Problems in Family Practice Hemoptysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Obstructive Sleep Apnea
ObSTruCTIve Sleep ApneA provider’s guide to diagnose and code sleep apnea Sleep apnea is a common disorder that by When reviewing these symptoms it is helpful definition is characterized by a reduction in to clarify the history with the patient’s sleeping normal breathing during hours of sleep, often partner, when available. The most useful symptom related to the collapse of the soft tissues in the for identifying patients with OSA is nocturnal back of the throat. Obstructive sleep apnea (OSA) choking or gasping. Snoring alone is not a is the most common sleeping disorder. It has been diagnostic predictor for OSA. However, the lack diagnosed in 3 to 7% of Americans. It is estimated of snoring and/or presence of apnea reduce the that 20% of the entire American population has not likelihood of an OSA diagnosis. been diagnosed. Quantification of the patient’s perception Independent risk factors for of daytime sleepiness and/or fatigue is an important historical finding. This can be developing OSA include: determined by using the Epworth Sleepiness › Obesity (BMI > 30 kg/m2) Scale (epworthsleepinessscale.com). A score of 10 supports the hypothesis of excessive daytime › African – American race sleepiness, which should prompt the clinician to › Male gender have the patient tested for OSA. › Advancing age › Cranio – facial anomalies The physical examination should focus on: Smoking › 1. Review of the oral airway, specifically: › Controlled substance use and alcohol intake the size of the uvula and tonsils, and › Chronic medical conditions such as: the presence of nasal septal deviation end-stage renal disease, congestive heart failure, 2. -

Respiratory Examination Cardiac Examination Is an Essential Part of the Respiratory Assessment and Vice Versa
Respiratory examination Cardiac examination is an essential part of the respiratory assessment and vice versa. # Subject steps Pictures Notes Preparation: Pre-exam Checklist: A Very important. WIPE Be the one. 1 Wash your hands. Wash your hands in Introduce yourself to the patient, confirm front of the examiner or bring a sanitizer with 2 patient’s ID, explain the examination & you. take consent. Positioning of the patient and his/her (Position the patient in a 3 1 2 Privacy. 90 degree sitting position) and uncover Exposure. full exposure of the trunk. his/her upper body. 4 (if you could not, tell the examiner from the beginning). 3 4 Examination: General appearance: B (ABC2DEVs) Appearance: young, middle aged, or old, Begin by observing the and looks generally ill or well. patient's general health from the end of the bed. Observe the patient's general appearance (age, Around the bed I can't state of health, nutritional status and any other see any medications, obvious signs e.g. jaundice, cyanosis, O2 mask, or chest dyspnea). 1 tube(look at the lateral sides of chest wall), metered dose inhalers, and the presence of a sputum mug. 2 Body built: normal, thin, or obese The patient looks comfortable and he doesn't appear short of breath and he doesn't obviously use accessory muscles or any heard Connections: such as nasal cannula wheezes. To determine this, check for: (mention the medications), nasogastric Dyspnea: Assess the rate, depth, and regularity of the patient's 3 tube, oxygen mask, canals or nebulizer, breathing by counting the respiratory rate, range (16–25 breaths Holter monitor, I.V. -

Hemoptysis in Children
R E V I E W A R T I C L E Hemoptysis in Children G S GAUDE From Department of Pulmonary Medicine, JN Medical College, Belgaum, Karnataka, India. Correspondence to: Dr G S Gaude, Professor and Head, Department of Pulmonary Medicine, J N Medical College, Belgaum 590 010, Karnataka, India. [email protected] Received: November, 11, 2008; Initial review: May, 8, 2009; Accepted: July 27, 2009. Context: Pulmonary hemorrhage and hemoptysis are uncommon in childhood, and the frequency with which they are encountered by the pediatrician depends largely on the special interests of the center to which the child is referred. Diagnosis and management of hemoptysis in this age group requires knowledge and skill in the causes and management of this infrequently occurring potentially life-threatening condition. Evidence acquisition: We reviewed the causes and treatment options for hemoptysis in the pediatric patient using Medline and Pubmed. Results: A focused physical examination can lead to the diagnosis of hemoptysis in most of the cases. In children, lower respiratory tract infection and foreign body aspiration are common causes. Chest radiographs often aid in diagnosis and assist in using two complementary diagnostic procedures, fiberoptic bronchoscopy and high-resolution computed tomography. The goals of management are threefold: bleeding cessation, aspiration prevention, and treatment of the underlying cause. Mild hemoptysis often is caused by an infection that can be managed on an outpatient basis with close monitoring. Massive hemoptysis may require additional therapeutic options such as therapeutic bronchoscopy, angiography with embolization, and surgical intervention such as resection or revascularization. Conclusions: Hemoptysis in the pediatric patient requires prompt and thorough evaluation and treatment. -

Visual Examination
Visual Examination • Consider the impact of chest shape on the respiratory condition of the patient – Barrel chest – Kyphosis – Scoliosis – Pectus excavatum (funnel chest) – Pectus carinatum Visual Assessment of Thorax • Thoracic scars from previous surgery • Chest symmetry • Use of accessory muscles • Bruising • In drawing of ribs • Flail segment www.nejm.org/doi/full/10.1056/NEJMicm0904437 • Paradoxical breathing /seesaw breathing • Pursed lip breathing • Nasal flaring Palpation • For vibration of secretion • Surgical emphysema • Symmetry of chest movement • Tactile vocal fremitus • Check for a tracheal tug • Palpate Nodes http://www.ncbi.nlm.nih.gov/books/NBK368/ https://m.youtube.com/watch?v=uzgdaJCf0Mk Auscultation • Is there any air entry? • Differentiate – Normal vesicular sounds – Bronchial breathing – Wheeze – Distinguish crackles • Fine • Coarse • During inspiration or expiration • Profuse or scanty – Absent sounds – Vocal resonance http://www.easyauscultation.com/lung-sounds.aspx Percussion • Tapping of the middle phalanx of the left middle finger with the right middle finger • Sounds should be resonant but may be – Hyper resonant – Dull – Stony Dull http://stanfordmedicine25.stanford.edu/the25/pulmonary.html Pathological Expansion Mediastinal Percussion Breath Further Process Displacement Note Sounds Examination Consolidation Reduced on None Dull Bronchial affected side breathing Vocal resonance Whispering pectoriloquy Collapse Reduced on Towards Dull Reduced None affected side affected side Pleural Reduced on Towards Stony dull Reduced/ Occasional rub effusion affected side opposite side Absent Empyema Asthma Reduced None Resonant Normal/ Wheeze throughout Reduced COPD Reduced None Resonant/ Normal/ Wheeze throughout Hyper-resonant Reduced Pulmonary Normal or None Normal Normal Bibasal crepitations Fibrosis reduced throughout Pneumothorax Reduced on Towards Hyper-resonant Reduced/ None affected side opposite side Absent http://www.cram.com/flashcards/test/lung-sounds-886428 sign up and test yourself.. -

Problems in Family Practice
problems in Family Practice Coughing in Childhood Hyman Sh ran d , M D Cambridge, M assachusetts Coughing in childhood is a common complaint involving a wide spectrum of underlying causes which require a thorough and rational approach by the physician. Most children who cough have relatively simple self-limiting viral infections, but some may have serious disease. A dry environment, allergic factors, cystic fibrosis, and other major illnesses must always be excluded. A simple clinical approach, and the sensible use of appropriate investigations, is most likely to succeed in finding the cause, which can allow precise management. The cough reflex as part of the defense mechanism of the respiratory tract is initiated by mucosal changes, secretions or foreign material in the pharynx, larynx, tracheobronchial Table 1. Persistent Cough — Causes in Childhood* tree, pleura, or ear. Acting as the “watchdog of the lungs,” the “good” cough prevents harmful agents from Common Uncommon Rare entering the respiratory tract; it also helps bring up irritant material from Environmental Overheating with low humidity the airway. The “bad” cough, on the Allergens other hand, serves no useful purpose Pollution Tobacco smoke and, if persistent, causes fatigue, keeps Upper Respiratory Tract the child (and parents) awake, inter Recurrent viral URI Pertussis Laryngeal stridor feres with feeding, and induces vomit Rhinitis, Pharyngitis Echo 12 Vocal cord palsy Allergic rhinitis Nasal polyp Vascular ring ing. It is best suppressed. Coughs and Prolonged use of nose drops Wax in ear colds constitute almost three quarters Sinusitis of all illness in young children. The Lower Respiratory Tract Asthma Cystic fibrosis Rt. -
Pleurisy Dry and Exudative: Symptoms and Syndromes Based on Clinical-Instrumental and Laboratory Methods of Study
Topic: Pleurisy dry and exudative: symptoms and syndromes based on clinical-instrumental and laboratory methods of study. Syndrome of fluid and air accumulation in the pleural cavity in pathology of the respiratory system Objective 1. Patient S. 25 years old, has complaints of severe pain in the left half of the chest, exacerbated by deep breath, lack of air. He first felt sick 3 days ago, noticed a one-time increase in body temperature to 37,5°C. On examination: rapid superficial breathing, the left half of the chest is slower in the act of breathing. Clear pulmonary sound is determined by percussion. During auscultation, there is a pleural friction sound to the left, it is louder in the armpit. The pain increases with inhalation, decreases with lying on the side of pain. In the general clinical blood test - moderate leukocytosis, ESR - 17 mm / h. Questions: 1. What is the diagnosis? 2. What (all) data will the doctor receive when auscultating the patient's lungs with this pathology? 3. How can you distinguish the pleural friction sound from the pericardial friction sound? 4. What is the normal respiratory rate? What is the respiratory rate of rapid breathing? 5. What are the possible causes of this disease. Task 2. Patient M., 33 years old, has complaints of chills, fever up to 38,5°C for 3 days, dry cough, pain in the right half of the chest. The pain is exacerbated by breathing and coughing. Objectively: the skin is pale, the lips are cyanotic, the respiratory rate is up to 30 per minute, the right half of the chest is enlarged in volume, the intercostal spaces are smoothed. -

Clinical Usefulness of 'Vocal Fremitus' and 'Vocal Resonance'
RESEARCH Clinical usefulness of ‘vocal fremitus’ and ‘vocal resonance’ Kyaw San Hla MMedSc, MRCP, FRACP, is Senior Lecturer and staff physician, James Cook University, Mackay Base GP perceptions and practice Hospital, Queensland. kyaw. [email protected] Assessment of vocal fremitus (VF) and vocal resonance The study was approved by the Ethics Committee at Mackay (VR) (whereby vocal vibrations are felt or heard during Base Hospital. a clinical examination) is an established part of physical examination of the respiratory system. Textbooks on Results clinical examination include these procedures as part of Sixty-seven responses were obtained (64 GPs and three the standard method.1–3 general practice registrars), providing a response rate of approximately 70%. Forty-four respondents (65.7%) Undergraduate and postgraduate candidates are required rarely performed VF/VR as part of routine chest examination to perform VF and VR when they undertake qualifying (Figure 1). 50 44 assessments, however the reliability of findings from More than half (53.7%) 40 these procedures is controversial.4 It is also unusual to disagreed with the statement 30 see experienced doctors performing VF/VR during actual that ‘routine inclusion of either chest examination. The author of the only identifiable study VF or VR on chest examination Count 20 9 on clinicians’ attitudes toward VF/VR (which had only 14 is desirable’ (with 11.9% strongly 10 6 2 3 3 respondents) remarked ‘it will be rare to see physicians disagreeing). More than a quarter 0 near about about about about rarely doing both or even one of them although the majority has (28%) remained neutral. -

Silent Reflux (Also Called LPR Or EOR)
Silent reflux (also called LPR or EOR) This leaflet explains what your condition is, why it happens, what the symptoms are and how it can be managed. If there is anything you don’t understand or if you have any further questions please talk to your doctor or nurse. What is silent reflux? Everyone has juices in the stomach which are acidic and digest and break down food. At the top of the stomach there is a muscular valve which closes to prevent food and stomach juices escaping upwards into the gullet. If this muscular valve (oesophageal sphincter) does not work very well, the stomach juices can leak backwards into the gullet, causing reflux or symptoms of indigestion (heartburn). However, in some people, small amounts of stomach juice can spill even further back into the back of your throat, affecting the throat lining and your voice box (larynx) and causing irritation and hoarseness. This is known as laryngo pharyngeal reflux (LPR) or extra oesophageal reflux (EOR). Its common name is 'silent reflux' because many people do not experience any of the classic symptoms of heartburn or indigestion. Silent reflux can occur during the day or night, even if a person hasn't eaten anything. Usually, however, silent reflux occurs at night. What are the symptoms of silent reflux? The most common symptoms are: • A sensation of food sticking or a feeling of a lump in the throat. • A hoarse, tight or 'croaky' voice. • Frequent throat clearing. • Difficulty swallowing (especially tablets or solid foods). • A sore, dry and sensitive throat. • Occasional unpleasant "acid" or "bilious" taste at the back of the mouth. -
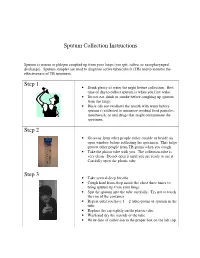
Sputum Collection Instructions Step 1 Step 2 Step 3
Sputum Collection Instructions Sputum is mucus or phlegm coughed up from your lungs (not spit, saliva, or nasopharyngeal discharge). Sputum samples are used to diagnose active tuberculosis (TB) and to monitor the effectiveness of TB treatment. Step 1 • Drink plenty of water the night before collection. Best time of day to collect sputum is when you first wake. • Do not eat, drink or smoke before coughing up sputum from the lungs. • Rinse (do not swallow) the mouth with water before sputum is collected to minimize residual food particles, mouthwash, or oral drugs that might contaminate the specimen. Step 2 • Go away from other people either outside or beside an open window before collecting the specimen. This helps protect other people from TB germs when you cough. • Take the plastic tube with you. The collection tube is very clean. Do not open it until you are ready to use it. Carefully open the plastic tube. Step 3 • Take several deep breaths. • Cough hard from deep inside the chest three times to bring sputum up from your lungs. • Spit the sputum into the tube carefully. Try not to touch the rim of the container. • Repeat until you have 1 – 2 tablespoons of sputum in the tube. • Replace the cap tightly on the plastic tube. • Wash and dry the outside of the tube. • Write date of collection in the proper box on the lab slip. Step 4 • Place the primary specimen container (usually a conical centrifuge tube) in the clear plastic baggie that has the biohazard symbol imprint. • Place the white absorbent sheet in the plastic baggie. -

Perinatal/Neonatal Case Presentation
Perinatal/Neonatal Case Presentation &&&&&&&&&&&&&& Urinary Tract Infection With Trichomonas vaginalis in a Premature Newborn Infant and the Development of Chronic Lung Disease David J. Hoffman, MD vaginal bleeding with suspected abruption resulted in delivery of Gerard D. Brown, DO the infant by Cesarean section. The Apgar scores were 1, 5, and 9 Frederick H. Wirth, MD at 1, 5, and 10 minutes of life, respectively. Betsy S. Gebert, CRNP After delivery, the infant was managed with mechanical Cathy L. Bailey, MS, CRNP ventilation with pressure support and volume guarantee for Endla K. Anday, MD respiratory distress syndrome. She received exogenous surfactant We report a case of a low-birth-weight infant with an infection of the urinary tract with Trichomonas vaginalis, who later developed cystic chronic lung disease suggestive of Wilson-Mikity syndrome. Although she had mild respiratory distress syndrome at birth, the extent of the chronic lung disease was out of proportion to the initial illness. We speculate that maternal infection with this organism may have resulted in an inflammatory response that led to its development. Journal of Perinatology (2003) 23, 59 – 61 doi:10.1038/sj.jp.7210819 CASE PRESENTATION A 956-g, appropriate-for-gestational-age, African–American female was delivered by Cesarean section following 27 5/7 weeks of gestation in breech presentation after a period of advanced cervical dilatation and uterine contractions. Her mother was a 20-year-old gravida 5, para 2022 woman whose prenatal laboratory data were significant for vaginal colonization with Streptococcus agalactiae, treatment for Chlamydia trachomatis, and a history of cocaine and marijuana usage confirmed by urine toxicology. -

Chest Pain in Pediatrics
PEDIATRIC CARDIOLOGY 0031-3955/99 $8.00 + .OO CHEST PAIN IN PEDIATRICS Keith C. Kocis, MD, MS Chest pain is an alarming complaint in children, leading an often frightened and concerned family to a pediatrician or emergency room and commonly to a subsequent referral to a pediatric cardiologist. Because of the well-known associ- ation of chest pain with significant cardiovascular disease and sudden death in adult patients, medical personnel commonly share heightened concerns over pediatric patients presenting with chest pain. Although the differential diagnosis of chest pain is exhaustive, chest pain in children is least likely to be cardiac in origin. Organ systems responsible for causing chest pain in children include*: Idiopathic (12%-85%) Musculoskeletal (15%-31%) Pulmonary (12%-21%) Other (4%-21%) Psychiatric (5%-17%) Gastrointestinal (4'/0-7%) Cardiac (4%4%) Furthermore, chest pain in the pediatric population is rareZy associated with life-threatening disease; however, when present, prompt recognition, diagnostic evaluation, and intervention are necessary to prevent an adverse outcome. This article presents a comprehensive list of differential diagnostic possibilities of chest pain in pediatric patients, discusses the common causes in further detail, and outlines a rational diagnostic evaluation and treatment plan. Chest pain, a common complaint of pediatric patients, is often idiopathic in etiology and commonly chronic in nature. In one study,67 chest pain accounted for 6 in 1000 visits to an urban pediatric emergency room. In addition, chest pain is the second most common reason for referral to pediatric cardiologist^.^, 23, 78 Chest pain is found equally in male and female patients, with an average *References 13, 17, 23, 27, 32, 35, 44, 48, 49, 63-67, 74, and 78. -

Gas Exchange and Respiratory Function
LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 484 Aptara Gas Exchange and 5 Respiratory Function Applying Concepts From NANDA, NIC, • Case Study and NOC A Patient With Impaired Cough Reflex Mrs. Lewis, age 77 years, is admitted to the hospital for left lower lobe pneumonia. Her vital signs are: Temp 100.6°F; HR 90 and regular; B/P: 142/74; Resp. 28. She has a weak cough, diminished breath sounds over the lower left lung field, and coarse rhonchi over the midtracheal area. She can expectorate some sputum, which is thick and grayish green. She has a history of stroke. Secondary to the stroke she has impaired gag and cough reflexes and mild weakness of her left side. She is allowed food and fluids because she can swallow safely if she uses the chin-tuck maneuver. Visit thePoint to view a concept map that illustrates the relationships that exist between the nursing diagnoses, interventions, and outcomes for the patient’s clinical problems. LWBK330-4183G-c21_p484-516.qxd 23/07/2009 02:09 PM Page 485 Aptara Nursing Classifications and Languages NANDA NIC NOC NURSING DIAGNOSES NURSING INTERVENTIONS NURSING OUTCOMES INEFFECTIVE AIRWAY CLEARANCE— RESPIRATORY MONITORING— Return to functional baseline sta- Inability to clear secretions or ob- Collection and analysis of patient tus, stabilization of, or structions from the respiratory data to ensure airway patency improvement in: tract to maintain a clear airway and adequate gas exchange RESPIRATORY STATUS: AIRWAY PATENCY—Extent to which the tracheobronchial passages remain open IMPAIRED GAS