Headache Management: Pharmacological Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(12) Patent Application Publication (10) Pub. No.: US 2014/0100249 A1 Sears Et Al
US 201401.00249A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2014/0100249 A1 Sears et al. (43) Pub. Date: Apr. 10, 2014 (54) THERAPEUTIC TREATMENT A63/37 (2006.01) A613 L/45 (2006.01) (71) Applicants: Douglas Sears, Oak Park, CA (US); A613 L/4458 (2006.01) Michael Reilly, Oak Park, CA (US) (52) U.S. Cl. CPC ............... A61K 45/06 (2013.01); A61 K3I/451 (72) Inventors: Douglas Sears, Oak Park, CA (US); (2013.01): A613 L/4458 (2013.01); A61 K Michael Reilly, Oak Park, CA (US) 3 1/137 (2013.01); A61 K31/165 (2013.01) USPC .......................................................... S14/325 (21) Appl. No.: 14/046,528 (57) ABSTRACT (22) Filed: Oct. 4, 2013 This invention discloses a treatment for a patient receiving O O medication to treat an attention deficit disorder Such as Related U.S. Application Data ADHD wherein the treatment results in a loss of appetite and (60) Provisional application No. 61/744,948, filed on Oct. impairment of the patient's attentiveness. The treatment com 9, 2012, now abandoned. bines a treatment for an attention deficit disorder with an appetite stimulant, wherein the appetite stimulant increases Publication Classification the caloric intake of a patient, which can increase the patients attentiveness. The combination treatment can be given for an (51) Int. Cl. indefinite, including, without limitation, life-long, to allow a A6 IK 45/06 (2006.01) patient to maintain normal caloric intake during treatment for A6 IK3I/65 (2006.01) an attention deficit disorder. 8aasaias: Patent Application Publication Apr. 10, 2014 Sheet 1 of 22 US 2014/010O249 A1 Figure i: improvement in Atiention with increased Caiotic intake 8aakast Patent Application Publication Apr. -
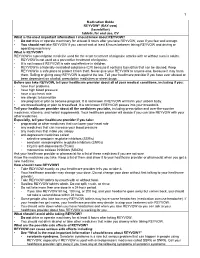
Medication Guide
1 Medication Guide REYVOW® (RAY-vow) (lasmiditan) tablets, for oral use, CV What is the most important information I should know about REYVOW? • Do not drive or operate machinery for at least 8 hours after you take REYVOW, even if you feel well enough. • You should not take REYVOW if you cannot wait at least 8 hours between taking REYVOW and driving or operating machinery. What is REYVOW? REYVOW is a prescription medicine used for the acute treatment of migraine attacks with or without aura in adults. • REYVOW is not used as a preventive treatment of migraine. • It is not known if REYVOW is safe and effective in children. • REYVOW is a federally controlled substance (CV) because it contains lasmiditan that can be abused. Keep REYVOW in a safe place to protect it from theft. Never give your REYVOW to anyone else, because it may harm them. Selling or giving away REYVOW is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs. Before you take REYVOW, tell your healthcare provider about all of your medical conditions, including if you: • have liver problems • have high blood pressure • have a low heart rate • are allergic to lasmiditan • are pregnant or plan to become pregnant. It is not known if REYVOW will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if REYVOW passes into your breastmilk. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. -

Appendix A: Potentially Inappropriate Prescriptions (Pips) for Older People (Modified from ‘STOPP/START 2’ O’Mahony Et Al 2014)
Appendix A: Potentially Inappropriate Prescriptions (PIPs) for older people (modified from ‘STOPP/START 2’ O’Mahony et al 2014) Consider holding (or deprescribing - consult with patient): 1. Any drug prescribed without an evidence-based clinical indication 2. Any drug prescribed beyond the recommended duration, where well-defined 3. Any duplicate drug class (optimise monotherapy) Avoid hazardous combinations e.g.: 1. The Triple Whammy: NSAID + ACE/ARB + diuretic in all ≥ 65 year olds (NHS Scotland 2015) 2. Sick Day Rules drugs: Metformin or ACEi/ARB or a diuretic or NSAID in ≥ 65 year olds presenting with dehydration and/or acute kidney injury (AKI) (NHS Scotland 2015) 3. Anticholinergic Burden (ACB): Any additional medicine with anticholinergic properties when already on an Anticholinergic/antimuscarinic (listed overleaf) in > 65 year olds (risk of falls, increased anticholinergic toxicity: confusion, agitation, acute glaucoma, urinary retention, constipation). The following are known to contribute to the ACB: Amantadine Antidepressants, tricyclic: Amitriptyline, Clomipramine, Dosulepin, Doxepin, Imipramine, Nortriptyline, Trimipramine and SSRIs: Fluoxetine, Paroxetine Antihistamines, first generation (sedating): Clemastine, Chlorphenamine, Cyproheptadine, Diphenhydramine/-hydrinate, Hydroxyzine, Promethazine; also Cetirizine, Loratidine Antipsychotics: especially Clozapine, Fluphenazine, Haloperidol, Olanzepine, and phenothiazines e.g. Prochlorperazine, Trifluoperazine Baclofen Carbamazepine Disopyramide Loperamide Oxcarbazepine Pethidine -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Headache in Primary Care *
HeadacHe IN PRIMARY CARE * Dr Neil Whittaker - GP, Nelson Key Advisers: Dr Alistair Dunn - GP, Whangarei Dr Alan Wright - Neurologist, Dunedin Expert Reviewer: Every headache presentation is unique and challenging, requiring a flexible and individualised approach to headache management. - Most headaches are benign primary headaches - A few headaches are secondary to underlying pathology, which may be life threatening Primary headaches can be difficult to diagnose and manage. People, who experience severe or recurrent primary headache, can be subject to significant social, financial and disability burden. We cannot cover all the issues associated with headache presentation in primary care; instead, our focus is on assisting clinicians to: - Recognise presentations of secondary headaches - Effectively diagnose primary headaches - Manage primary headaches, in particular tension-type headache, migraine and cluster headache - Avoid, recognise and manage medication overuse headache 10 I BPJ I Issue 7 www.bpac.org.nz keyword: “Headache” DIAGNOSIS OF HEADACHE IN PRIMARY CARE The keys to headache diagnosis in primary care are: - Ensuring occasional presentations of secondary headache do not escape notice - Differentiating between the causes of primary headache - Addressing patient concerns about serious pathology RECOGNISE SERIOUS SECONDARY HEADACHES BY BEING ALERT FOR RED FLAGS AND PERFORMING FUNDOSCOPY Although primary care clinicians worry about Red Flags in headache presentation missing serious secondary headaches, most Red Flags in headache presentation include: people presenting with secondary headache will have alerting clinical features. These Age clinical features, red flags, are not highly - Over 50 years at onset of new headache specific but do alert clinicians to the need for - Under 10 years at onset particular care in the history, examination and Characteristics investigation. -

Deprescribing Anticholinergic and Sedative Medicines: Protocol for a Feasibility Trial (DEFEAT- Polypharmacy) in Residential Aged Care Facilities
Open Access Protocol BMJ Open: first published as 10.1136/bmjopen-2016-013800 on 16 April 2017. Downloaded from Deprescribing anticholinergic and sedative medicines: protocol for a Feasibility Trial (DEFEAT- polypharmacy) in residential aged care facilities Nagham Ailabouni,1 Dee Mangin,2 Prasad S Nishtala1 To cite: Ailabouni N, ABSTRACT Strengths and limitations of this study Mangin D, Nishtala PS. Introduction: Targeted deprescribing of Deprescribing anticholinergic anticholinergic and sedative medicines can lead to ▪ and sedative medicines: Using a quantitative measure (ie, the Drug Burden positive health outcomes in older people; as they have protocol for a Feasibility Trial Index) will help to determine the effect of depre- (DEFEAT-polypharmacy) in been associated with cognitive and physical scribing anticholinergic and sedative medicines. residential aged care facilities. functioning decline. This study will examine whether ▪ A pharmacist conducting in-depth medicine BMJ Open 2017;7:e013800. the proposed intervention is feasible at reducing the reviews could help to alleviate time constraints doi:10.1136/bmjopen-2016- prescription of anticholinergic and sedative medicines often faced by general practitioners in the resi- 013800 in older people. dential care setting. Methods and analysis: The Standard Protocol ▪ Six months may not be adequate to fully investi- ▸ Prepublication history and Items: Recommendations for Interventional trials gate the clinical effects of deprescribing. additional material is (SPIRIT checklist) was used to develop and report the available. To view please visit protocol. Single group (precomparison and the journal (http://dx.doi.org/ postcomparison) feasibility study design. 10.1136/bmjopen-2016- Study population: 3 residential care homes have INTRODUCTION 013800). been recruited. -

Lasmiditan Is an Effective Acute Treatment for Migraine: a Phase 3 Randomized Study Bernice Kuca, Stephen D
ARTICLE OPEN ACCESS CLASS OF EVIDENCE Lasmiditan is an effective acute treatment for migraine A phase 3 randomized study Bernice Kuca, BA, MS, Stephen D. Silberstein, MD, Linda Wietecha, BSN, MS, Paul H. Berg, MS, Correspondence Gregory Dozier, MPH, and Richard B. Lipton, MD, on behalf of the COL MIG-301 Study Group Ms. Wietecha [email protected] Neurology® 2018;91:e2222-e2232. doi:10.1212/WNL.0000000000006641 Abstract RELATED ARTICLE Objective Article To assess the efficacy and safety of lasmiditan in the acute treatment of migraine. Galcanezumab in chronic migraine: The randomized, Methods double-blind, placebo- Adult patients with migraine were randomized (1:1:1) to a double-blind dose of oral lasmiditan controlled REGAIN study 200 mg, lasmiditan 100 mg, or placebo and were asked to treat their next migraine attack within Page 1082 4 hours of onset. Over 48 hours after dosing, patients used an electronic diary to record headache pain and the presence of nausea, phonophobia, and photophobia, one of which was MORE ONLINE designated their most bothersome symptom (MBS). Class of Evidence Criteria for rating Results ≥ therapeutic and diagnostic Of the 1,856 patients who treated an attack, 77.9% had 1 cardiovascular risk factors in addition studies to migraine. Compared with placebo, more patients dosed with lasmiditan 200 mg were free of NPub.org/coe headache pain at 2 hours after dosing (32.2% vs 15.3%; odds ratio [OR] 2.6, 95% confidence interval [CI] 2.0–3.6, p< 0.001), similar to those dosed with lasmiditan 100 mg (28.2%; OR 2.2, 95% CI 1.6–3.0, p< 0.001). -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Preventive Report Appendix
Title Authors Published Journal Volume Issue Pages DOI Final Status Exclusion Reason Nasal sumatriptan is effective in treatment of migraine attacks in children: A Ahonen K.; Hamalainen ML.; Rantala H.; 2004 Neurology 62 6 883-7 10.1212/01.wnl.0000115105.05966.a7 Deemed irrelevant in initial screening Seasonal variation in migraine. Alstadhaug KB.; Salvesen R.; Bekkelund SI. Cephalalgia : an 2005 international journal 25 10 811-6 10.1111/j.1468-2982.2005.01018.x Deemed irrelevant in initial screening Flunarizine, a calcium channel blocker: a new prophylactic drug in migraine. Amery WK. 1983 Headache 23 2 70-4 10.1111/j.1526-4610.1983.hed2302070 Deemed irrelevant in initial screening Monoamine oxidase inhibitors in the control of migraine. Anthony M.; Lance JW. Proceedings of the 1970 Australian 7 45-7 Deemed irrelevant in initial screening Prostaglandins and prostaglandin receptor antagonism in migraine. Antonova M. 2013 Danish medical 60 5 B4635 Deemed irrelevant in initial screening Divalproex extended-release in adolescent migraine prophylaxis: results of a Apostol G.; Cady RK.; Laforet GA.; Robieson randomized, double-blind, placebo-controlled study. WZ.; Olson E.; Abi-Saab WM.; Saltarelli M. 2008 Headache 48 7 1012-25 10.1111/j.1526-4610.2008.01081.x Deemed irrelevant in initial screening Divalproex sodium extended-release for the prophylaxis of migraine headache in Apostol G.; Lewis DW.; Laforet GA.; adolescents: results of a stand-alone, long-term open-label safety study. Robieson WZ.; Fugate JM.; Abi-Saab WM.; 2009 Headache 49 1 45-53 10.1111/j.1526-4610.2008.01279.x Deemed irrelevant in initial screening Safety and tolerability of divalproex sodium extended-release in the prophylaxis of Apostol G.; Pakalnis A.; Laforet GA.; migraine headaches: results of an open-label extension trial in adolescents. -

Acute Migraine Treatment
Acute Migraine Treatment Morris Levin, MD Professor of Neurology Director, Headache Center UCSF Department of Neurology San Francisco, CA Mo Levin Disclosures Consulting Royalties Allergan Oxford University Press Supernus Anadem Press Amgen Castle Connolly Med. Publishing Lilly Wiley Blackwell Mo Levin Disclosures Off label uses of medication DHE Antiemetics Zolmitriptan Learning Objectives At the end of the program attendees will be able to 1. List all important options in the acute treatment of migraine 2. Discuss the evidence and guidelines supporting the major migraine acute treatment options 3. Describe potential adverse effects and medication- medication interactions in acute migraine pharmacological treatment Case 27 y/o woman has suffered ever since she can remember from “sick headaches” . Pain is frontal, increases over time and is generally accompanied by nausea and vomiting. She feels depressed. The headache lasts the rest of the day but after sleeping through the night she awakens asymptomatic 1. Diagnosis 2. Severe Headache relief Diagnosis: What do we need to beware of? • Misdiagnosis of primary headache • Secondary causes of headache Red Flags in HA New (recent onset or change in pattern) Effort or Positional Later onset than usual (middle age or later) Meningismus, Febrile AIDS, Cancer or other known Systemic illness - Neurological or psych symptoms or signs Basic principles of Acute Therapy of Headaches • Diagnose properly, including comorbid conditions • Stratify therapy rather than treat in steps • Treat early -

A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache
University of South Florida Masthead Logo Scholar Commons School of Information Faculty Publications School of Information 7-2015 A Comparative Effectiveness Meta-Analysis of Drugs for the Prophylaxis of Migraine Headache Authors: Jeffrey L. Jackson, Elizabeth Cogbill, Rafael Santana-Davila, Christina Eldredge, William Collier, Andrew Gradall, Neha Sehgal, and Jessica Kuester OBJECTIVE: To compare the effectiveness and side effects of migraine prophylactic medications. DESIGN: We performed a network meta-analysis. Data were extracted independently in duplicate and quality was assessed using both the JADAD and Cochrane Risk of Bias instruments. Data were pooled and network meta-analysis performed using random effects models. DATA SOURCES: PUBMED, EMBASE, Cochrane Trial Registry, bibliography of retrieved articles through 18 May 2014. ELIGIBILITY CRITERIA FOR SELECTING STUDIES: We included randomized controlled trials of adults with migraine headaches of at least 4 weeks in duration. RESULTS: Placebo controlled trials included alpha blockers (n = 9), angiotensin converting enzyme inhibitors (n = 3), angiotensin receptor blockers (n = 3), anticonvulsants (n = 32), beta-blockers (n = 39), calcium channel blockers (n = 12), flunarizine (n = 7), serotonin reuptake inhibitors (n = 6), serotonin norepinephrine reuptake inhibitors (n = 1) serotonin agonists (n = 9) and tricyclic antidepressants (n = 11). In addition there were 53 trials comparing different drugs. Drugs with at least 3 trials that were more effective than placebo for episodic migraines