Niger: Assessment of Malaria Control
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Progress Report on Soil Fertility Restoration
PROGRESS REPORT ON SOIL FERTILITY RESTORATION PROJECT (WEST AFRICA) THE U.S. AGENCY FOR INTERNATIONAL DEVELOPMENT BY INTERNATIONAL FERTILIZER DEVELOPMENT CENTER November, 1988 2 TABLE OF CONTENTS Pagie 1.0 Introduction 3 2.0 Start-up Phase and Staffing 7 2.1 Administration and Personnel Recruitment 7 2.2 Links with Organizations Promoting Fertilizer Use 8 2.3 National Collaborating Institutions and Zones of Operation 9 2.4 Preparation and Adoption of Supplementary Technical Paper 10 3.0 Development of Work Plan 11 4.0 Prel-minz.ry/Exploratory Survey 11 4.1 Ghana 12 4.2 Niger 13 4.3 Togo 15 5.0 Verification Survey and The Role of Women in the SFRP 15 6.0 On Farm Trials 16 6.1 Training of Collaborators in Ghana 16 6.2 Design and Establishment of OFT in Ghana 17 6.3 Design and Fstablishment of OFT in Niger 18 7.0 Environmental impact of Fertilizer Use 18 8.0 Operating Problems During Phase One 19 9.0 Project Monitoring/Management to Overcome Problems 19 10.0 Plans for 1988/89 20 11.0 Appendices 22 SFRP ;RC";ESS REPCRT 3 PROGRESS REPORT SOIL FERTILITY RESTORATIOV PROJECT (WEST AFRICA) 1.0 Introduction Rapidly increasing populations coupled with declining per capita food production continue to place sub-Saharan Africa at the center of international concern in relauion to food availability and production. The regions of best and Central Africa present some of the most complex problems in agricultural development during the latter quarter of this century. The soils of West Africa are generally low in fertility, very fragile, readily exhausted through Lropping, and prone to leaching of nutrients and erosion. -

F:\Niger En Chiffres 2014 Draft
Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 1 Novembre 2014 Le Niger en Chiffres 2014 Direction Générale de l’Institut National de la Statistique 182, Rue de la Sirba, BP 13416, Niamey – Niger, Tél. : +227 20 72 35 60 Fax : +227 20 72 21 74, NIF : 9617/R, http://www.ins.ne, e-mail : [email protected] 2 Le Niger en Chiffres 2014 Le Niger en Chiffres 2014 Pays : Niger Capitale : Niamey Date de proclamation - de la République 18 décembre 1958 - de l’Indépendance 3 août 1960 Population* (en 2013) : 17.807.117 d’habitants Superficie : 1 267 000 km² Monnaie : Francs CFA (1 euro = 655,957 FCFA) Religion : 99% Musulmans, 1% Autres * Estimations à partir des données définitives du RGP/H 2012 3 Le Niger en Chiffres 2014 4 Le Niger en Chiffres 2014 Ce document est l’une des publications annuelles de l’Institut National de la Statistique. Il a été préparé par : - Sani ALI, Chef de Service de la Coordination Statistique. Ont également participé à l’élaboration de cette publication, les structures et personnes suivantes de l’INS : les structures : - Direction des Statistiques et des Etudes Economiques (DSEE) ; - Direction des Statistiques et des Etudes Démographiques et Sociales (DSEDS). les personnes : - Idrissa ALICHINA KOURGUENI, Directeur Général de l’Institut National de la Statistique ; - Ibrahim SOUMAILA, Secrétaire Général P.I de l’Institut National de la Statistique. Ce document a été examiné et validé par les membres du Comité de Lecture de l’INS. Il s’agit de : - Adamou BOUZOU, Président du comité de lecture de l’Institut National de la Statistique ; - Djibo SAIDOU, membre du comité - Mahamadou CHEKARAOU, membre du comité - Tassiou ALMADJIR, membre du comité - Halissa HASSAN DAN AZOUMI, membre du comité - Issiak Balarabé MAHAMAN, membre du comité - Ibrahim ISSOUFOU ALI KIAFFI, membre du comité - Abdou MAINA, membre du comité. -
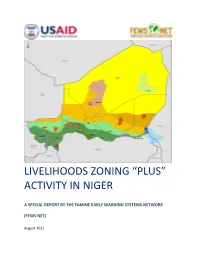
Livelihoods Zoning “Plus” Activity in Niger
LIVELIHOODS ZONING “PLUS” ACTIVITY IN NIGER A SPECIAL REPORT BY THE FAMINE EARLY WARNING SYSTEMS NETWORK (FEWS NET) August 2011 Table of Contents Introduction .................................................................................................................................................. 3 Methodology ................................................................................................................................................. 4 National Livelihoods Zones Map ................................................................................................................... 6 Livelihoods Highlights ................................................................................................................................... 7 National Seasonal Calendar .......................................................................................................................... 9 Rural Livelihood Zones Descriptions ........................................................................................................... 11 Zone 1: Northeast Oases: Dates, Salt and Trade ................................................................................... 11 Zone 2: Aïr Massif Irrigated Gardening ................................................................................................ 14 Zone 3 : Transhumant and Nomad Pastoralism .................................................................................... 17 Zone 4: Agropastoral Belt ..................................................................................................................... -

BROCHURE Dainformation SUR LA Décentralisation AU NIGER
REPUBLIQUE DU NIGER MINISTERE DE L’INTERIEUR, DE LA SECURITE PUBLIQUE, DE LA DECENTRALISATION ET DES AFFAIRES COUTUMIERES ET RELIGIEUSES DIRECTION GENERALE DE LA DECENTRALISATION ET DES COLLECTIVITES TERRITORIALES brochure d’INFORMATION SUR LA DÉCENTRALISATION AU NIGER Edition 2015 Imprimerie ALBARKA - Niamey-NIGER Tél. +227 20 72 33 17/38 - 105 - REPUBLIQUE DU NIGER MINISTERE DE L’INTERIEUR, DE LA SECURITE PUBLIQUE, DE LA DECENTRALISATION ET DES AFFAIRES COUTUMIERES ET RELIGIEUSES DIRECTION GENERALE DE LA DECENTRALISATION ET DES COLLECTIVITES TERRITORIALES brochure d’INFORMATION SUR LA DÉCENTRALISATION AU NIGER Edition 2015 - 1 - - 2 - SOMMAIRE Liste des sigles .......................................................................................................... 4 Avant propos ............................................................................................................. 5 Première partie : Généralités sur la Décentralisation au Niger ......................................................... 7 Deuxième partie : Des élections municipales et régionales ............................................................. 21 Troisième partie : A la découverte de la Commune ......................................................................... 25 Quatrième partie : A la découverte de la Région .............................................................................. 53 Cinquième partie : Ressources et autonomie de gestion des collectivités ........................................ 65 Sixième partie : Stratégies et outils -

CFAES ESO 1313.Pdf (3.597Mb)
Economics and Sociology Occasional Paper #1313 FINANCIAL MARKETS IN RURAL NIGER THE BOUNDARIES OF INSTITUTIONS Carlos E. Cuevas October, 1986 Department of Agricultural Economics and Rural Sociology The Ohio State University 2120 Fyffe Road Columbus, Ohio 43210 Paper prepared for presentation at the Annual Meeting of the African Studies Association, Madison, Wisconsin, October SO November 2, 1986. FINANCIAL MARKETS IN RURAL NIGER THE BOUNDARIES OF INSTITUTIONS 1. Introduction The institutional financial system of Niger is very underdeveloped. There are only 27 bank branches in the country, which represents approximately one bank branch for every 226 thousand inhabitants, undoubtedly one of the lowest ratios in the world. One of the poorest countries in Asia, Bangladesh has a ratio of one branch for about 25 thousand people, while one of the poorest countries in Latin America, Honduras, has one bank branch for every 15 thousand inhabitants. Even though about 90 percent of the Nigerien population lives in the rural sector, one-third of the bank branches are located in the capital city. Therefore the provision of financial services by formal institutions is even more limited in the rural areas than it is in the urban centers. This paper documents and analyzes the functioning of financial markets in the rural areas of Niger. The study discusses the prevalence and importance of formal and informal financial transactions at the household level. Emphasis is given to the analysis of institutional limitations in the provision of financial services to rural households. The discussion draws upon data obtained in an extensive field survey of rural households undertaken in 1985. -
A Simple National Atlas of Niger
A Simple National Atlas of Niger Copyright Calvin College, 2011 This map atlas has been produced by Calvin College, Department of Geology, Geography, and Environmental Studies students. It is provided free of any charge as a service to global communities and can be distributed freely. Changes, alterations, and use are allowed with the agreement that Calvin College, Department of Geology, Geography, and Environmental Studies is recognized as the original author. No warranty is given for this map as to accuracy and is based on available data. Created in Fall 2010. Inquiries can be made to Dr. Jason VanHorn at Calvin College. http://www.calvin.edu/academic/geology/faculty/ A Simple Atlas Niger Elevation of Niger Niger features desert L I B Y A plains through out the Elevation (m) country with a hilly -182 - 196 northern area. 197 - 371 It is one of the hottest 372 - 536 and driest countries in 537 - 736 the world and its A L G E R I A 737 - 962 southern section contains sparse 963 - 1,180 savanna areas. 1,181 - 1,423 Agadez 1,424 - 1,774 The highest peak is Idoukal-n-Taghes at 1,775 - 2,338 2,022 meters. 2,339 - 5,780 M A L I Tahoua Diffa Tillaberi Zinder Maradi Niamey C H A D Dosso This map has been produced by Calvin College, Department of Geology, Geography, BURKINA and Environmental Studies. It is provided N I G E R I A free of any charge as a service to global FASO communities and can be distributed freely. -

Cross-Border Cooperation Between Niger and Nigeria: Opportunities and Challenges for the Maradi Micro-Region in West Africa
Cross-Border Cooperation between Niger and Nigeria: Opportunities and Challenges for the Maradi Micro-Region in West Africa Terhemba Nom AMBE-UVA Department of French and International Studies, National Open University of Nigeria 14-16 Ahmadu Bello Way, Victoria Island, Lagos, NIGERIA. [email protected] +2348068799158 A Paper for Presentation at the Conference on “Cross-Border Trade in Africa: The Local Politics of a Global Economy” within the Framework of the Fourth ABORNE (African Borderlands Research Network) in Basel, Switzerland from September 08 through September 11, 2010. 1 Abstract Within Africa, renewed interest is being shown in sub-regional integration and West Africa is no exception. Micro-regions act as a microcosm and an entry point to the study of regionalism in Africa. This paper presents the case of a “micro-region” developing within the broader Benin-Niger-Nigeria border-zone. The study illustrates that cross-border cooperation is the driver and engine of regional integration, a kind of regional cooperation transcending the micro-region itself with a variety of integrative trends. The distinctive characteristic of the Maradi-Katsina-Kano micro-region is the promotion of regional trade beyond the borders of Niger and Nigeria. It contends that formal borders either essentially does not exist in the Westphalian sense, being ignored by actors such as local populations and traders, or strategically used by representatives of the state to extract resources and rents. The dynamism of this “micro-initiative” tends to cement peaceful relationships, develop social and economic interdependencies, and make up a base for “regional civil society”. Even though there is an increasing awareness by politicians and institutional leaders that micro-regional processes should be encouraged and included in the regional integration process, there is still a long way to go before the top-down and state-led macro- regional policies are synchronised with such micro-regional dynamics. -

Legislative Reform, Tenure, and Natural Resource Management in Niger: the New Rural Code
IfllQRKSHOFMN POLIT1CIAL THEORY AND POLJCY ANALYSIS 513 NORTH PARK JNDWNA UNIVERSITY INDJAWA 474f ''3186 LEGISLATIVE REFORM, TENURE, AND NATURAL RESOURCE MANAGEMENT IN NIGER: THE NEW RURAL CODE by Kent M. Elbow Paper prepared for the Comite Permanent Inter-Etats de Lutte contre la Secheresse dans le Sahel Support for the paper has been provided by the United States Agency for International Development i All views, interpretations, recommendations, and conclusions expressed in this paper are those of the author and not necessarily those of the supporting or cooperating institutions. Land Tenure Center University of Wisconsin-Madison May, 1996 CONTENTS BRIEF SUMMARY OF FINDINGS I. INTRODUCTION Background and Structure A Note on the Limited Scope and Specific Nature of the Study A Note on the Information Sources Contributing to this Case Study of Legislative Reform in Niger H. SETTING THE STAGE FOR THE RURAL CODE INITIATIVE A History of Centralization and Introduction of Competing Tenure Systems The Road to Praia and Decentralization The Continuing Dominance of Customary Systems of Tenure and Resource Management in the Sahel Genesis of the Rural Code Project HI. THE POLICYMAKING AND ADMINISTRATIVE ENVIRONMENT IN NIGER, AND THE APPROACH AND METHODOLOGY OF THE RURAL CODE PROCESS The Rural Code within the Broader Context of Rural Development, Tenure and Natural Resource Management and Administration in Niger The Unfolding Methodology of the Rural Code Summary of Rural Code Methodology and its Degree of Success in Achieving Objectives IV. POLICY CHOICES DEFINED BY THE RURAL CODE PROCESS Promoting Security of Access Rights to Resources Conservation and Natural Resource Management State Institutions, Regional Planning, Private Organizations of Rural Populations, Credit and Conflict Management ^ Summary of Rural Code Policy Choices V. -

Case of the Early Alert System of Niger
Tropentag 2011 University of Bonn, October 5 - 7, 2011 Conference on International Research on Food Security, Natural Resource Management and Rural Development The assessment of food vulnerability in Sahel countries: case of the early alert system of Niger Ludovic Andresa1, Philippe Lebaillyb a Phd Student in ULg-Gembloux Agro-Bio Tech, Economic and rural development unit, 5030 Gembloux, Belgium b Professor in ULg-Gembloux Agro-Bio Tech, Economic and rural development unit, 5030 Gembloux, Belgium. Introduction The definition of food vulnerability is multidisciplinary and is linked to food security. Many agencies use food vulnerability to select target population of different rural projects. Niger is one on the poorest countries on the World. In Niger, the early alert system and the national statistical institute define the food vulnerability as « the analysis of adaptation mechanisms and reaction IDFHG ZLWK D GLIILFXOW VLWXDWLRQ ,I WKH PHFKDQLVPV DUHQ¶W HIIHFWLYH WKH KRXVHKROG LV LQ D temporary or structural vulnerability situation » (SAP and INS, 2010). In the country, we can observe two types of food insecurity: the structural and the cyclical insecurity. The structural insecurity depends on poverty and climatic hazards. The cyclical insecurity affects a layer of the population each year especially the rural household (CC/SAP, 2008). The early alert system of Niger has existed since 1989. This system analyses the food vulnerability every year and every month in each department. The early alert system characterizes the annual vulnerability for each department and this analysis is made for determine the most vulnerable departments who will receive a monthly monitoring (CC/SAP, 2004). This annual analysis identifies the area and the population most at risk. -

C:\Mes Documents\Annuaires\Annu
ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 REPUBLIQUE DU NIGER MINISTERE DU PLAN -©©©- INSTITUT NATIONAL DE LA STATISTIQUE Etablissement Public à Caractère Administratif ANNUAIRE STATISTIQUE 2013-2017 Edition 2018 Novembre 2018 1 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 2 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 ANNUAIRE STATISTIQUE 2013 - 2017 EDITION 2018 Novembre 2018 3 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 4 Institut National de la Statistique ANNUAIRE STATISTIQUE DU NIGER 2013 - 2017 Ce document a été élaboré par : - Sani ALI, Chef de Division de la Coordination Statistique et de la Coopération Ont également participé à l’élaboration de cette publication, les structures et personnes suivantes de l’Institut National de la Statistique (INS) : Les structures : - Direction de la Comptabilité Nationale, de la Conjoncture et des Etudes Economiques (DCNCEE) ; - Direction des Statistiques et des Etudes Démographiques et Sociales (DSEDS). Les personnes : - Idrissa ALICHINA KOURGUENI, Directeur Général de l’Institut National de la Statistique ; - Issoufou SAIDOU, Directeur de la Coordination et du Management de l’Information Statistique. Ce document a été examiné et validé par les personnes ci-après : - Maman Laouali ADO, Conseiller du DG/INS ; - Djibo SAIDOU, Inspecteur des Services Statistiques (ISS) ; - Ghalio EKADE, Inspecteur de Services Statistiques (ISS) ; - Sani ALI, Chef de Division de la Coordination Statistique et de -

Violent Extremism, Organised Crime and Local Conflicts in Liptako-Gourma William Assanvo, Baba Dakono, Lori-Anne Théroux-Bénoni and Ibrahim Maïga
Violent extremism, organised crime and local conflicts in Liptako-Gourma William Assanvo, Baba Dakono, Lori-Anne Théroux-Bénoni and Ibrahim Maïga This report analyses the links between violent extremism, illicit activities and local conflicts in the Liptako-Gourma region. Addressing regional instability in the long term requires empirical data that helps explain the local dynamics that fuel insecurity. This is the first of two reports, and is based on interviews conducted in Burkina Faso, Mali and Niger. The second report assesses the measures aimed at bringing stability to the region. WEST AFRICA REPORT 26 | DECEMBER 2019 Key findings There are several armed groups operating in Support for illicit activities such as poaching the Liptako-Gourma region: violent extremist in eastern Burkina Faso or attitudes towards groups, Malian armed groups that are local conflicts such as the Fulani-Daoussahaq signatories to the peace agreement, and self- conflict on the Mali-Niger border have enabled defence groups. They are all directly or indirectly violent extremists to establish themselves and involved in illicit activities and local conflicts. recruit in some communities. Violent extremist groups are generally The argument that violent extremist groups pragmatic and opportunistic in how they exploit and exacerbate local tensions and position themselves regarding illicit activities conflicts is simplistic. The positioning of these and local conflicts. They are resilient and groups in relation to local conflicts varies adaptable. They exploit the nature and depending on the context and their strategic vulnerabilities of local economies, rivalries objectives. Violent extremists can either be between different socio-professional groups party to conflicts or serve as mediators, and and governance deficiencies. -

Downloaded from Afsis Website
REPUBLIC OF NIGER FRATERNITY – LABOR - PROGRESS MINISTRY OF FINANCE NATIONAL INSTITUTE OF STATISTICS 2011 National Survey on Household Living Conditions and Agriculture (ECVM/A-2011) BASIC INFORMATION DOCUMENT October 2013 ACRONYMS ECVM/A National Survey on Living Conditions and Agriculture 2011 ENBC National Survey on Household Budget and Consumption GDP Gross Domestic Product INS National Institute of Statistics LSMS-ISA Living Standards Measurement Study – Integrated Surveys on Agriculture MDG Millennium Development Goal QUIBB Core Welfare Indicator Questionnaire ZD Enumeration area CONTENTS 1. INTRODUCTION .................................................................................................................. 1 2. CHARACTERISTICS OF THE SURVEY ............................................................................ 2 2.1. Brief Introduction to the Survey and the Household Questionnaire – first visit ............. 2 2.2. DESCRIPTION OF THE SECOND VISIT QUESTIONNAIRE ................................... 3 2.3 Description of the agriculture and livestock questionnaire – First Visit .......................... 3 2.4 description of the agriculture and livestock questionnaire – second visit ........................ 3 2.5 description of the community questionnaire .................................................................... 3 3. SAMPLING ........................................................................................................................... 3 4 PILOT TEST .........................................................................................................................