Proceedings Science Week 2013
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MAC1 Abstracts – Oral Presentations
Oral Presentation Abstracts OP001 Rights, Interests and Moral Standing: a critical examination of dialogue between Regan and Frey. Rebekah Humphreys Cardiff University, Cardiff, United Kingdom This paper aims to assess R. G. Frey’s analysis of Leonard Nelson’s argument (that links interests to rights). Frey argues that claims that animals have rights or interests have not been established. Frey’s contentions that animals have not been shown to have rights nor interests will be discussed in turn, but the main focus will be on Frey’s claim that animals have not been shown to have interests. One way Frey analyses this latter claim is by considering H. J. McCloskey’s denial of the claim and Tom Regan’s criticism of this denial. While Frey’s position on animal interests does not depend on McCloskey’s views, he believes that a consideration of McCloskey’s views will reveal that Nelson’s argument (linking interests to rights) has not been established as sound. My discussion (of Frey’s scrutiny of Nelson’s argument) will centre only on the dialogue between Regan and Frey in respect of McCloskey’s argument. OP002 Can Special Relations Ground the Privileged Moral Status of Humans Over Animals? Robert Jones California State University, Chico, United States Much contemporary philosophical work regarding the moral considerability of nonhuman animals involves the search for some set of characteristics or properties that nonhuman animals possess sufficient for their robust membership in the sphere of things morally considerable. The most common strategy has been to identify some set of properties intrinsic to the animals themselves. -

Understanding Human Factors Involved in the Unwanted Cat Problem
UNDERSTANDING HUMAN FACTORS INVOLVED IN THE UNWANTED CAT PROBLEM Sarah Jane Maria Zito BVetMed MANZCVS (feline medicine) A thesis submitted for the degree of Doctor of Philosophy at The University of Queensland in 2015 School of Veterinary Science I Abstract The large number of unwanted cats in many modern communities results in a complex, worldwide problem causing many societal issues. These include ethical concerns about the euthanasia of many healthy animals, moral stress for the people involved, financial costs to organisations that manage unwanted cats, environmental costs, wildlife predation, potential for disease spread, community nuisance, and welfare concerns for cats. Humans contribute to the creation and maintenance of unwanted cat populations and also to solutions to alleviate the problem. The work in this thesis explored human factors contributing to the unwanted cat problem—including cat ownership perception, cat caretaking, cat semi-ownership and cat surrender—and human factors associated with cat adoption choices and outcomes. To investigate human factors contributing to the unwanted cat problem, data were collected from 141 people surrendering cats to four animal shelters. The aim was to better understand the people and human-cat relationships involved, and ultimately to inform strategies to reduce shelter intake. Participants were recruited for this study when they surrendered a cat to a shelter and information was obtained on their demographics, cat interaction history, cat caretaking, and surrender reasons. This information was used to describe and compare the people, cats, and human-cat relationships contributing to shelter intake, using logistic regression models and biplot visualisation techniques. A model of cat ownership perception in people that surrender cats to shelters was proposed. -

ANIMAL SPIRIT the Animal Interfaith Alliance Magazine Spring 2018 - Issue 8
ANIMAL SPIRIT The Animal Interfaith Alliance Magazine Spring 2018 - Issue 8 Faiths Working Together for Animals In This Issue: Animals and the Law Animal Rights, Unnecessary Suffering and Our Dominion - Prof. Gary Francione & Prof. Anna Charlton The Law and Campaigning for Animal Protection - David Thomas Save the Asian Elephant: Interview with Duncan McNair KHS - Abigail Scott Presentation to the European Parliament on REACH - Dr Andre Menache Bees-at-Law - Noël Sweeney New Animal Welfare Bill & Labour’s Animal Welfare Plan Special Feature: Vijay Shah - A Jain, a Vegan and an Astronaut Contender www.animal-interfaith-alliance.com 1 People Member Organisations President: - Satish Kumar (Jain) Anglican Society for the Welfare of Animals (ASWA) - www.aswa.org.uk Vice-President: - Dr Deborah Jones Animals in Islam - www.animalsinislam.com (Vice Chair - CCA) The Bhagvatinandji Education & Health Trust - www.beht.org Catholic Concern for Animals (CCA) - www.catholic-animals.com Patrons: Christian Vegetarians & Vegans UK - www.christian-vegetariansvegans.org.uk Kay, Duchess of Hamilton Christian Vegetarian Association (CVA US) - www.christianveg.org Rev. Christa Blanke (Christian) Dharma Voices for Animals (DVA) (Buddhist) - www.dharmavoicesforanimals.org Joyce D’Silva (Ambassador CIWF) Institute of Jainology (IOJ) - www.jainology.org Nitin Mehta MBE (Jain) Dr André Menache (Jewish) The Jewish Vegetarian Society (JVS) - www.jvs.org Dr Alpesh Patel (Hindu) The Mahavir Trust Dr Matthieu Ricard (Buddhist) Oshwal Association of the UK (OAUK) - www.oshwal.co.uk Dr Richard D. Ryder (Ethicist) Pan-Orthodox Concern for Animals - www.panorthodoxconcernforanimals.org Anant Shah (Jain) Quaker Concern for Animals (QCA) - www.quaker-animals.co.uk Muhammad Safa (Muslim) Sadhu Vaswani Centre (Hindu) - www.sadhuvaswani.org Ajit & Charanjit Singh MBE (Sikh) The Young Jains - www.youngjains.org.uk Board: Rev. -

Evaluation of the Predictive Validity of the Behavioural Assessment for Re-Homing K9’S (B.A.R.K.) Protocol and Owner Satisfaction with Adopted Dogs
Accepted Manuscript Title: Evaluation of the predictive validity of the behavioural assessment for re-homing K9’s (B.A.R.K.) protocol and owner satisfaction with adopted dogs Author: Kate M. Mornement Grahame J. Coleman Samia R. Toukhsati Pauleen C. Bennett PII: S0168-1591(15)00099-4 DOI: http://dx.doi.org/doi:10.1016/j.applanim.2015.03.013 Reference: APPLAN 4057 To appear in: APPLAN Received date: 30-9-2014 Revised date: 22-3-2015 Accepted date: 28-3-2015 Please cite this article as: Mornement, K.M., Coleman, G.J., Toukhsati, S.R., Bennett, P.C.,Evaluation of the predictive validity of the behavioural assessment for re-homing K9’s (B.A.R.K.) protocol and owner satisfaction with adopted dogs., Applied Animal Behaviour Science (2015), http://dx.doi.org/10.1016/j.applanim.2015.03.013 This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. 1 Highlights 2 3 We examine the predictive validity of the B.A.R.K. protocol 4 B.A.R.K. predicted fearful and friendly behaviour post adoption 5 Problem behaviour and aggression post adoption were not predicted by B.A.R.K. 6 About 25% of adopted dogs assessed by B.A.R.K. -

Animals, Moral Risk and Moral Considerability
Durham E-Theses Animals, moral risk and moral considerability Tanner, Julia K. H. How to cite: Tanner, Julia K. H. (2007) Animals, moral risk and moral considerability, Durham theses, Durham University. Available at Durham E-Theses Online: http://etheses.dur.ac.uk/2477/ Use policy The full-text may be used and/or reproduced, and given to third parties in any format or medium, without prior permission or charge, for personal research or study, educational, or not-for-prot purposes provided that: • a full bibliographic reference is made to the original source • a link is made to the metadata record in Durham E-Theses • the full-text is not changed in any way The full-text must not be sold in any format or medium without the formal permission of the copyright holders. Please consult the full Durham E-Theses policy for further details. Academic Support Oce, Durham University, University Oce, Old Elvet, Durham DH1 3HP e-mail: [email protected] Tel: +44 0191 334 6107 http://etheses.dur.ac.uk Animals, Moral Risk and Moral Considerability The copyright of this thesis rests with the author or the university to which it was submitted. No quotation from it, or information derived from it may be published without the prior written consent of the author or university, and any information derived from it should be acknowledged. Name: Julia K. H. Tanner Degree for which thesis is being submitted: Ph.D University: University of Durham Department: Philosophy Department Year of submission: 2007 The copyright of this thesis rests with the author. -

The Canadian Veterinary Journal La Revue Vétérinaire Canadienne Hydronephrosis in a Dairy Calf: a Diagnosis Delayed by a Clinician’S Bayesian Brain Reasoning
October/Octobre 2018 The Canadian Veterinary Journal La Revue vétérinaire canadienne Vol. 59,Vol. No. 10 October/Octobre 2018 Volume 59, No. 10 The Canadian Veterinary Journal Canadian Veterinary The Hydronephrosis in a dairy calf: A diagnosis delayed by a clinician’s Bayesian brain reasoning Radiation therapy for the treatment of canine progressive cutaneous angiomatosis: Description of 2 cases Successful surgical resolution of a ceco- cecal intussusception in a 15-month-old Angus heifer Occult tonsillar squamous cell carcinoma La Revue vétérinaire canadienneLa Revue vétérinaire in 2 dogs presenting for treatment of primary oral squamous cell carcinoma Successful management of doxorubicin overdose and extravasation in a dog with lymphoma Urinary bladder herniation through inguinal ring in a female cat Radiotherapy and pasireotide treatment of a growth hormone producing pituitary tumor in a diabetic dog Fracture-associated osteosarcoma of the femur in a cat Antimicrobial resistance in mastitis, respiratory and enteric bacteria isolated from ruminant animals from the Atlantic Provinces of Canada from 1994–2013 Overlooked sources of Salmonella contamination in the pig production network: Slaughterhouse yard pathways and mudguards and carpets from transport trucks Serological survey of canine vector-borne diseases in Saskatchewan, Canada Assessing the sharpness of hypodermic needles after repeated use FOR PERSONAL USE ONLY ONE ESSENTIAL SOLUTION FOR LIGHTER1, BRIGHTER DAYS NEW OBESITY+URINARY Formulated to help dissolve struvite stones & reduce 1 the risk of struvite and calcium oxalate stones With omega-3s from fish oil to helpreduce inflammation 2 associated with conditions such as UTI and stones Formulated with the nutrition of Metabolic, 3 proven to reduce weight by 13% in 60 days1 Now get the nutrition of c/d® Multicare combined with the proven weight loss power of Metabolic. -
Exploring Human – Animal Interactions a Multidisciplinary Approach from Behavioral and Social Sciences
Proceedings Exploring Human – Animal Interactions a multidisciplinary approach from behavioral and social sciences Barcelona 7th – 10th of July 2016 INTRODUCTION Vision, Goals and Objectives Animals were domesticated thousands of years ago and are now present in almost every human society around the world. Nevertheless, only recently scientists have begun to analyse both positive and negative aspects of human-animal relationships. For centuries people have recognised the value of animals for obvious economical reasons, but also as an important source of physical and emotional wellbeing. Indeed, people’s attitudes towards animals depend on a variety of factors, including socio-economical relationships with each particular species, cultural background, religious believes, as well as individual differences regarding behaviour and personality. A proper understanding of these differences requires a multidisciplinary approach, from psychology, social psychology and anthropology to psychiatry and neuroscience. The main goal of the conference would be to provide delegates with an updated and multi-disciplinary overview of human-animal interactions. Selected topics would include but are not limited to: • The concept of empathy in the study of human-animals interactions. • The concept of protected values (or sacred values) in human-animal interactions. • Understanding cultural views on animals. We will also organise a Satellite Meeting (10th of July) on the state of the art of the abandonment of companion animals and global strategies to prevent the abandonment. ISAZ grateFULLY acKnoWLedges the generous support OF the 2016 conFerence FroM the FOLLOWing sponsors and COLLaborators Sponsors Collaborators 2 PROGRAM Thursday 7th July Friday 8th July 19:00 – 20:30 8:00 – 18:30 Welcome Ceremony Registration at the PRBB Barcelona City Council 9:00 – 9:15 Opening address 9:15 – 10:15 Keynote Speaker Dr. -

Pigeon Barbara Allen
Pigeon Barbara Allen Animal series Pigeon Animal Series editor: Jonathan Burt Already published Crow Fox Spider Boria Sax Martin Wallen Katja and Sergiusz Michalski Ant Fly Pig Charlotte Sleigh Steven Connor Brett Mizelle Tortoise Cat Camel Peter Young Katharine M. Rogers Robert Irwin Cockroach Peacock Chicken Marion Copeland Christine E. Jackson Annie Potts Dog Cow Wolf Susan McHugh Hannah Velten Garry Marvin Oyster Duck Ape Rebecca Stott Victoria de Rijke John Sorenson Bear Shark Butterfly Robert E. Bieder Dean Crawford Matthew Brower Bee Swan Sheep Claire Preston Peter Young Philip Armstrong Rat Rhinoceros Giraffe Jonathan Burt Kelly Enright Mark Williams Snake Horse Eagle Drake Stutesman Elaine Walker Ron Broglio Falcon Elephant Jellyfish Helen Macdonald Daniel Wylie Eva Hayward Whale Moose Penguin Joe Roman Kevin Jackson Stephen Martin Parrot Eel Owl Paul Carter Richard Schweid Desmond Morris Tiger Susie Green Forthcoming Salmon Hare Peter Coates Simon Carnell Pigeon Barbara Allen reaktion books For David, for Rhys (thank you for bringing home an injured squab during the writing of this book), and for my feathered friends, named (Bacardi, Chagall, Bert, Celeste, Olympia and Splash) and unnamed; you are truly magnificent! Published by reaktion books ltd 33 Great Sutton Street London ec1v 0dx, uk www.reaktionbooks.co.uk First published 2009 Copyright © Barbara Allen 2009 This book has been published with the assistance of the Australian Academy of the Humanities All rights reserved No part of this publication may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the prior permission of the publishers. -
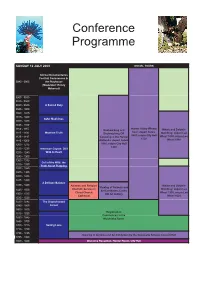
Conference Programme
Conference Programme SUNDAY 12 JULY 2009 SOCIAL TOURS Animal Documentaries Festival Commences in 0845 - 0900 the Playhouse (Moderator: Randy Malamud) 0900 - 0915 0915 - 0930 0930 - 0945 A Sacred Duty 0945 - 1000 1000 - 1015 1015 - 1030 Safer Medicines 1030 - 1045 1045 - 1100 1100-1115 Hunter Valley Winery Bushwalking and Whale and Dolphin Tour: depart hotels 1115 - 1130 Meat the Truth Birdwatching OR Watching: depart Lee 0845, return City Hall 1130 - 1145 Canoeing in the Hunter Wharf 1000, return Lee 1530 1145 - 1200 Wetlands: depart hotels Wharf 1300 1200 - 1215 0900, return City Hall 1430 1215 - 1230 American Coyote: Still 1230 - 1245 Wild At Heart 1245 - 1300 1300 - 1315 Cull of the Wild: the 1315 - 1330 Truth About Trapping 1330 - 1345 1345 - 1400 1400 - 1415 1415 - 1430 A Delicate Balance 1430 - 1445 Animals and Religion Whale and Dolphin Viewing of Animals and Interfaith Service in Watching: depart Lee 1445 - 1500 Art Exhibition, Cooks Christ Church Wharf 1330, return Lee 1500 - 1515 Hill Art Gallery Cathedral Wharf 1630 1515 - 1530 1530 - 1545 The Disenchanted 1545 - 1600 Forest 1600 - 1615 Registration 1615 - 1630 Commences in the 1630 - 1645 Mulubinba Room 1645 - 1700 1700 - 1715 Saving Luna 1715 - 1730 1730 - 1745 Viewing of Animals and Art Exhibition by the Newcastle School, Concert Hall 1745 - 1800 1800 - 1930 Welcome Reception, Hunter Room, City Hall MONDAY 13 JULY 2009 Banquet Room 0800 - 0900 Registration Concert Hall 0900 - 0905 Introductions: Rod Bennison and Jill Bough, Minding Animals Conference Co-convenors, Animals -

People & Animals – for Life
PEOPLE & ANIMALS – FOR LIFE The Conference is hosted on behalf of the International Association of Human-Animal Interaction Organizations by the Swedish IAHAIO members 12th International IAHAIO Conference JULY 1-4, 2010 STOCKHOLM, SWEDEN Venue: City Conference Center - Folkets Hus in Stockholm Website: www.iahaio2010.com Abstract Book Major Sponsors 2 Table of Contents Plenary Sessions 4 Plenary 1-9 5 Oral Sessions (Thursday July 1) 14 Oral 1-12 15 Oral Sessions (Friday July 2) 27 Oral 13-42 28 Oral Sessions (Saturday July 3) 57 Oral 43-66 58 Oral Sessions (Sunday July 4) 82 Oral 67-87 83 Workshops 104 Workshops 1-17 105 Poster Sessions 122 Poster 1-40 123 All abstracts are published exactly as their respective authors wrote them. © IAHAIO and respective authors. 3 Plenary Sessions Abstract from Plenary speakers 4 Plenary session 1 Some We Love, Some We Hate, Some We Eat: Why It’s So Hard to Think Straight about Animals Harold Herzog Professor, Western Carolina University Our attitudes toward non-human animals are often morally incoherent. How can most Americans claim WKH\VXSSRUWWKHDLPVRIWKHDQLPDOULJKWVPRYHPHQW\HWRIDGXOWVLQWKH8QLWHV6WDWHVHDWÁHVK":K\ GRZHORYHFDWVDQGKDWHUDWV":K\DUHGRJVWUHDWHGDVIDPLO\PHPEHUVLQVRPHFRXQWULHVDQGHDWHQIRU GLQQHULQRWKHUV",QWKLVSUHVHQWDWLRQ,ZLOOXVHUHFHQWÀQGLQJVIURPDQWKURSRORJ\SV\FKRORJ\DQGEUDLQ science to examine why human interactions with other species are so fraught with inconsistency. 2XUWKLQNLQJDERXWQRQKXPDQDQLPDOVUHÁHFWVDFRPSOH[PL[RIJHQHWLFFXOWXUDODQGFRJQLWLYHIDFWRUV These include biophilia and biophobia, learning, language, and the tendency for human decision-making to rely on quick and dirty rules of thumb. I will argue that the social intuitionist model of moral judgment (Haidt, 2001) helps explain why our relationships with other species are so ethically messy. This theory holds WKDWPRUDOGHFLVLRQVLQYROYHWZRGLVWLQFWDQGRIWHQFRQÁLFWLQJSURFHVVHV7KHÀUVWLVUDSLGXQFRQVFLRXVDQG intuitive, while the second is slow, conscious and logical. -

Research Group, Monash University Editorial Committee: Timothy Adams Bvsc (Hons), Petcare Information and Advisory Service
Shelresearcterh 12th Edition: 2010 Editor: Kate Mornement BSc (Hons), PhD student, Building on your Anthrozoology Research Group, Monash University Editorial Committee: Timothy Adams BVSc (Hons), Petcare Information and Advisory Service strengths within the PhD Dr. Pauleen Bennett , Founder, Anthrozoology Research Group, Monash University Dr. Linda Marston PhD, Research Fellow, shelter environment Anthrozoology Research Group, Monash University by Vanessa Rohlf What is positive psychology? Positive psychology is a new and rapidly growing field of Psychology. Unlike traditional models of Psychology, Positive Psychology is concerned with the study of optimal human functioning rather than pathology. Basically positive psychologists are concerned with understanding and promoting happiness. Understanding and Promoting Happiness According to the founder of Positive Psychology, Martin Seligman, there are three ways to be happy; Pleasure, Engagement and Meaning (Seligman, 2002). Pleasure – is all about increasing positive emotions. Positive emotions can be increased by focusing on Promoting happiness in the workplace the past, present or future. We can People spend on average a third of their lives at work so it is experience positive emotions about extremely important to cultivate happiness in the workplace. the past by practicing gratitude. Working in an animal shelter is no different – especially when Positive emotions about the present you often have to deal with unhappy situations. Research also can be experienced by savouring (e.g. indicates that there may be a flow on effect. Satisfaction with savouring the taste of a chocolate bar). work is associated with life satisfaction as well as reduced Positive emotions about the future can levels of conflict in the home (Diener & Seligman, 2004). -

Co-Sleeping Between Adolescents and Their Pets May Not Impact Sleep Quality
Article Co-Sleeping between Adolescents and Their Pets May Not Impact Sleep Quality Jessica Rosano 1, Tiffani Howell 1,*, Russell Conduit 2 and Pauleen Bennett 1 1 Anthrozoology Research Group, School of Psychology and Public Health, La Trobe University, Bendigo, VIC 3552, Australia; [email protected] (J.R.); [email protected] (P.B.) 2 School of Health and Biomedical Sciences, RMIT University, Melbourne, VIC 3083, Australia; [email protected] * Correspondence: [email protected] Abstract: Pet–owner co-sleeping is increasingly common in some parts of the world. Adult owners often subjectively report benefits of co-sleeping with pets, although objective actigraphy reports conversely indicate sleep disruptions due to the pet. Because limited research is available regarding pet–owner co-sleeping in non-adult samples, the aim of this two-part study was to explore whether co-sleeping improves sleep quality in adolescents, an age group in which poor sleep patterns are well documented. In Study One, an online survey with 265 pet-owning 13-to-17-year-old participants found that over 78% co-slept with their pet. Average sleep quality scores for co-sleepers and non- co-sleepers indicated generally poor sleep, with no differences in sleep quality depending on age, gender, or co-sleeping status. Study Two consisted of two preliminary case studies, using actigraphy on dog–adolescent co-sleepers. In both cases, high sleep concordance was observed, but owners again experienced generally poor sleep quality. Future actigraphy research is needed, including larger sample sizes and a control group of non-co-sleepers, to validate the preliminary findings from this study, but our limited evidence suggests that co-sleeping with a pet may not impact sleep quality in adolescents.