Clinical Usefulness of 'Vocal Fremitus' and 'Vocal Resonance'
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Respiratory Examination Cardiac Examination Is an Essential Part of the Respiratory Assessment and Vice Versa
Respiratory examination Cardiac examination is an essential part of the respiratory assessment and vice versa. # Subject steps Pictures Notes Preparation: Pre-exam Checklist: A Very important. WIPE Be the one. 1 Wash your hands. Wash your hands in Introduce yourself to the patient, confirm front of the examiner or bring a sanitizer with 2 patient’s ID, explain the examination & you. take consent. Positioning of the patient and his/her (Position the patient in a 3 1 2 Privacy. 90 degree sitting position) and uncover Exposure. full exposure of the trunk. his/her upper body. 4 (if you could not, tell the examiner from the beginning). 3 4 Examination: General appearance: B (ABC2DEVs) Appearance: young, middle aged, or old, Begin by observing the and looks generally ill or well. patient's general health from the end of the bed. Observe the patient's general appearance (age, Around the bed I can't state of health, nutritional status and any other see any medications, obvious signs e.g. jaundice, cyanosis, O2 mask, or chest dyspnea). 1 tube(look at the lateral sides of chest wall), metered dose inhalers, and the presence of a sputum mug. 2 Body built: normal, thin, or obese The patient looks comfortable and he doesn't appear short of breath and he doesn't obviously use accessory muscles or any heard Connections: such as nasal cannula wheezes. To determine this, check for: (mention the medications), nasogastric Dyspnea: Assess the rate, depth, and regularity of the patient's 3 tube, oxygen mask, canals or nebulizer, breathing by counting the respiratory rate, range (16–25 breaths Holter monitor, I.V. -
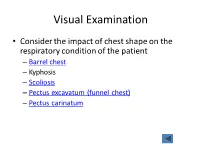
Visual Examination
Visual Examination • Consider the impact of chest shape on the respiratory condition of the patient – Barrel chest – Kyphosis – Scoliosis – Pectus excavatum (funnel chest) – Pectus carinatum Visual Assessment of Thorax • Thoracic scars from previous surgery • Chest symmetry • Use of accessory muscles • Bruising • In drawing of ribs • Flail segment www.nejm.org/doi/full/10.1056/NEJMicm0904437 • Paradoxical breathing /seesaw breathing • Pursed lip breathing • Nasal flaring Palpation • For vibration of secretion • Surgical emphysema • Symmetry of chest movement • Tactile vocal fremitus • Check for a tracheal tug • Palpate Nodes http://www.ncbi.nlm.nih.gov/books/NBK368/ https://m.youtube.com/watch?v=uzgdaJCf0Mk Auscultation • Is there any air entry? • Differentiate – Normal vesicular sounds – Bronchial breathing – Wheeze – Distinguish crackles • Fine • Coarse • During inspiration or expiration • Profuse or scanty – Absent sounds – Vocal resonance http://www.easyauscultation.com/lung-sounds.aspx Percussion • Tapping of the middle phalanx of the left middle finger with the right middle finger • Sounds should be resonant but may be – Hyper resonant – Dull – Stony Dull http://stanfordmedicine25.stanford.edu/the25/pulmonary.html Pathological Expansion Mediastinal Percussion Breath Further Process Displacement Note Sounds Examination Consolidation Reduced on None Dull Bronchial affected side breathing Vocal resonance Whispering pectoriloquy Collapse Reduced on Towards Dull Reduced None affected side affected side Pleural Reduced on Towards Stony dull Reduced/ Occasional rub effusion affected side opposite side Absent Empyema Asthma Reduced None Resonant Normal/ Wheeze throughout Reduced COPD Reduced None Resonant/ Normal/ Wheeze throughout Hyper-resonant Reduced Pulmonary Normal or None Normal Normal Bibasal crepitations Fibrosis reduced throughout Pneumothorax Reduced on Towards Hyper-resonant Reduced/ None affected side opposite side Absent http://www.cram.com/flashcards/test/lung-sounds-886428 sign up and test yourself.. -
Pleurisy Dry and Exudative: Symptoms and Syndromes Based on Clinical-Instrumental and Laboratory Methods of Study
Topic: Pleurisy dry and exudative: symptoms and syndromes based on clinical-instrumental and laboratory methods of study. Syndrome of fluid and air accumulation in the pleural cavity in pathology of the respiratory system Objective 1. Patient S. 25 years old, has complaints of severe pain in the left half of the chest, exacerbated by deep breath, lack of air. He first felt sick 3 days ago, noticed a one-time increase in body temperature to 37,5°C. On examination: rapid superficial breathing, the left half of the chest is slower in the act of breathing. Clear pulmonary sound is determined by percussion. During auscultation, there is a pleural friction sound to the left, it is louder in the armpit. The pain increases with inhalation, decreases with lying on the side of pain. In the general clinical blood test - moderate leukocytosis, ESR - 17 mm / h. Questions: 1. What is the diagnosis? 2. What (all) data will the doctor receive when auscultating the patient's lungs with this pathology? 3. How can you distinguish the pleural friction sound from the pericardial friction sound? 4. What is the normal respiratory rate? What is the respiratory rate of rapid breathing? 5. What are the possible causes of this disease. Task 2. Patient M., 33 years old, has complaints of chills, fever up to 38,5°C for 3 days, dry cough, pain in the right half of the chest. The pain is exacerbated by breathing and coughing. Objectively: the skin is pale, the lips are cyanotic, the respiratory rate is up to 30 per minute, the right half of the chest is enlarged in volume, the intercostal spaces are smoothed. -
Gas Exchange and Respiratory Function
LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 484 Aptara Gas Exchange and 5 Respiratory Function Applying Concepts From NANDA, NIC, • Case Study and NOC A Patient With Impaired Cough Reflex Mrs. Lewis, age 77 years, is admitted to the hospital for left lower lobe pneumonia. Her vital signs are: Temp 100.6°F; HR 90 and regular; B/P: 142/74; Resp. 28. She has a weak cough, diminished breath sounds over the lower left lung field, and coarse rhonchi over the midtracheal area. She can expectorate some sputum, which is thick and grayish green. She has a history of stroke. Secondary to the stroke she has impaired gag and cough reflexes and mild weakness of her left side. She is allowed food and fluids because she can swallow safely if she uses the chin-tuck maneuver. Visit thePoint to view a concept map that illustrates the relationships that exist between the nursing diagnoses, interventions, and outcomes for the patient’s clinical problems. LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 485 Aptara Nursing Classifications and Languages NANDA NIC NOC NURSING DIAGNOSES NURSING INTERVENTIONS NURSING OUTCOMES INEFFECTIVE AIRWAY CLEARANCE— RESPIRATORY MONITORING— Return to functional baseline sta- Inability to clear secretions or ob- Collection and analysis of patient tus, stabilization of, or structions from the respiratory data to ensure airway patency improvement in: tract to maintain a clear airway and adequate gas exchange RESPIRATORY STATUS: AIRWAY PATENCY—Extent to which the tracheobronchial passages remain open IMPAIRED GAS -

Community-Acquired Pneumonia in Adults: Diagnostic Reliability of Physical Examination Techniques and Their Teaching in Academia
James Madison University JMU Scholarly Commons Physician Assistant Capstones The Graduate School Fall 12-14-2018 Community-acquired pneumonia in adults: Diagnostic reliability of physical examination techniques and their teaching in academia Amber Tordoff James Madison University Lauren A. Williams James Madison University Follow this and additional works at: https://commons.lib.jmu.edu/pacapstones Part of the Bacteria Commons, Bacterial Infections and Mycoses Commons, Diagnosis Commons, Investigative Techniques Commons, Medical Pathology Commons, Respiratory Tract Diseases Commons, Virus Diseases Commons, and the Viruses Commons Recommended Citation Tordoff AL, Williams LA. Community-Acquired Pneumonia in Adults: Diagnostic Reliability of Physical Examination Techniques and their Teaching in Academia. JMU Scholarly Commons Physician Assistant Capstones. https://commons.lib.jmu.edu/pacapstones/44/. Published December 12, 2018. This Presentation is brought to you for free and open access by the The Graduate School at JMU Scholarly Commons. It has been accepted for inclusion in Physician Assistant Capstones by an authorized administrator of JMU Scholarly Commons. For more information, please contact [email protected]. Community-Acquired Pneumonia in Adults: Diagnostic Reliability of Physical Examination Techniques and their Teaching in Academia Amber Tordoff, PA-S and Lauren Williams, PA-S, James Madison University, Harrisonburg, Virginia _____________________________________________________________________________________ ABSTRACT Background: -
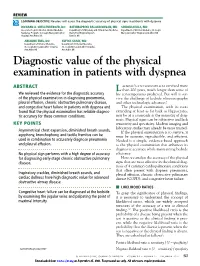
Diagnostic Value of the Physical Examination in Patients with Dyspnea
REVIEW LEARNING OBJECTIVE: Readers will assess the diagnostic accuracy of physical signs in patients with dyspnea RICHARD A. SHELLENBERGER, DO BATHMAPRIYA BALAKRISHNAN, MD SINDHU AVULA, MD Associate Program Director, Internal Medicine Department of Pulmonary and Critical Care Medicine, Department of Internal Medicine, St. Joseph Residency Program, St. Joseph Mercy Ann Arbor Henry Ford Hospital System, Mercy Ann Arbor Hospital, Ann Arbor, MI Hospital, Ann Arbor, MI Detroit, MI ARIADNE EBEL, DO SUFIYA SHAIK, MD Department of Internal Medicine, Department of Internal Medicine, St. Joseph Mercy Ann Arbor Hospital, St. Joseph Mercy Ann Arbor Hospital, Ann Arbor, MI Ann Arbor, MI Diagnostic value of the physical examination in patients with dyspnea ABSTRACT aennec’s stethoscope has survived more L than 200 years, much longer than some of We reviewed the evidence for the diagnostic accuracy his contemporaries predicted. But will it sur- of the physical examination in diagnosing pneumonia, vive the challenge of bedside ultrasonography pleural effusion, chronic obstructive pulmonary disease, and other technologic advances? and congestive heart failure in patients with dyspnea and The physical examination, with its roots found that the physical examination has reliable diagnos- extending at least as far back as Hippocrates, tic accuracy for these common conditions. may be at a crossroads as the mainstay of diag- nosis. Physical signs can be subjective and lack KEY POINTS sensitivity and specificity. Modern imaging and laboratory studies may already be more trusted. Asymmetrical chest expansion, diminished breath sounds, If the physical examination is to survive, it egophony, bronchophony, and tactile fremitus can be must be accurate, reproducible, and efficient. -

Physical Examination of the Adult Patient with Respiratory Diseases: Inspection and Palpation
Eur Respir J, 1995, 8, 1584–1593 Copyright ERS Journals Ltd 1995 DOI: 10.1183/09031936.95.08091584 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 SERIES 'CHEST PHYSICAL EXAMINATION' Edited by J.C. Yernault Physical examination of the adult patient with respiratory diseases: inspection and palpation B. Maitre, T. Similowski, J-P. Derenne Physical examination of the adult patient with respiratory diseases: inspection and pal- Service de Pneumologie et de Réanimation, pation. B. Maitre, T. Similowski, J-P. Derenne. ©ERS Journals Ltd 1995. Groupe Hospitalier Pitié-Salpêtrière, Paris, ABSTRACT: Inspection of the thorax identifies the breathing position adopted by France. the patient, the shape of the thorax, the dynamics of respiration (breathing pat- tern, symmetry of expansion, mechanics and synchrony of rib cage and abdominal Correspondence: T. Similowski movements). Inspection of the neck adds useful information, particularly with Service de Pneumologie et de Réanimation respect to the dynamics of breathing. Palpation ascertains the signs suggested by Groupe Hospitalier Pitié-Salpêtrière inspection with respect to the mechanics of breathing. It also assesses the state of 47-83 Bd de l'Hôpital 75651 Paris Cedex 13 the pleura and pulmonary parenchyma by studying the tactile fremitus. It inte- France grates extrarespiratory signs, such as enlarged lymph nodes or breast abnorma- lities. Extrathoracic respiratory signs should also be systematically looked for, Keywords: Clinical examination including cyanosis, finger deformation, pulsus paradoxus, and pursed lips breath- inspection ing. palpation Interobserver agreement about respiratory signs has repeatedly been studied, and respiratory system generally found to be low, as are clinical-functional correlations. -

Approach to Chronic Cough and Atopy Year 3 Clerkship Guide, Family Medicine Department Schulich School of Medicine and Dentistry ______Objectives 1
Approach to Chronic Cough and Atopy Year 3 Clerkship Guide, Family Medicine Department Schulich School of Medicine and Dentistry _____________________________________________________________________________________________ Objectives 1. Understand the principles of management for allergic conditions 2. Be able to conduct an appropriate history and physical exam for someone with a complaint of chronic cough. 3. Be able to outline a differential diagnosis for chronic cough. 4. Identify appropriate investigations for a child complaining of chronic cough. 5. Develop an approach for management of asthma. 6. Be able to distinguish between seborrheic dermatitis and atopic dermatitis. 7. Be able to identify other atopic conditions (allergic rhinitis and atopic dermatitis), order appropriate investigations for diagnosis and outline a plan for management. 8. Understand the correct management for an acute exacerbation of asthma. 9. Be able to explain and demonstrate when and how to use a puffer (see module) 10. Atopy refers to a genetic predisposition to the type 1 hypersensitivity reactions that most commonly manifest as allergic rhinitis, asthma, and atopic dermatitis. Approach to Chronic Cough History: When taking a history, make sure to identify the onset and nature of the cough, including whether it is productive, if there is associated dyspnea, what the cough sounds like and if there are any other symptoms (e.g. rhinorrhea, allodynia, malaise, headache, or fever) which might indicate an infectious cause. Determine what the circumstances were at the onset of the cough, as a cough that onset while playing or eating may lead to suspicion about a foreign body in the airway. Ask about any medications that may have been taken to control the cough and whether they were effective. -

Physical Diagnosis the Pulmonary Exam What Should We Know About the Examination of the Chest?
PHYSICAL DIAGNOSIS THE PULMONARY EXAM WHAT SHOULD WE KNOW ABOUT THE EXAMINATION OF THE CHEST? • LANDMARKS • PERTINENT VOCABULARY • SYMPTOMS • SIGNS • HOW TO PERFORM AN EXAM • HOW TO PRESENT THE INFORMATION • HOW TO FORMULATE A DIFFERENTIAL DIAGNOSIS IMPORTANT TOPOGRAPHY OF THE CHEST TOPOGRAPHY OF THE BACK LOOK AT THE PATIENT • RESPIRATORY DISTRESS • ANXIOUS • CLUTCHING • ACCESSORY MUSCLES •CYANOSIS • GASPING • STRIDOR • CLUBBING TYPES OF BODY HABITUS WHAT IS A BARRELL CHEST? • THORACIC INDEX – RATIO OF THE ANTERIORPOSTERIOR TO LATERAL DIAMETER NORMAL 0.70 – 0.75 IN ADULTS - >0.9 IS CONSIDERED ABNORMAL • NORMALS - ILLUSION •COPD AM J MED 25:13-22,1958 PURSED – LIPS BREATHING • COPD – DECREASES DYSPNEA • DECREASES RR • INCREASES TIDAL VOLUME • DECREASES WORK OF BREATHING CHEST 101:75-78, 1992 WHITE NOISE (NOISY BREATHING) • THIS NOISE CAN BE HEARD AT THE BEDSIDE WITHOUT THE STETHOSCOPE • LACKS A MUSICAL PITCH • AIR TURBULENCE CAUSED BY NARROWED AIRWAYS • CHRONIC BRONCHITIS CHEST 73:399-412, 1978 RESPIRATORY ALTERNANS • NORMALLY BOTH CHEST AND ABDOMEN RISE DURING INSPIRATION • PARADOXICAL RESPIRATION IMPLIES THAT DURING INSPIRATION THE CHEST RISES AND THE ABDOMEN COLLAPSES • IMPENDING MUSCLE FATIGUE DO NOT FORGET THE TRACHEA • TRACHEAL DEVIATION • AUSCULTATE - STRIDOR • TRACHEAL TUG (OLIVERS SIGN) – DOWNWARD DISPLACEMENT OF THE CRICOID CARTILAGE WITH VENTRICULAR CONTRACTION – OBSERVED IN PATIENTS WITH AN AORTIC ARCH ANEURYSM • TRACHEAL TUG (CAMPBELL’S SIGN) – DOWNWARD DISPACEMENT OF THE THYROID CARTILAGE DURING INSPIRATION – SEEN IN PATIENTS -

Respiratory Examination Learnpediatrics.Com Narration Written by Drs
Respiratory Examination Learnpediatrics.com Narration Written by Drs. C. Taylor, P. Gfeller, and T. Ring Introduction Hello and welcome to the respiratory module. I will be accompanying you through examination of the respiratory system in a cooperative child. Remember you must always adjust your approach and be flexible when examining a child, taking into consideration their age, personality and how well they are. A complete examination of the respiratory system must always include an examination of the ears, nose and throat. Acute Assessment Your first encounter with a patient allows you to make some general observations. Most essential in immediate observation is the acute assessment of the child. This information determines the pace, the focus and the thoroughness of the exam. In emergency situations, an acute assessment may require direct medical intervention prior to the commencement of any further historical or physical investigations. If the child appears well you will likely have time to complete a thorough history and physical examination. Keep in mind that much of the diagnosis of the respiratory problem in a child is formed through your observations. In your initial observations you should obtain a general impression of the state of the child’s health, observe the nature and effort of his or her breathing during both inspiration and expiration. Also observe any signs of respiratory problems, noisy breathing, the quality of any cough and the allergic salute or shiners. It is also important to make a quick assessment of the parent accompanying the child. You can gain valuable information and build rapport by recognizing the emotional state of the parent. -

Pulmonary and Thorax Exam FACILITATOR & STUDENT COPY
PATIENT CENTERED MEDICINE - 1 PCM-1 Physical Exam Skills Session: Pulmonary and Thorax Exam FACILITATOR & STUDENT COPY GOALS & OUTCOMES: 1. To introduce basic examination techniques of the thorax and the pulmonary system and stress the applied physiology as well as to review the applied anatomy. 2. To introduce the use of the stethoscope ASSIGNMENTS DUE FOR THIS SESSION: 1. Bates' Guide to Physical Examination and History Taking. 11th Edition. The Thorax and Lungs: Anatomy and Physiology, pp. 293-299, Techniques of Examination, pp. 305-318. 2. PCM Basic Examination- Details: View: Lung Video and Thorax Video Review the Using Diagnostic Equipment video 3. Bring your stethoscope with you to learn its use in the pulmonary exam ASSIGNMENTS DUE FOR NEXT WEEK: 1) Practice the skills learned on friends, family, pets, etc. SESSION ACTIVITIES: SUGGESTED TIMELINE: 1) Watch the high yield demonstration with course 45 minutes faculty in lecture hall as a group. 2) Examine each other in small groups guided by 60 minutes faculty. Thorax/Pulmonary Exam Page 1 of 6 BACKGROUND – TO BE READ BEFORE COMING TO THE SMALL GROUP This session is a continuation of the physical exam sessions representing a collaborative effort between the two courses Patient Centered Medicine 1 and Structure of the Human Body. Process: 1. Meet in the lecture hall for the high yield demonstration. 2. Then you will have an assigned time at which to report to the clinical skills center. Typically, there are three waves of assigned times usually 1:00 p.m., 2:00 p.m. and 3:00 p.m. -

1997 Documentation Guidelines for Evaluation and Management Services
1997 DOCUMENTATION GUIDELINES FOR EVALUATION AND MANAGEMENT SERVICES TABLE OF CONTENTS Introduction ....................................................................................................…… 2 What Is Documentation and Why Is it Important?............................………. 2 What Do Payers Want and Why? .......................................................……… 2 General Principles of Medical Record Documentation ..................................... 3 Documentation of E/M Services........................................................................... 4 Documentation of History .................................................................................... 5 Chief Complaint (CC) ..................................................................................... 6 History of Present Illness (HPI) ..................................................................... 7 Review of Systems (ROS) .............................................................................. 8 Past, Family and/or Social History (PFSH) ................................................... 9 Documentation of Examination ........................................................................... 10 General Multi-System Examinations ............................................................ 11 Single Organ System Examinations ............................................................ 12 Content and Documentation Requirements ................................................ 13 General Multi-System Examination ………..............................................