Applying Systems Science Methods to Risk-Based Disease Management and Population Oral Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Violence and Masculinity in Hollywood War Films During World War II a Thesis Submitted To
Violence and Masculinity in Hollywood War Films During World War II A thesis submitted to: Lakehead University Faculty of Arts and Sciences Department of History In partial fulfillment of the requirements for the degree in Master of Arts Matthew Sitter Thunder Bay, Ontario July 2012 Library and Archives Bibliothèque et Canada Archives Canada Published Heritage Direction du Branch Patrimoine de l'édition 395 Wellington Street 395, rue Wellington Ottawa ON K1A 0N4 Ottawa ON K1A 0N4 Canada Canada Your file Votre référence ISBN: 978-0-494-84504-2 Our file Notre référence ISBN: 978-0-494-84504-2 NOTICE: AVIS: The author has granted a non- L'auteur a accordé une licence non exclusive exclusive license allowing Library and permettant à la Bibliothèque et Archives Archives Canada to reproduce, Canada de reproduire, publier, archiver, publish, archive, preserve, conserve, sauvegarder, conserver, transmettre au public communicate to the public by par télécommunication ou par l'Internet, prêter, telecommunication or on the Internet, distribuer et vendre des thèses partout dans le loan, distrbute and sell theses monde, à des fins commerciales ou autres, sur worldwide, for commercial or non- support microforme, papier, électronique et/ou commercial purposes, in microform, autres formats. paper, electronic and/or any other formats. The author retains copyright L'auteur conserve la propriété du droit d'auteur ownership and moral rights in this et des droits moraux qui protege cette thèse. Ni thesis. Neither the thesis nor la thèse ni des extraits substantiels de celle-ci substantial extracts from it may be ne doivent être imprimés ou autrement printed or otherwise reproduced reproduits sans son autorisation. -

Lbc July07.Pdf
It’s a busy year for birthdays: John Wayne, FROM THE Laurence Olivier, Barbara Stanwyck, Fay Wray, Burgess Meredith, Katharine Hepburn, Gene BOOTH Autry, and Rosalind Russell, among others, would have turned 100 this year. We’re celebrating by NOT slavishly following the mob of classic-movie stations that will be running King Kong and His Girl Friday and Git Along Little Dogies in ’round-the- from the booth clock birthday bashes. Instead, we’re doing what we do best: dig through the vaults for unheralded gems and seldom-screened classics. So instead of Fay Wray screaming and John Wayne shooting, we have Walter Huston saving America (again!) in Gabriel Over the White House, Henry Fonda winning World War II in The Immortal Sergeant, Judy Garland and Mickey Rooney putting on a show (again!) in Strike Up the Band, and Judy Holliday foreseeing American Idol’s cult of instant celebrity in It Should Happen to You. And, for a change of pace, we’ve got giant grasshoppers, giant scorpions, giant creatures from Venus, and one tiny, tiny man in a handful of 1950s sci-fi classics scattered throughout the season. (Speaking of anniversaries, if you blinked, you probably missed the 35th anniversary of this very theater back in May. Happy birthday to us.) Program by Michael King (MK) and Michael W. Phillips, Jr. (MP) CHRISTMAS IN JULY | 1940 july 7, 2007 Director: Preston Sturges Striking while the iron was hot, America’s foremost cinematic satirist rushed his second feature as director intro production before his debut had even opened. Preston Sturges was eager to make use of a story he had been kicking around Universal for a decade: a regular go-getter (Dick Powell) is duped into thinking he’s won $25,000 in an advertising slogan contest with his asinine entry. -
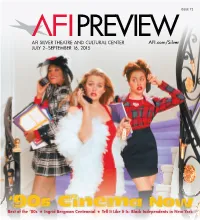
AFI PREVIEW Is Published by the Age 46
ISSUE 72 AFI SILVER THEATRE AND CULTURAL CENTER AFI.com/Silver JULY 2–SEPTEMBER 16, 2015 ‘90s Cinema Now Best of the ‘80s Ingrid Bergman Centennial Tell It Like It Is: Black Independents in New York Tell It Like It Is: Contents Black Independents in New York, 1968–1986 Tell It Like It Is: Black Independents in New York, 1968–1986 ........................2 July 4–September 5 Keepin’ It Real: ‘90s Cinema Now ............4 In early 1968, William Greaves began shooting in Central Park, and the resulting film, SYMBIOPSYCHOTAXIPLASM: TAKE ONE, came to be considered one of the major works of American independent cinema. Later that year, following Ingrid Bergman Centennial .......................9 a staff strike, WNET’s newly created program BLACK JOURNAL (with Greaves as executive producer) was established “under black editorial control,” becoming the first nationally syndicated newsmagazine of its kind, and home base for a Best of Totally Awesome: new generation of filmmakers redefining documentary. 1968 also marked the production of the first Hollywood studio film Great Films of the 1980s .....................13 directed by an African American, Gordon Park’s THE LEARNING TREE. Shortly thereafter, actor/playwright/screenwriter/ novelist Bill Gunn directed the studio-backed STOP, which remains unreleased by Warner Bros. to this day. Gunn, rejected Bugs Bunny 75th Anniversary ...............14 by the industry that had courted him, then directed the independent classic GANJA AND HESS, ushering in a new type of horror film — which Ishmael Reed called “what might be the country’s most intellectual and sophisticated horror films.” Calendar ............................................15 This survey is comprised of key films produced between 1968 and 1986, when Spike Lee’s first feature, the independently Special Engagements ............12-14, 16 produced SHE’S GOTTA HAVE IT, was released theatrically — and followed by a new era of studio filmmaking by black directors. -

The Culture of Queers
THE CULTURE OF QUEERS For around a hundred years up to the Stonewall riots, the word for gay men was ‘queers’. From screaming queens to sensitive vampires and sad young men, and from pulp novels and pornography to the films of Fassbinder, The Culture of Queers explores the history of queer arts and media. Richard Dyer traces the contours of queer culture, examining the differ- ences and continuities with the gay culture which succeeded it. Opening with a discussion of the very concept of ‘queers’, he asks what it means to speak of a sexual grouping having a culture and addresses issues such as gay attitudes to women and the notion of camp. Dyer explores a range of queer culture, from key topics such as fashion and vampires to genres like film noir and the heritage film, and stars such as Charles Hawtrey (outrageous star of the Carry On films) and Rock Hudson. Offering a grounded historical approach to the cultural implications of queerness, The Culture of Queers both insists on the negative cultural con- sequences of the oppression of homosexual men and offers a celebration of queer resistance. Richard Dyer is Professor of Film Studies at The University of Warwick. He is the author of Stars (1979), Now You See It: Studies in Lesbian and Gay Film (Routledge 1990), The Matter of Images (Routledge 1993) and White (Routledge 1997). THE CULTURE OF QUEERS Richard Dyer London and New York First published 2002 by Routledge 11 New Fetter Lane, London EC4P 4EE Simultaneously published in the USA and Canada by Routledge 29 West 35th Street, New York, NY 10001 Routledge is an imprint of the Taylor & Francis Group This edition published in the Taylor and Francis e-Library, 2005. -

Autograph Albums - ITEM 936
Autograph Albums - ITEM 936 A Jess Barker Jocelyn Brando Lex Barker Marlon Brando Walter Abel Binnie Barnes Keefe Brasselle Ronald Adam Lita Baron Rossano Brazzi Julie Adams Gene Barry Teresa Brewer (2) Nick Adams John Barrymore, Jr. (2) Lloyd Bridges Dawn Addams James Barton Don Briggs Brian Aherne Count Basie Barbara Britton Eddie Albert Tony Bavaar Geraldine Brooks Frank Albertson Ann Baxter Joe E. Brown Lola Albright John Beal Johnny Mack Brown Ben Alexander Ed Begley, Sr. Les Brown John Alexander Barbara Bel Geddes Vanessa Brown Richard Allan Harry Belafonte Carol Bruce Louise Allbritton Ralph Bellamy Yul Brynner Bob “Tex” Allen Constance Bennett Billie Burke June Allyson Joan Bennett George Burns and Gracie Allen Kirk Alyn Gertrude Berg Richard Burton Don Ameche Polly Bergen Spring Byington Laurie Anders Jacques Bergerac Judith Anderson Yogi Berra C Mary Anderson Edna Best Susan Cabot Warner Anderson (2) Valerie Bettis Sid Caesar Keith Andes Vivian Blaine James Cagney Dana Andrews Betsy Blair Rory Calhoun (2) Glenn Andrews Janet Blair Corinne Calvet Pier Angeli Joan Blondell William Campbell Eve Arden Claire Bloom Judy Canova Desi Arnaz Ben Blue Macdonald Carey Edward Arnold Ann Blyth Kitty Carlisle Mary Astor Humphrey Bogart Richard Carlson Jean-Pierre Aumont Ray Bolger Hoagy Carmichael Lew Ayres Ward Bond Leslie Caron B Beulah Bondi John Carradine Richard Boone Madeleine Carroll Lauren Bacall Shirley Booth Nancy Carroll Buddy Baer Ernest Borgnine Jack Carson (2) Fay Bainter Lucia Bose Jeannie Carson Suzan Ball Long Lee Bowman -

Film Noir Database
www.kingofthepeds.com © P.S. Marshall (2021) Film Noir Database This database has been created by author, P.S. Marshall, who has watched every single one of the movies below. The latest update of the database will be available on my website: www.kingofthepeds.com The following abbreviations are added after the titles and year of some movies: AFN – Alternative/Associated to/Noirish Film Noir BFN – British Film Noir COL – Film Noir in colour FFN – French Film Noir NN – Neo Noir PFN – Polish Film Noir www.kingofthepeds.com © P.S. Marshall (2021) TITLE DIRECTOR Actor 1 Actor 2 Actor 3 Actor 4 13 East Street (1952) AFN ROBERT S. BAKER Patrick Holt, Sandra Dorne Sonia Holm Robert Ayres 13 Rue Madeleine (1947) HENRY HATHAWAY James Cagney Annabella Richard Conte Frank Latimore 36 Hours (1953) BFN MONTGOMERY TULLY Dan Duryea Elsie Albiin Gudrun Ure Eric Pohlmann 5 Against the House (1955) PHIL KARLSON Guy Madison Kim Novak Brian Keith Alvy Moore 5 Steps to Danger (1957) HENRY S. KESLER Ruth Ronan Sterling Hayden Werner Kemperer Richard Gaines 711 Ocean Drive (1950) JOSEPH M. NEWMAN Edmond O'Brien Joanne Dru Otto Kruger Barry Kelley 99 River Street (1953) PHIL KARLSON John Payne Evelyn Keyes Brad Dexter Frank Faylen A Blueprint for Murder (1953) ANDREW L. STONE Joseph Cotten Jean Peters Gary Merrill Catherine McLeod A Bullet for Joey (1955) LEWIS ALLEN Edward G. Robinson George Raft Audrey Totter George Dolenz A Bullet is Waiting (1954) COL JOHN FARROW Rory Calhoun Jean Simmons Stephen McNally Brian Aherne A Cry in the Night (1956) FRANK TUTTLE Edmond O'Brien Brian Donlevy Natalie Wood Raymond Burr A Dangerous Profession (1949) TED TETZLAFF George Raft Ella Raines Pat O'Brien Bill Williams A Double Life (1947) GEORGE CUKOR Ronald Colman Edmond O'Brien Signe Hasso Shelley Winters A Kiss Before Dying (1956) COL GERD OSWALD Robert Wagner Jeffrey Hunter Virginia Leith Joanne Woodward A Lady Without Passport (1950) JOSEPH H. -

Post-War America, the Hollywood Left and the Problem with Film Noir
Re-examining the Maladjusted Text: Post-war America, the Hollywood Left and the Problem with Film Noir Robert John Manning PhD Thesis University of East Anglia School of Film, Television and Media Studies October 2015 “This copy of the thesis has been supplied on condition that anyone who consults it is understood to recognise that its copyright rests with the author and that use of any information derived there from must be in accordance with current UK Copyright Law. In addition, any quotation or extract must include full attribution.” Re-examining the Maladjusted Text: Post-war America, the Hollywood Left and the Problem with Film Noir Film noir is a term created after fact and applied back to films from a previous period and studies have often conflated very different films and privileged some facets over others in an endeavour to structure a definition. Some scholars have identified that a relatively small group of films came to be seen by the Hollywood Left as highly significant; and that their discussions of these films were the products of deeper anxieties faced by this group in the immediate post-war period. Subsequent conclusions were made that the Hollywood Left was opposed to this generalised categorisation similar to contemporary understandings of film noir. The thesis examines those films now considered as film noir in their original contexts. Studying the reception of films generally considered to be representative of contemporary understandings of film noir, such as Boomerang (Elia Kazan, 1947) The Big Sleep (Howard Hawks, 1946) and Crossfire (Edward Dmytryk, 1947) shows how they were parts of very different cycles at the time and not seen critically as a homogeneous group. -

Recent Acquisitions, 1956—1959
TEDDY AT THE THROTTLE (1916) Recent Acquisitions, 1956—1959 1909 HEKSEN OG CYKLISTEN (The Witch and the 1922 THE PRIMITIVE LOVER, produced by Joseph Bicyclist), Denmark, director unknown. An early M. Schenck for First National, directed by Sidney trick film. Acquired through the courtesy of the Franklin, scenario by Frances Marion, based on a Danske Filmmuseum, Copenhagen. 16mm, 1 reel. story by Edgar Selwyn, photography by David Abel; with Constance Talmadge, Harrison Ford, Kenneth 1916 TEDDY AT THE THROTTLE, produced by Harlan, Joe Roberts, Charles Stevens. Gift of Paul Mack Sennett for Triangle-Keystone, directed by Killiam. 35mm, 5 reels. Clarence Badger, photographed by J. C. Bitzer; with Bobbie Vernon, Gloria Swanson, Wallace Beery, 1924 WAXWORKS, produced by Viking Film, Germany, May Emory, Blanche Phillips, and Teddy, the Key- directed and designed by Paul Leni, scenario by Henrik stone dog. Acquired through the courtesy of Paul Galeen, photography by Helmar Lerski; with Wilhelm Killiam. 16mm, 2 reels. Dieterle, John Gottowt, Olga Belajeff, Emil Jannings, Conrad Veidt, Werner Krauss. Acquired through the 1919 TRUE HEART SUSIE, directed by D. W. Griffith courtesy of the British Film Institute, London, and for Artcraft, story by Marian Fremont; with Lillian Brandon Films, Inc. 16mm, 7 reels. Gish, Robert Harron, Clarine Seymour, Carol Demp- 1925 UAFFICHE, produced by A.B.C. Films, directed ster, Walter Higby, Loyola O'Connor, Kate Bruce. by Jean Epstein, with Nathalie Lissenko, Camille Purchase, 16mm, 6 reels. Bardou, Genica Missiro. Gift of the Cinematheque de 1920 L9 HOMMEDU LARGE, produced by A.B.C. Film, Belgique. 35mm, 5 reels. directed by Marcel L'Herbier, based on the novel by 1925 STRIKE, produced by Goskino, Moscow, written Balzac; with Marcelle Pradot, Roger Karl, Jacques and directed by Sergei Eisenstein, photographed by Catelain. -

Melodies De Guerra.Pdf
MELODIES DE GUERRA Anàlisi de les Bandes Sonores Originals (Soundtrack) de pel·lícules sobre la Segona Guerra Mundial Cristina Bosch Sierra Montserrat de Rocafiguera 20 de desembre de 2018 ESCORIAL VIC Melodies de guerra “La música transcendeix les fronteres de la llengua, de la política i de les nacions” Pau Casals 2 Melodies de guerra ÍNDEX Pàgina 1. Presentació . 4 2. Introducció . 9 3. El cinema . 15 3.1. El cinema de guerra . 16 4. La Música en el cinema . 19 4.1. La Banda Sonora (soundtrack) . 20 5. L’anàlisi de les bandes sonores . 25 5.1. Criteris de selecció de les pel·lícules . 25 5.2. Característiques cinematogràfiques . 28 5.3. Característiques musicals . 33 5.4. Comparació . 39 6. El meu soundtrack. 54 6.1. Argument novel·la . 54 6.2. Partitura . 56 6.3. Anàlisi peça musical . 57 7. Conclusions . 59 8. Bibliografia . 63 9. Annexos . - 9.1. Fitxes Tècniques pel·lícules . - 9.2. Fitxes Tècniques Bandes Sonores . - 9.3. Entrevistes . - 9.4. Llistat compositors d’origen jueu . - 9.5. Llistat directors d’origen jueu. - 9.6. Partitura . - 3 Melodies de guerra 1. PRESENTACIÓ L’objectiu d’aquest treball és fer una anàlisi comparativa de les bandes sonores d’algunes pel·lícules que tracten el tema de la Segona Guerra Mundial i, a partir de les conclusions que en trec, establir si existeix un patró comú a totes elles que pugui definir-les com a un gènere particular. Les bandes sonores, o soundtrack en anglès, han acompanyat i acompanyen totes les pel·lícules. Són músiques que els donen un segell propi que fa que impactin en els espectadors, que segueixin vigents anys després d’haver-se estrenat i que, de manera inconscient a vegades, es mantinguin en la ment de la gent, que és capaç de recordar-les i cantar-les una i altra vegada. -
![1945-05-04, [P ]](https://docslib.b-cdn.net/cover/5620/1945-05-04-p-9235620.webp)
1945-05-04, [P ]
• ” v?! yj * » THE TOLEDO UNION JOURNAL Page Five tifc , I...................... ................ ——........ — ................... .. A. Hollywood’s Loveliest Qirls Starred By M-Q-M In One of Season’s Best Stage anti Screen “Keep Your Powder Dry” Is Superb Entertainment For The Entire Family Officers’ Candidate Song Star, Jan Clayton Miami Inn Is Wins New Screen Pact By Burny Zawodny Packing ’Em In “Keep Your Powder Dry,” the Seen On A Hollywood HOLLYWOOD (Special) new Metro-Goldwyn-Mayer hit Movie Set Jan Clayton has been given a They’re packing ’em in again at the Valentine Theatre, boasts new contract with Metro-Gold- this week at the New Miami Inn one of the season’s top casts in HOLLYWOOD—Dancing wyn-Mayer Studios. The young, with an all-star cast headed by aie of the year’s finest film of- on a crowded nightclub red-haired beauty contest win Roy Vincent, M. C. ecrewball .•ings. It stars no less a love floor, rFances Rafferty and ner is now in New York scoring deluxe. ► ly and talented trio than Lana Bob Stanton are to play a 'bl1 \ a success in the musical show. Others in the cast are Viki ■ Turner, Laraine Day and Susan love scene for the new “Carousel,” and the studio de Mills, songstress; Candy Leigh, Peters. M-G-M comedy with music, cided to give her the contract toe tap and acrobatic dancer Chockfu! of laughs and tears “Abbott and Costello in as a result of her outstanding and Mme. Evon, the original •—indeed, all the ingredients that Hollywood,” in which the work in “This Man’s Navy,” the Amazon. -

AUTOGRAPH AUCTION Saturday 26 November 2011 10:00
AUTOGRAPH AUCTION Saturday 26 November 2011 10:00 International Autograph Auctions (IAA) Radisson Edwardian Heathrow Hotel 140 Bath Road Heathrow UB3 5AW International Autograph Auctions (IAA) (AUTOGRAPH AUCTION) Catalogue - Downloaded from UKAuctioneers.com Lot: 1 to the verso of a 7 x 10 photograph of Burns, n.p., 17th May GULLY JOHN: (1783-1863) English Boxer, Sportsman and 1949, to Charles Fletcher. In bold, dark fountain pen ink The Politician. Rare A.L.S., Jon. Gully, two pages, 8vo, Brighton, Little Giant of Hanover, writes, in full, 'Your good letter received 11th July 1852, to B[enjamin] Oliveira. Gully states that it has today & I am sending you this photograph which was taken given him great pleasure to hear that his correspondent has while I was Worlds Heavyweight Champion. I am living in the been returned as Member for his old Boro, commenting 'pray garden spot of the World, Life is beautifull (sic) & its just as we accept of my humble congratulations and if I rendered you any make it. God bless you, Always your Friend, Tommy Burns'. service in the cause it is indeed most gratifying to my feelings.' The image shows Burns standing outdoors in a full length He concludes by adding that he will call in at the Club tomorrow boxing pose wearing his Championship belt. One very light, afternoon 'just to take the chance of seeing you'. One very light, minor surface crease, otherwise VG minor stain to the upper edge of the first page, otherwise VG Estimate: £400.00 - £600.00 Benjamin Oliveira had been elected as the new Member of Parliament for Pontefract in 1852, a position in which Gully had served from 1832-37. -

PAA 2017 PRELIMINARY PROGRAM *As of 2/27/17 WEDNESDAY, APRIL 26
PAA 2017 PRELIMINARY PROGRAM *As of 2/27/17 WEDNESDAY, APRIL 26 Registration Wednesday 6:00 pm–9:00 pm — 8th Street South Welcome Mixer / Exhibit Hall Open 6:30 pm–9:00 pm — Salon C THURSDAY, APRIL 27 PAA Travel Award Recipients Breakfast 7:30 am–8:30 am — Lake Michigan Registration Thursday 7:00 am–5:00 pm — 8th Street South Exhibit Hall Open (Thursday) 8:00 am–6:30 pm — Salon D Speaker Ready Room Thursday 8:00 am–3:30 pm — Private Dining Room #7 Pres. Interviews 8:00 am–5:00 pm — Private Dining Room #5 P1 Health and Mortality 1 8:15 am–9:45 am — Salon D P1-1 Breast Cancer Among Immigrant Women: The Impact of Family Cancer History on Breast Cancer Prevention By Region of Birth Federico Martin Ghirimoldi, University of Texas at San Antonio P1-2 A Reversed Gender Pattern? a Meta-Analysis of Sex Differences in the Prevalence of Non- Suicidal Self-Injurious Behaviour Among Chinese Adolescents Yang Xueyan, Institute for Population and Development Studies, Xi'an Jiaotong University; Marcus Feldman, Morrison Institute for Population and Resource Studies P1-3 Age-Related Cataracts and Associated Risk Factors Among Elderly Population in India: Findings from a Large Scale Nationally Representative Cross-Sectional Survey Sutapa Agrawal, Public Health Foundation of India (PHFI); Jasmine Fledderjohann, Lancaster University P1-4 Protective but Not Sheltering: Educational Attainment and Poor Mental Health in the Great Recession Erik Liet Hernandez, Pennsylvania State University P1-5 Food Resources in Comal County: A Spatial Mismatch Daniela Krotzer, The University of Texas at San Antonio P1-6 Social Cohesion in Post-Apartheid South Africa: Any Implication for the Health of Adults? Emmanuel Olawale Olamijuwon, University of the Witwatersrand; Clifford O.