Antidepressive Agents Improve Symptoms and Reduce Pain in Patients with Functional Gastrointestinal Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Appendix A: Potentially Inappropriate Prescriptions (Pips) for Older People (Modified from ‘STOPP/START 2’ O’Mahony Et Al 2014)
Appendix A: Potentially Inappropriate Prescriptions (PIPs) for older people (modified from ‘STOPP/START 2’ O’Mahony et al 2014) Consider holding (or deprescribing - consult with patient): 1. Any drug prescribed without an evidence-based clinical indication 2. Any drug prescribed beyond the recommended duration, where well-defined 3. Any duplicate drug class (optimise monotherapy) Avoid hazardous combinations e.g.: 1. The Triple Whammy: NSAID + ACE/ARB + diuretic in all ≥ 65 year olds (NHS Scotland 2015) 2. Sick Day Rules drugs: Metformin or ACEi/ARB or a diuretic or NSAID in ≥ 65 year olds presenting with dehydration and/or acute kidney injury (AKI) (NHS Scotland 2015) 3. Anticholinergic Burden (ACB): Any additional medicine with anticholinergic properties when already on an Anticholinergic/antimuscarinic (listed overleaf) in > 65 year olds (risk of falls, increased anticholinergic toxicity: confusion, agitation, acute glaucoma, urinary retention, constipation). The following are known to contribute to the ACB: Amantadine Antidepressants, tricyclic: Amitriptyline, Clomipramine, Dosulepin, Doxepin, Imipramine, Nortriptyline, Trimipramine and SSRIs: Fluoxetine, Paroxetine Antihistamines, first generation (sedating): Clemastine, Chlorphenamine, Cyproheptadine, Diphenhydramine/-hydrinate, Hydroxyzine, Promethazine; also Cetirizine, Loratidine Antipsychotics: especially Clozapine, Fluphenazine, Haloperidol, Olanzepine, and phenothiazines e.g. Prochlorperazine, Trifluoperazine Baclofen Carbamazepine Disopyramide Loperamide Oxcarbazepine Pethidine -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Headache in Primary Care *
HeadacHe IN PRIMARY CARE * Dr Neil Whittaker - GP, Nelson Key Advisers: Dr Alistair Dunn - GP, Whangarei Dr Alan Wright - Neurologist, Dunedin Expert Reviewer: Every headache presentation is unique and challenging, requiring a flexible and individualised approach to headache management. - Most headaches are benign primary headaches - A few headaches are secondary to underlying pathology, which may be life threatening Primary headaches can be difficult to diagnose and manage. People, who experience severe or recurrent primary headache, can be subject to significant social, financial and disability burden. We cannot cover all the issues associated with headache presentation in primary care; instead, our focus is on assisting clinicians to: - Recognise presentations of secondary headaches - Effectively diagnose primary headaches - Manage primary headaches, in particular tension-type headache, migraine and cluster headache - Avoid, recognise and manage medication overuse headache 10 I BPJ I Issue 7 www.bpac.org.nz keyword: “Headache” DIAGNOSIS OF HEADACHE IN PRIMARY CARE The keys to headache diagnosis in primary care are: - Ensuring occasional presentations of secondary headache do not escape notice - Differentiating between the causes of primary headache - Addressing patient concerns about serious pathology RECOGNISE SERIOUS SECONDARY HEADACHES BY BEING ALERT FOR RED FLAGS AND PERFORMING FUNDOSCOPY Although primary care clinicians worry about Red Flags in headache presentation missing serious secondary headaches, most Red Flags in headache presentation include: people presenting with secondary headache will have alerting clinical features. These Age clinical features, red flags, are not highly - Over 50 years at onset of new headache specific but do alert clinicians to the need for - Under 10 years at onset particular care in the history, examination and Characteristics investigation. -

Deprescribing Anticholinergic and Sedative Medicines: Protocol for a Feasibility Trial (DEFEAT- Polypharmacy) in Residential Aged Care Facilities
Open Access Protocol BMJ Open: first published as 10.1136/bmjopen-2016-013800 on 16 April 2017. Downloaded from Deprescribing anticholinergic and sedative medicines: protocol for a Feasibility Trial (DEFEAT- polypharmacy) in residential aged care facilities Nagham Ailabouni,1 Dee Mangin,2 Prasad S Nishtala1 To cite: Ailabouni N, ABSTRACT Strengths and limitations of this study Mangin D, Nishtala PS. Introduction: Targeted deprescribing of Deprescribing anticholinergic anticholinergic and sedative medicines can lead to ▪ and sedative medicines: Using a quantitative measure (ie, the Drug Burden positive health outcomes in older people; as they have protocol for a Feasibility Trial Index) will help to determine the effect of depre- (DEFEAT-polypharmacy) in been associated with cognitive and physical scribing anticholinergic and sedative medicines. residential aged care facilities. functioning decline. This study will examine whether ▪ A pharmacist conducting in-depth medicine BMJ Open 2017;7:e013800. the proposed intervention is feasible at reducing the reviews could help to alleviate time constraints doi:10.1136/bmjopen-2016- prescription of anticholinergic and sedative medicines often faced by general practitioners in the resi- 013800 in older people. dential care setting. Methods and analysis: The Standard Protocol ▪ Six months may not be adequate to fully investi- ▸ Prepublication history and Items: Recommendations for Interventional trials gate the clinical effects of deprescribing. additional material is (SPIRIT checklist) was used to develop and report the available. To view please visit protocol. Single group (precomparison and the journal (http://dx.doi.org/ postcomparison) feasibility study design. 10.1136/bmjopen-2016- Study population: 3 residential care homes have INTRODUCTION 013800). been recruited. -
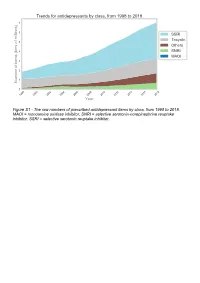
The Raw Numbers of Prescribed Antidepressant Items by Class, from 1998 to 2018
Figure S1 - The raw numbers of prescribed antidepressant items by class, from 1998 to 2018. MAOI = monoamine oxidase inhibitor, SNRI = selective serotonin-norepinephrine reuptake inhibitor, SSRI = selective serotonin reuptake inhibitor. Figure S2 - The raw numbers of prescribed antidepressant items for the ten most commonly prescribed antidepressants (in 2018), from 1998 to 2018. Figure S3 - Practice level percentile charts for the proportions of the ten most commonly prescribed antidepressants (in 2018), prescribed between August 2010 and November 2019. Deciles are in blue, with median shown as a heavy blue line, and extreme percentiles are in red. Figure S4 - Practice level percentile charts for the proportions of specific MAOIs prescribed between August 2010 and November 2019. Deciles are in blue, with median shown as a heavy blue line, and extreme percentiles are in red. Figure S5 - CCG level heat map for the percentage proportions of MAOIs prescribed between December 2018 and November 2019. MAOI = monoamine oxidase inhibitor. Figure S6 - CCG level heat maps for the percentage proportions of paroxetine, dosulepin, and trimipramine prescribed between December 2018 and November 2019. Table S1 - Antidepressant drugs, by category. MAOI = monoamine oxidase inhibitor, SNRI = selective serotonin-norepinephrine reuptake inhibitor, SSRI = selective serotonin reuptake inhibitor. Class Drug MAOI Isocarboxazid, moclobemide, phenelzine, tranylcypromine SNRI Duloxetine, venlafaxine SSRI Citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, -
Preventive Report Appendix
Title Authors Published Journal Volume Issue Pages DOI Final Status Exclusion Reason Nasal sumatriptan is effective in treatment of migraine attacks in children: A Ahonen K.; Hamalainen ML.; Rantala H.; 2004 Neurology 62 6 883-7 10.1212/01.wnl.0000115105.05966.a7 Deemed irrelevant in initial screening Seasonal variation in migraine. Alstadhaug KB.; Salvesen R.; Bekkelund SI. Cephalalgia : an 2005 international journal 25 10 811-6 10.1111/j.1468-2982.2005.01018.x Deemed irrelevant in initial screening Flunarizine, a calcium channel blocker: a new prophylactic drug in migraine. Amery WK. 1983 Headache 23 2 70-4 10.1111/j.1526-4610.1983.hed2302070 Deemed irrelevant in initial screening Monoamine oxidase inhibitors in the control of migraine. Anthony M.; Lance JW. Proceedings of the 1970 Australian 7 45-7 Deemed irrelevant in initial screening Prostaglandins and prostaglandin receptor antagonism in migraine. Antonova M. 2013 Danish medical 60 5 B4635 Deemed irrelevant in initial screening Divalproex extended-release in adolescent migraine prophylaxis: results of a Apostol G.; Cady RK.; Laforet GA.; Robieson randomized, double-blind, placebo-controlled study. WZ.; Olson E.; Abi-Saab WM.; Saltarelli M. 2008 Headache 48 7 1012-25 10.1111/j.1526-4610.2008.01081.x Deemed irrelevant in initial screening Divalproex sodium extended-release for the prophylaxis of migraine headache in Apostol G.; Lewis DW.; Laforet GA.; adolescents: results of a stand-alone, long-term open-label safety study. Robieson WZ.; Fugate JM.; Abi-Saab WM.; 2009 Headache 49 1 45-53 10.1111/j.1526-4610.2008.01279.x Deemed irrelevant in initial screening Safety and tolerability of divalproex sodium extended-release in the prophylaxis of Apostol G.; Pakalnis A.; Laforet GA.; migraine headaches: results of an open-label extension trial in adolescents. -

Fatal Toxicity of Antidepressant Drugs in Overdose
BRITISH MEDICAL JOURNAL VOLUME 295 24 OCTOBER 1987 1021 Br Med J (Clin Res Ed): first published as 10.1136/bmj.295.6605.1021 on 24 October 1987. Downloaded from PAPERS AND SHORT REPORTS Fatal toxicity of antidepressant drugs in overdose SIMON CASSIDY, JOHN HENRY Abstract dangerous in overdose, thus meriting investigation of their toxic properties and closer consideration of the circumstances in which A fatal toxicity index (deaths per million National Health Service they are prescribed. Recommendations may thus be made that prescriptions) was calculated for antidepressant drugs on sale might reduce the number offatalities. during the years 1975-84 in England, Wales, and Scotland. The We used national mortality statistics and prescription data tricyclic drugs introduced before 1970 had a higher index than the to compile fatal toxicity indices for the currently available anti- mean for all the drugs studied (p<0-001). In this group the depressant drugs to assess the comparative safety of the different toxicity ofamitriptyline, dibenzepin, desipramine, and dothiepin antidepressant drugs from an epidemiological standpoint. Owing to was significantly higher, while that ofclomipramine, imipramine, the nature of the disease these drugs are particularly likely to be iprindole, protriptyline, and trimipramine was lower. The mono- taken in overdose and often cause death. amine oxidase inhibitors had intermediate toxicity, and the antidepressants introduced since 1973, considered as a group, had significantly lower toxicity than the mean (p<0-001). Ofthese newer drugs, maprotiline had a fatal toxicity index similar to that Sources ofinformation and methods of the older tricyclic antidepressants, while the other newly The statistical sources used list drugs under their generic and proprietary http://www.bmj.com/ introduced drugs had lower toxicity indices, with those for names. -

A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache
University of South Florida Masthead Logo Scholar Commons School of Information Faculty Publications School of Information 7-2015 A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache Authors: Jeffrey L. Jackson, Elizabeth Cogbill, Rafael Santana-Davila, Christina Eldredge, William Collier, Andrew Gradall, Neha Sehgal, and Jessica Kuester OBJECTIVE: To compare the effectiveness and side effects of migraine prophylactic medications. DESIGN: We performed a network meta-analysis. Data were extracted independently in duplicate and quality was assessed using both the JADAD and Cochrane Risk of Bias instruments. Data were pooled and network meta-analysis performed using random effects models. DATA SOURCES: PUBMED, EMBASE, Cochrane Trial Registry, bibliography of retrieved articles through 18 May 2014. ELIGIBILITY CRITERIA FOR SELECTING STUDIES: We included randomized controlled trials of adults with migraine headaches of at least 4 weeks in duration. RESULTS: Placebo controlled trials included alpha blockers (n = 9), angiotensin converting enzyme inhibitors (n = 3), angiotensin receptor blockers (n = 3), anticonvulsants (n = 32), beta-blockers (n = 39), calcium channel blockers (n = 12), flunarizine (n = 7), serotonin reuptake inhibitors (n = 6), serotonin norepinephrine reuptake inhibitors (n = 1) serotonin agonists (n = 9) and tricyclic antidepressants (n = 11). In addition there were 53 trials comparing different drugs. Drugs with at least 3 trials that were more effective than placebo for episodic migraines -

Zebrafish Embryo Screen Identifies Anti-Metastasis Drugs
bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.434001; this version posted March 5, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Zebrafish embryo screen identifies anti-metastasis drugs 2 3 Joji Nakayama1,2,3,4§, Lora Tan1, Boon Cher Goh2, Shu Wang1, 5, Hideki Makinoshima3,6 and 4 Zhiyuan Gong1§ 5 6 1Department of Biological Science, National University of Singapore, Singapore 7 2Cancer Science Institute of Singapore, National University of Singapore, Singapore 8 3Tsuruoka Metabolomics Laboratory, National Cancer Center, Tsuruoka, Japan 9 4Shonai Regional Industry Promotion Center, Tsuruoka, Japan. 10 5Institute of Bioengineering and Nanotechnology, Singapore 11 6Division of Translational Research, Exploratory Oncology Research and Clinical Trial 12 Center, National Cancer Center, Kashiwa, Japan. 13 14 Keywords: Zebrafish, metastasis, gastrulation, phenotyping screening 15 16 §Corresponding authors: 17 Joji Nakayama 18 Tsuruoka Metabolomics Laboratory, National Cancer Center, Mizukami 246-2, Kakuganji, 19 Tsuruoka, Yamagata, Japan 975-0052. 20 email: [email protected] 21 22 Zhiyuan Gong 23 Department of Biological Science, National University of Singapore, Singapore 117543. 24 email: [email protected] 25 26 The authors disclose no potential conflicts of interest. 27 Total words excluding abstract, material and methods, references, and figure legends: 1390 28 Number of figures: 2 29 Number of supplementary figures: 3 30 Number of supplementary tables: 3 31 bioRxiv preprint doi: https://doi.org/10.1101/2021.03.04.434001; this version posted March 5, 2021. -

Association of Selective Serotonin Reuptake Inhibitors with the Risk for Spontaneous Intracranial Hemorrhage
Supplementary Online Content Renoux C, Vahey S, Dell’Aniello S, Boivin J-F. Association of selective serotonin reuptake inhibitors with the risk for spontaneous intracranial hemorrhage. JAMA Neurol. Published online December 5, 2016. doi:10.1001/jamaneurol.2016.4529 eMethods 1. List of Antidepressants for Cohort Entry eMethods 2. List of Antidepressants According to the Degree of Serotonin Reuptake Inhibition eMethods 3. Potential Confounding Variables Included in Multivariate Models eMethods 4. Sensitivity Analyses eFigure. Flowchart of Incident Antidepressant (AD) Cohort Definition and Case- Control Selection eTable 1. Crude and Adjusted Rate Ratios of Intracerebral Hemorrhage Associated With Current Use of SSRIs Relative to TCAs eTable 2. Crude and Adjusted Rate Ratios of Subarachnoid Hemorrhage Associated With Current Use of SSRIs Relative to TCAs eTable 3. Crude and Adjusted Rate Ratios of Intracranial Extracerebral Hemorrhage Associated With Current Use of SSRIs Relative to TCAs. eTable 4. Crude and Adjusted Rate Ratios of Intracerebral Hemorrhage Associated With Current Use of Antidepressants With Strong Degree of Inhibition of Serotonin Reuptake Relative to Weak eTable 5. Crude and Adjusted Rate Ratios of Subarachnoid Hemorrhage Associated With Current Use of Antidepressants With Strong Degree of Inhibition of Serotonin Reuptake Relative to Weak eTable 6. Crude and Adjusted Rate Ratios of Intracranial Extracerebral Hemorrhage Associated With Current Use of Antidepressants With Strong Degree of Inhibition of Serotonin Reuptake Relative to Weak This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. Downloaded From: https://jamanetwork.com/ on 10/02/2021 eMethods 1. -

Headache Management: Pharmacological Approaches
REVIEW Headache management: Pract Neurol: first published as 10.1136/practneurol-2015-001167 on 3 July 2015. Downloaded from pharmacological approaches Alex J Sinclair,1,2 Aaron Sturrock,2 Brendan Davies,3 Manjit Matharu4 ▸ Additional material is ABSTRACT be very rewarding for the clinician. The published online only. To view Headache is one of the most common conditions purpose of this article, the first of two please visit the journal online (http://dx.doi.org/10.1136/ presenting to the neurology clinic, yet a linked articles, is to provide an up-to-date practneurol-2015-001167). significant proportion of these patients are overview of the pharmacological manage- unsatisfied by their clinic experience. Headache ment of common headache disorders 1Department of Neurobiology, School of Clinical and can be extremely disabling; effective treatment is (as well as a limited number of non- Experimental Medicine, College not only essential for patients but is rewarding pharmaceutical strategies). of Medical and Dental Sciences, for the physician. In this first of two parts review The University of Birmingham, of headache, we provide an overview of Birmingham, UK THE COMMON PRIMARY HEADACHE 2Neurology Department, headache management, emerging therapeutic DISORDERS University Hospitals Birmingham strategies and an accessible interpretation of In European populations, the annual sex- NHS Trust, Queen Elizabeth clinical guidelines to assist the busy neurologist. Hospital Birmingham, adjusted prevalence for tension-type Birmingham, UK headache is 35%, for migraine is 38%, 3 Department of Neurology, Royal BACKGROUND but for cluster headache is only Stoke University Hospital, ’ 0.15%.45These three together comprise Stoke-on-Trent, UK Headache is listed among the WHO s 4Headache Group, Institute of major causes of disability with a global the most prevalent primary headache dis- Neurology, London, UK prevalence of 47% (symptoms occurring orders. -

New Zealand Data Sheet
1 PARNATE tranylcypromine film-coated tablets 10 mg New Zealand Data Sheet 1 PARNATE® (10 MG FILM-COATED TABLETS) PARNATE 10 mg film-coated tablets. 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Parnate 10 mg film-coated tablets: each tablet contains tranylcypromine sulfate equivalent to 10 mg of tranylcypromine. Excipients with known effect: each tablet contains sucrose 6 mg. For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Parnate 10 mg film-coated tablets contain "geranium rose" coloured, biconvex, film-coated tablets. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Parnate is indicated for the treatment of symptoms of depressive illness especially where treatment with other types of anti-depressants has failed. It is not recommended for use in mild depressive states resulting from temporary situational difficulties. 4.2 Dose and method of administration Adults Begin with 20 mg a day given as 10 mg in the morning and 10 mg in the afternoon. If there is no satisfactory response after two weeks, add one more tablet at midday. Continue this dosage for at least a week. A dosage of 3 tablets a day should only be exceeded with caution. When a satisfactory response is established, dosage may be reduced to a maintenance level. Some patients will be maintained on 20 mg per day, some will need only 10 mg daily. If no improvement occurs, continued administration is unlikely to be beneficial. 1 2 PARNATE tranylcypromine film-coated tablets 10 mg When given together with a tranquilliser, the dosage of Parnate is not affected. When the medicine is given concurrently with electroconvulsive therapy, the recommended dosage is 10 mg twice a day during the series and 10 mg a day afterwards as maintenance therapy.