Vitamin a Deficiency
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

OCULAR MANIFESTATIONS of VITAMIN a DEFICIENCY*T
Br J Ophthalmol: first published as 10.1136/bjo.51.12.854 on 1 December 1967. Downloaded from Brit. J. Ophthal. (1967) 51, 854 OCULAR MANIFESTATIONS OF VITAMIN A DEFICIENCY*t BY G. VENKATASWAMY Department of Ophthalmology, Madurai Medical College, Madurai, India NUTRITIONAL deficiencies are a frequent cause of serious eye disease in India. Oomen (1961) reported a mortality of nearly 30 per cent. in young children with keratomalacia and an even higher proportion in those with protein malnutrition; about 25 per cent. of the survivors became totally blind, and about 60 per cent. were left with reduced vision in one or both eyes. Deficiency diseases revealed by dietary surveys have included xerophthalmia, Bitot's spots, angular stomatitis, and phrynoderma. Gilroy (1951) observed xerophthalmia in 250 out of 4,191 children from 44 estates in Assam. Sundararajan (1963) found signs of vitamin A deficiency in 35 to 45 per cent. of schoolchildren in Calcutta. Chandra, Venkatachalam, Belavadi, Reddy, and Gopalan (1960) reported that lack of protein and vitamin A was the most frequent cause of nutritional deficiency disorders in India; out of copyright. 14,563 children examined in a 5-year period, 2,245 showed malnutrition, 551 vitamin A deficiency, and 157 keratomalacia. Rao, Swaminathan, Swarup, and Patwardhan (1959) observed two to five cases ofvitamin A deficiency for every case ofkwashiorkor. A world-wide survey ofxerophthalniia carried out in nearly fifty countries (including countries in Asia) by WHO in 1962-1963 revealed that this was often the most important cause of blindness in young children. Scrimshaw (1959), McLaren (1963), and UNICEF (1963) concluded that vitamin A deficiency was one of the http://bjo.bmj.com/ main nutritional problems in tropical and subtropical areas. -

JMSCR Vol||08||Issue||02||Page 208-210||February 2020
JMSCR Vol||08||Issue||02||Page 208-210||February 2020 http://jmscr.igmpublication.org/home/ ISSN (e)-2347-176x ISSN (p) 2455-0450 DOI: https://dx.doi.org/10.18535/jmscr/v8i2.40 Keratomalacia - A Case Report Authors Deepthi Pullepu1*, Deepthi Janga2, V Murali Krishna3 *Corresponding Author Deepthi Pullepu Department of Ophthalmology, Rangaraya Medical College, Kakinada, Andhra Pradesh, India Abstract Xerophthalmia refers to an ocular condition of destructive dryness of conjunctiva and cornea caused due to severe vitamin A deficiency. Usually affects infants, children and women of reproductive age group. It is estimated to affect about one-third of children under the age of five around the world. Keratomalacia means dry and cloudy cornea which melts and perforates, caused due to severe vitamin A deficiency. Here we describe a case of 21 year old female with neurofibromatosis type 1 presenting with keratomalacia. Keywords: Vitamin A deficiency, Xerophthalmia, Keratomalacia. Introduction blindness is a significant contributor Vitamin A is essential for the functioning of the In India, it is estimated that there are immune system, healthy growth and development approximately 6.8 million people who have vision of body and is usually acquired through diet. less than 6/60 in at least one eye due to corneal Globally, 190 million children under five years of diseases; of these, about a million have bilateral age are affected by vitamin A deficiency involvement. They suffer from an increased risk of visual Corneal blindness resulting due to this disease can impairment, illness and death from childhood be completely prevented by institution of effective infections such as measles and those causing preventive or prophylactic measures at the diarrhoea community level. -

Abstract: a 19 Year Old Male Was Diagnosed with Vitamin a Deficiency
Robert Adam Young Abstract: A 19 year old male was diagnosed with vitamin A deficiency (VAD). Clinical examination shows conjunctival changes with central and marginal corneal ulcers. Patient history and lab testing were used to confirm the diagnosis. I. Case History 19 year old Hispanic Male Presents with chief complaint of progressive blur at distance and near in both eyes, foreign body sensation, ocular pain, photophobia, and epiphora; signs/symptoms are worse in the morning upon wakening. Started 6 months to 1 year ago, and has progressively gotten worse. Patient reports that the right eye is worse than the left eye. Ocular history of Ocular Rosacea Medical history of Hypoaldosteronism, Pernicious Anemia, and Type 2 Polyglandular Autoimmune Syndrome Last eye examination was two weeks ago at a medical center Presenting topical/systemic medications - Tobramycin TID OU, Prednisolone Acetate QD OU (has used for two weeks); Fludrocortisone (used long-term per PCP) Other pertinent info includes reports that patient cannot gain weight, although he has a regular appetite. Patient presents looking very slim, malnourished, and undersized for his age. II. Pertinent findings Entering unaided acuities are 20/400 OD with no improvement with pinhole; 20/50 OS that improves to 20/25 with pinhole. Pupil testing shows (-)APD; Pupils are 6mm in dim light, and constrict to 4mm in bright light. Ocular motilities are full and smooth with no reports of diplopia or pain. Tonometry was performed with tonopen and revealed intraocular pressures of 12 mmHg OD and 11 mmHG OS. Slit lamp examination shows 2+ conjunctival injection with trace-mild bitot spots both nasal and temporal, OU. -

Vitamins a and E and Carotenoids
Fat-Soluble Vitamins & Micronutrients: Vitamins A and E and Carotenoids Vitamins A (retinol) and E (tocopherol) and the carotenoids are fat-soluble micronutrients that are found in many foods, including some vegetables, fruits, meats, and animal products. Fish-liver oils, liver, egg yolks, butter, and cream are known for their higher content of vitamin A. Nuts and seeds are particularly rich sources of vitamin E (Thomas 2006). At least 700 carotenoids—fat-soluble red and yellow pigments—are found in nature (Britton 2004). Americans consume 40–50 of these carotenoids, primarily in fruits and vegetables (Khachik 1992), and smaller amounts in poultry products, including egg yolks, and in seafoods (Boylston 2007). Six major carotenoids are found in human serum: alpha-carotene, beta-carotene, beta-cryptoxanthin, lutein, trans-lycopene, and zeaxanthin. Major carotene sources are orange-colored fruits and vegetables such as carrots, pumpkins, and mangos. Lutein and zeaxanthin are also found in dark green leafy vegetables, where any orange coloring is overshadowed by chlorophyll. Trans-Lycopene is obtained primarily from tomato and tomato products. For information on the carotenoid content of U.S. foods, see the 1998 carotenoid database created by the U.S. Department of Agriculture and the Nutrition Coordinating Center at the University of Minnesota (http://www.nal.usda.gov/fnic/foodcomp/Data/car98/car98.html). Vitamin A, found in foods that come from animal sources, is called preformed vitamin A. Some carotenoids found in colorful fruits and vegetables are called provitamin A; they are metabolized in the body to vitamin A. Among the carotenoids, beta-carotene, a retinol dimer, has the most significant provitamin A activity. -

Current Health Issues in the Caribbean BLINDNESS in THE
Current Health Issues in the Caribbean BLINDNESS IN THE CARIBBEAN Alfred L. Anduze, M.D. St. Croix Vision Center St. Croix Hospital St. Croix U.S. Virgin Islands Caribbean Studies Association Merida, Mexico May 26, 1994 Abstract: Blindness in the Caribbean Background: The prevailing of blindness in the Caribbean region are reviewed in the context of world blindness statistics to identify differences and similarities that might exist. Method: A review of the status of blindness in the U.S. Virgin Islands, Barbados, Jamaica, Puerto Rico, Trinidad, and Mexico; individually with regard to causal etiology, epidemiology, treatment and possible future research. Results: Blindness in the Caribbean is the result of genetics, tropical environment and cultural habits of the inhabitants and consist of Age-related macular disease, Infectious diseases, Diabetes mellitus, Glaucoma, Congenital defects, Xerophthalmia, Trachoma, Trauma and Cataracts. Conclusion: There are almost 50 million people who are legally blind worldwide (i.e. with a vision of 20/200 or less) 2-3 million in the Caribbean region. The social and economic consequences are serious additional deterrents in developing countries. Outline: Causes of Blindness in the Caribbean I. Age-related macular disease a. Vascular insufficiency b. Senile macular degeneration II. Cataracts III. Glaucoma IV. Diabetes mellitus V. Infectious diseases a. Trachoma b. Onchocerciasis c. Leprosy d. Toxoplasmosis e. Toxocariasis f. AIDS VI. Trauma a. industrial/work-related b. sports c. home accidents VII. Nutritional a. Xerophthalmia/keratomalacia b. Iron-deficiency anemia c. Tobacco/Alcohol Retinopathy VIII. Congenital defects a. genetic syndromes b. strabismus Legal blindness is acceptably defined as vision 20/200 (6/60) or less. -
2002 Samel 10 Most Common Systemic Health Conditions with A
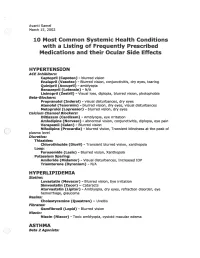
Avanti Samel / March 15, 2002 10 Most Common Systemic Health Conditions with a Listing of Frequently Prescribed Medications and their Ocular Side Effects HYPERTENSION ACE Inhibitors: Captopril (Capoten}- blurred vision Enalapril (Vasotec) - Blurred vision, conjunctivitis, dry eyes, tearing Quinipril (Accupril)- amblyopia Benazepril (Lotensin)- N/A Lisinopril (Zestril) - Visual loss, diplopia, blurred vision, photophobia Beta-Blockers: Propranolol (Inderal)- visual disturbances, dry eyes Atenolol (Tenormin)- blurred vision, dry eyes, visual disturbances Metoprolol (Lopressor) - blurred vision, dry eyes calcium Channel Blockers: Diltiazem (Cardizem)- Amblyopia, eye irritation Amlodipine (Norvasc)- abnormal vision, conjunctivitis, diplopia, eye pain Verapamil (Calan)- Blurred vision Nifedipine (Procardia) - blurred vision, Transient blindness at the peak of plasma level · Diuretics: Thiazides: Chlorothiazide (Diuril) - Transient blurred vision, xanthopsia Loop: Furosemide (Lasix) - Blurred vision, Xanthopsia Potassium Sparing: Amiloride (Midamor) - Visual disturbances, Increased lOP Triamterene (Dyrenium)- N/A HYPERLIPIDEMIA Statins: Lovastatin (Mevacor) - Blurred vision, Eye irritation Simvastatin (Zocor)- Cataracts Atorvastatin (Lipitor)- Amblyopia, dry eyes, refraction disorder, eye hemorrhage, glaucoma Resins: Cholestyramine (Questran)- Uveitis Fibrates: Gemfibrozil (Lopid)- Blurred vision Niacin: Niacin (Niacor) - Toxic amblyopia, cystoid macular edema ASTHMA ( ) Beta 2 Agonists: Albuterol (Proventil) - N/A ( Salmeterol (Serevent)- -

© Alan Macfarlane and Gerry Martin, 2002 1 MYOPIA: ITS
© Alan Macfarlane and Gerry Martin, 2002 MYOPIA: ITS COMPARATIVE INCIDENCE AND PROBABLE CAUSES What Rasmussen encountered in his many years of working with Chinese eye problem astonished him. He summarized his impressions thus. 'Three facts stand out clearly in both ancient and modern records of Chinese eyesight: one that they are a highly myopic nation; two that keratomalacia is the major cause of ocular disease; and three that presbyopia is earlier than in the West by about five years. They stand out against an historical background of neglect and abuse, malnutrition, and centuries of State indifference.' (p.48) Moving on to the statistics of myopia, he summarized the research of a quarter of a century by saying that 'only 20 per cent. of all lenses supplied by the ancients, and similar amount by the moderns (excluding high astigmatic) were for old-sight lenses. It is the other 80 per cent. that matters; the 65 per cent. for myopia and the 15 per cent. for glare and therapeutics.' (p.20) Elsewhere he gives slightly different statistics, which applied to those aged under forty years, showed that approximately 75 per cent. of the lenses were supplied for myopia. In a detailed table he presents the figures; in the 'Ancient Chinese Sight Records', 65% were for myopia; in the 'Modern Chinese Sight Records' myopia (simple) or with astigmatism combined accounted for 70% of the lenses.(p.48) The second figure of 70% was based on 120,000 case histories collected by Rasmussen and his colleagues over a period of 25 years. (p.49) The significance of the degree of myopia only comes out if we compare the Chinese figures with those for other nationalities. -

Vitamin a Information Vitamin a Deficiency (VAD) Is the Leading
Vitamin A Information Vitamin A deficiency (VAD) is the leading cause of preventable blindness in children. Xerophthalmia, which is abnormal dryness of the conjunctiva and cornea of the eye, is associated with VAD and when left untreated can lead to blindness. The World Health Organization estimates that worldwide there are “at least 254 million children under the age of five that are at-risk in terms of their health and survival”. An estimated 250,000 to 500,000 vitamin A deficient children become blind each year. Half of these children die within 12 months of losing their sight. Although this problem is most prevalent in Africa and South East Asia, it is certainly existent throughout the developing nations. According to UNICEF, “Of 82 countries deemed ‘priorities’ for national-level vitamin A supplementation programs, 57 had coverage estimates available for 2014. Half of these 57 countries achieved the recommended coverage of 80 percent.” As a result, half did not receive the 80 percent level, and for those that did, a significant number of children remained untreated. While the problem is most prevalent in Africa and South East Asia, central American countries are also at risk. “About 40% of Mexican children in rural areas had deficient values of plasma vitamin A” (Rosado, 1995). Furthermore, it was noted as far back as 1989 that vitamin A deficient Guatemalan children grow poorly, are more anemic, have more infections and are more likely to die than their peers (Sommer, 1989). The World Health Organization recommends that all children between the ages of six months and six years in developing nations that are at risk receive vitamin A supplementation. -

The Main Causes of Blindness and Low Vision in School for Blind
26ORIGINAL ARTICLE DOI 10.5935/0034-7280.20160006 The main causes of blindness and low vision in school for blind As principais causas de cegueira e baixa visão em escola para deficientes visuais Abelardo Couto Junior1, Lucas Azeredo Gonçalves de Oliveira2 ABSTRACT Objective: Identify and analyze the main causes of blindness and low vision in school for blind. Methods: One hundred sixty-five medical records of visually impaired students were reviewed in an institution specialized in teaching the blind, treated between august 2013 and may 2014. The variables analyzed were age, sex, visual acuity, primary and secondary diagnoses, treatment, optical prescription features and prognosis. Results: 165 students were evaluated, 91 students (55%) are legally blind and only 74 (45%) of the students are classified as low vision. The main causes of blindness were: retinopathy of prematurity (21%), optic nerve atrophy (18%), congenital glaucoma (16%), retinal dystrophy (11%) and cancer (8%). The causes of low vision were: congenital cataract (18%), congenital glaucoma (15%) and retinochoroidal scarring (12%). Conclusion: The main causes of blindness and low vision in the Benjamin Constant Institute are from preventable diseases. Keywords: Blindness; Low vision; Visual acuity; Child; Health school RESUMO Objetivo: Identificar e analisar as principais causas de cegueira e baixa visão em escola para deficientes visuais. Métodos: Foram revisados 165 prontuários de alunos portadores de deficiência visual em instituição especializada no ensino de cegos, atendidos no período de agosto de 2013 a maio de 2014. As variáveis analisadas foram: idade, gênero, acuidade visual, diagnóstico principal e secundário, tratamento, recursos ópticos prescritos e prognóstico. Resultados: Dos 165 alunos avaliados, 91 alunos (55%) são legalmente cegos e apenas 74 (45%) dos alunos são enquadrados como baixa visão. -

Ophthaproblem
Pratique clinique Clinical Pract ice Ophthaproblem Shaun Segal Sanjay Sharma, MD, MSC, MBA, FRCSC : Ophthalmic Photography : Ophthalmic Photography Photo credit Photo Dieu Hotel University, Laboratory of Queen’s Kingston, Ont. Hospital, 30-year-old woman had been admitted to hospital in infancy with diarrhea, steatorrhea, and failure to thrive. During late childhood, she developed atypi- Acal retinitis pigmentosa involving the retina and a progressive ataxic neuropathy. Investigations showed her serum lacked beta-lipoprotein and her red corpuscles had a spiky shape. Recent ophthalmic examination revealed substantial choroidal atrophy around the disk and a speckled peripheral fundus. Which vitamins should this patient be given as therapy for her disorder? 1. Vitamin A 2. Vitamin E 3. Vitamin C 4. Vitamin B Answer on page 1085 Mr Segal is a medical student at Queen’s University in Kingston, Ont. Dr Sharma is an Associate Professor of Ophthalmology and an Assistant Professor of Epidemiology at Queen’s University VOL 5: AUGUST • AOÛT 2005 d Canadian Family Physician • Le Médecin de famille canadien 1079 Pratique clinique Clinical Pract ice Answer to Ophthaproblem continued from page 1079 1. Vitamin A and 2. vitamin E Th is patient has abetalipoproteinemia (ABL), some- times called Bassen-Kornzweig syndrome,1 a dis- ease characterized by malabsorption of fat. The condition is treated with supplements of the two fat-soluble vitamins A and E. Abetalipoproteinemia manifests itself through signs of lipid malabsorp- tion, dense contracted red blood -

Micronutrient Malnutrition – Detection, Measurement and Intervention: a Training Package for Field Staff Handouts for Group Tr
Micronutrient Malnutrition – Detection, Measurement and Intervention: A Training Package for Field Staff Compiled by the Institute of Child Health Handouts for Group Training For UNHCR Version 1 2003 ICH/UNHCR Handout Contents Section 1: Section 2: Section 3: Important Micronutrient Detection Nutrition Concepts Deficiency Diseases and Prevention 1. Food and Nutrition 1. Anaemia 1. Detection of Deficiencies 2. Nutritional Requirements 2. Vitamin A Deficiency 2. Intervention 3. Nutritional Deficiencies 3. Iodine Deficiency Disorders 4. Micronutrient Deficiency Disease 4. Beriberi 5. Nutritional Assessments 5. Ariboflavinosis 6. Causes of Malnutrition 6. Pellagra 7. Scurvy 8. Rickets ICH/UNHCR Handout 2 Section 1 Food and Nutrition • All people and animals need food to live, grow and be healthy. • Food contains different types of nutrients. • Food contains certain nutrients called macronutrients: – Fat – Carbohydrate – Protein • Food also contains nutrients called micronutrients: – Vitamins – Minerals • A good diet is made up of foods that contain all these types of nutrients – macronutrients and micronutrients. ICH/UNHCR Handout 3 Section 1 Nutritional Requirements For people to be healthy and productive they need a certain amount of nutrients. This is called their nutritional requirement. • The amount of energy that people get from their food is measured in kilo calories (kcal). • The average person needs about 2100 kcal each day • 17-20 % of this energy should come from fat • At least 10 % of this energy should come from protein • People also need certain amounts of vitamins and minerals • For example the average person should have at least 12 mg of the B vitamin niacin, 28 mg of vitamin C, and 22 mg of iron each day. -

Prevalence and Causes of Low Vision and Blindness Worldwide
S Afr Optom 2005 64 (2) 44 − 54 Prevalence and causes of low vision and blindness worldwide AO Oduntan* Department of Optometry, University of Limpopo, Private Bag X1106, Sovenga, 0727 South Africa <[email protected]> Abstract Introduction A recent review of the causes and prevalence There are many low vision and blind people of low vision and blindness world wide is lack- worldwide, and there is a considerable amount of ing. Such review is important for highlighting data available on the prevalence of low vision and the causes and prevalence of visual impairment blindness in many parts of the world. The data, in the different parts of the world. Also, it is however, vary significantly from one continent to important in providing information on the types another. In 1995, the World Health Organization and magnitude of eye care programs needed in (WHO) Task Force on data on blindness estimated different parts of the world. In this article, the that there were 37.1 million blind people world- causes and prevalence of low vision and blind- wide, indicating a global prevalence of 0.7 percent1. ness in different parts of the world are reviewed According to that report, the prevalence values and the socio-economic and psychological range from 0.3% in the developed countries to implications are briefly discussed. The review 1.4% in Sub-Saharan African countries. The preva- is based on an extensive review of the litera- lence of visual impairment is expected to be higher ture using computer data bases combined with in the developing countries due to the low level of review of available national, regional and inter- health care services in many of the countries.