, the SPL are all negatives at frequency 1000 Hz, 2000 Hz and 4000 Hz. In conclusion, SPL of breathing sounds of the participants, at frequencies 250 Hz and 500 Hz that have both positive and negative values are viable to be studied further for physiological and medicinal clues. -

THE DUBLIN MEDICAL SCHOOL and ITS INFLUENCE UPON MEDICINE in AMERICA1 by DAVID RIESMAN, M.D
THE DUBLIN MEDICAL SCHOOL AND ITS INFLUENCE UPON MEDICINE IN AMERICA1 By DAVID RIESMAN, M.D. PROFESSOR OF CLINICAL MEDICINE IN THE UNIVERSITY OF PENNSYLVANIA PHILADELPHIA, PA. HE Irish, a mixture of primitive universal genius like Robert Boyle, Ireland pre-Celtic peoples and of Goidelic did not produce a perpetuating body of Celts coming from the European learned men who made their influence felt T continent, developed in the early beyond the confines of the Green Island. Middle Ages, out of their own resources Of the history of Irish medicine in the and untouched in any marked degree by the Middle Ages, little is known and the all-pervading influence of Rome, a remark subject is largely an untilled field. Norman able indigenous culture. In particular they Moore (St. Barth. Hosp. Rep., 1875, it elaborated a native type of Christianity 145) has resuscitated a few of the original which with characteristic energy and manuscripts in the Irish language. Most wandering spirit they carried to Scotland, of them are translations from the works of to Northern England—to Northumbria—to Bernard de Gordon, especially from his France, to Belgium, and to Switzerland. “Lilium Medicinae”; of John of Gaddes- St. Columba, of Iona, and St. Columbanus, den’s “Rosa Anglica”; of the works of of Luxeuil, stand forth as the great militant Avicenna, of A verroes, of Isaac, and of the missionaries of that first flowering period Salernitan School. Much space is given to of Irish civilization. Although they and their the writings of Isidorus. This Isidorus is successors had to succumb to the greater the famous Spanish churchman, bishop might of Latin Christianity,2 they left of Seville, who not only was a master of dotted over Europe a number of large theology but a writer upon every branch of monasteries which became active centers of knowledge of his day. -

Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy
Medical Coverage Policy Effective Date ............................................. 7/10/2021 Next Review Date ....................................... 3/15/2022 Coverage Policy Number .................................. 0554 Diagnostic Nasal/Sinus Endoscopy, Functional Endoscopic Sinus Surgery (FESS) and Turbinectomy Table of Contents Related Coverage Resources Overview .............................................................. 1 Balloon Sinus Ostial Dilation for Chronic Sinusitis and Coverage Policy ................................................... 2 Eustachian Tube Dilation General Background ............................................ 3 Drug-Eluting Devices for Use Following Endoscopic Medicare Coverage Determinations .................. 10 Sinus Surgery Coding/Billing Information .................................. 10 Rhinoplasty, Vestibular Stenosis Repair and Septoplasty References ........................................................ 28 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence -
Pleurisy Dry and Exudative: Symptoms and Syndromes Based on Clinical-Instrumental and Laboratory Methods of Study
Topic: Pleurisy dry and exudative: symptoms and syndromes based on clinical-instrumental and laboratory methods of study. Syndrome of fluid and air accumulation in the pleural cavity in pathology of the respiratory system Objective 1. Patient S. 25 years old, has complaints of severe pain in the left half of the chest, exacerbated by deep breath, lack of air. He first felt sick 3 days ago, noticed a one-time increase in body temperature to 37,5°C. On examination: rapid superficial breathing, the left half of the chest is slower in the act of breathing. Clear pulmonary sound is determined by percussion. During auscultation, there is a pleural friction sound to the left, it is louder in the armpit. The pain increases with inhalation, decreases with lying on the side of pain. In the general clinical blood test - moderate leukocytosis, ESR - 17 mm / h. Questions: 1. What is the diagnosis? 2. What (all) data will the doctor receive when auscultating the patient's lungs with this pathology? 3. How can you distinguish the pleural friction sound from the pericardial friction sound? 4. What is the normal respiratory rate? What is the respiratory rate of rapid breathing? 5. What are the possible causes of this disease. Task 2. Patient M., 33 years old, has complaints of chills, fever up to 38,5°C for 3 days, dry cough, pain in the right half of the chest. The pain is exacerbated by breathing and coughing. Objectively: the skin is pale, the lips are cyanotic, the respiratory rate is up to 30 per minute, the right half of the chest is enlarged in volume, the intercostal spaces are smoothed. -

Clinical Usefulness of 'Vocal Fremitus' and 'Vocal Resonance'
RESEARCH Clinical usefulness of ‘vocal fremitus’ and ‘vocal resonance’ Kyaw San Hla MMedSc, MRCP, FRACP, is Senior Lecturer and staff physician, James Cook University, Mackay Base GP perceptions and practice Hospital, Queensland. kyaw. [email protected] Assessment of vocal fremitus (VF) and vocal resonance The study was approved by the Ethics Committee at Mackay (VR) (whereby vocal vibrations are felt or heard during Base Hospital. a clinical examination) is an established part of physical examination of the respiratory system. Textbooks on Results clinical examination include these procedures as part of Sixty-seven responses were obtained (64 GPs and three the standard method.1–3 general practice registrars), providing a response rate of approximately 70%. Forty-four respondents (65.7%) Undergraduate and postgraduate candidates are required rarely performed VF/VR as part of routine chest examination to perform VF and VR when they undertake qualifying (Figure 1). 50 44 assessments, however the reliability of findings from More than half (53.7%) 40 these procedures is controversial.4 It is also unusual to disagreed with the statement 30 see experienced doctors performing VF/VR during actual that ‘routine inclusion of either chest examination. The author of the only identifiable study VF or VR on chest examination Count 20 9 on clinicians’ attitudes toward VF/VR (which had only 14 is desirable’ (with 11.9% strongly 10 6 2 3 3 respondents) remarked ‘it will be rare to see physicians disagreeing). More than a quarter 0 near about about about about rarely doing both or even one of them although the majority has (28%) remained neutral. -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Respiratory Examination Hand-Out
Respiratory Examination A thorough respiratory examination should include the following aspects. Underlined are the areas of highest importance which should always be considered. General Inspection Patient wellbeing: stable, alert, comfortable, breathless, cachexia (cancer, emphysema), cushingoid (steroid use). Breathing: use of accessory muscles (severe asthma, COPD, pneumothorax) , pursed lip breathing (keeps open small airways by increasing thoracic pressure during expiration in severe emphysema), stridor (upper airway obstruction), wheeze, cough, prolonged expiratory phase. Around the bed / couch: oxygen, medications, sputum samples, cigarettes Hands Generalised fine tremor (beta agonists), CO2 retention flap, perfusion (eg cyanosis), small muscle wasting (eg Pancoast tumour), clubbing (IPF, lung cancer, bronchiectasis) tar staining. Pulse and Respiratory rate Pulse: rate and rhythm, bounding pulse (CO2 retention) Respiratory rate: tachypnoea (hyperventilation, pneumothorax, anxiety) bradypnoea (sedation) Head and Neck Face: cushingoid, plethoric (CO2 retention) Eyes: conjunctival pallor (anaemia of chronic disease) Mouth: central cyanosis Neck: JVP height (raised in cor pulmonale) tracheal tug, tracheal deviation (pleural effusion, pneumothorax, collapse), lymphadenopathy 1 MISSION ABC Respiratory Examination v1: 19th Sept 2017 Review Date: 19/09/2019 Version 1.0 2019 Chest – both anteriorly and posteriorly Inspection: Asymmetry (previous surgery, spinal deformities), scars (previous surgery), shape Palpation: Both supra-mammary -

Septal Deviation Operation Informed Consent Form
SEPTAL DEVIATION OPERATION INFORMED CONSENT FORM FIRST DOCUMEN RB.FR. PUBLIS REVISION REVISION PAGE 01.02.2010 09.12.2015 1 1/6 T NO 15 HING DATE NO NO DATE Revision Cause: PATIENT’S Name Surname:……………………………………………... Birthdate :…………………………………………. Hospital Admission Date:………………………………. Hospitalization Date:…………………………………… Protocol Number:…………………………………….. Telephone Number:……………………………………… Address:………………………………………………………………………………………………………… …………………………………………………………………………………………………………………… Please read this form carefully and answer the questions. As a result of the examinations, it has been decided that you should undergo surgical intervention because of “septal deviation”. Before the procedure, your doctor will give you information about the course and the different forms of the procedure and the risks involved. Accordingly, you will be free to decide on the interventions. This written form is intended to provide you with basic information about the intervention and associated complications (problems that may occur during or after the procedure). What you should know about your disease: The nasal septum deviation (see figure) occurs due to the development of deformities of the facial bones, as well as fractures of the nasal bone that may occur during birth. If the deviation is causing the following problems, surgery is required: 1. Difficulty in nasal respiration 2. Drying, burning sensation, feeling of foreign body in the throat due to continuous oral breathing 3. Snoring, sleep acnea (occasionally) 4. Head/face ache 5. Recurrent sinusitis, 6. Laryngitis and bronchi inflammation 7. İnfection of the Eustachian tube and tendency to middle ear infections . In some sinus operations and certain types of nasal bleeding, nasal septum deviation surgery may be necessary. SEPTAL DEVIATION OPERATION INFORMED CONSENT FORM FIRST DOCUMEN RB.FR. -
PALS Helpful Hints 2015 Guidelines - December 2016 Mandatory Precourse Assessment at Least 70% Pass
PALSPALS Helpful Helpful Hints Courtesy Hints are of CourtesyKey Medical of Resources, Key Medical Inc. Resources, www.cprclassroom.com Inc. PALS Helpful Hints 2015 Guidelines - December 2016 Mandatory precourse assessment at least 70% pass. Bring proof of completion to class. The PALS exam is 50 questions. Passing score is 84% or you may miss 8 questions. All AHA exams are now open resource, so you may use your books and/or handouts for the exam. For those persons taking PALS for the first time or updating/renewing with a current card, exam remediation is permitted should you miss more than 8 questions on the exam. Viewing the PALS book ahead of time with the online resources is very helpful. The American Heart Association link is www.heart.org/eccstudent has a pre-course self- assessment, supplementary written materials and videos. The code for these online resources is in the PALS Provider manual page ii. The code is PALS15. Basic Dysrhythmia knowledge is required. The exam has at least 5 strips to interpret. The course is a series of video segments then skills. The course materials well prepare you for the exam. Basic Dysrhythmias knowledge is required in relation to asystole, ventricular fibrillation, tachycardias in general and bradycardias in general. You do not need to know the ins and outs of each and every one. Tachycardias need to differentiate wide complex (ventricular tachycardia) and narrow complex (supraventricular tachycardia or SVT). Airway - child is grunting - immediate intervention. Airway - deteriorates after oral airway, next provide bag-mask ventilation. Airway - snoring with poor air entry bilaterally - reposition, oral airway.