Acute Migraine Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Medication Guide
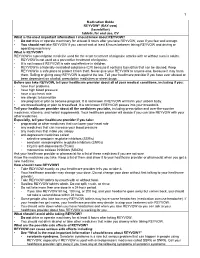
1 Medication Guide REYVOW® (RAY-vow) (lasmiditan) tablets, for oral use, CV What is the most important information I should know about REYVOW? • Do not drive or operate machinery for at least 8 hours after you take REYVOW, even if you feel well enough. • You should not take REYVOW if you cannot wait at least 8 hours between taking REYVOW and driving or operating machinery. What is REYVOW? REYVOW is a prescription medicine used for the acute treatment of migraine attacks with or without aura in adults. • REYVOW is not used as a preventive treatment of migraine. • It is not known if REYVOW is safe and effective in children. • REYVOW is a federally controlled substance (CV) because it contains lasmiditan that can be abused. Keep REYVOW in a safe place to protect it from theft. Never give your REYVOW to anyone else, because it may harm them. Selling or giving away REYVOW is against the law. Tell your healthcare provider if you have ever abused or been dependent on alcohol, prescription medicines or street drugs. Before you take REYVOW, tell your healthcare provider about all of your medical conditions, including if you: • have liver problems • have high blood pressure • have a low heart rate • are allergic to lasmiditan • are pregnant or plan to become pregnant. It is not known if REYVOW will harm your unborn baby. • are breastfeeding or plan to breastfeed. It is not known if REYVOW passes into your breastmilk. Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. -

What Are the Acute Treatments for Migraine and How Are They Used?
2. Acute Treatment CQ II-2-1 What are the acute treatments for migraine and how are they used? Recommendation The mainstay of acute treatment for migraine is pharmacotherapy. The drugs used include (1) acetaminophen, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans and (5) antiemetics. Stratified treatment according to the severity of migraine is recommended: use NSAIDs such as aspirin and naproxen for mild to moderate headache, and use triptans for moderate to severe headache, or even mild to moderate headache when NSAIDs were ineffective in the past. It is necessary to give guidance and cautions to patients having acute attacks, and explain the methods of using medications (timing, dose, frequency of use) and medication use during pregnancy and breast-feeding. Grade A Background and Objective The objective of acute treatment is to resolve the migraine attack completely and rapidly and restore the patient’s normal functions. An ideal treatment should have the following characteristics: (1) resolves pain and associated symptoms rapidly; (2) is consistently effective; (3) no recurrence; (4) no need for additional use of medication; (5) no adverse effects; (6) can be administered by the patients themselves; and (7) low cost. Literature was searched to identify acute treatments that satisfy the above conditions. Comments and Evidence The acute treatment drugs for migraine generally include (1) acetaminophens, (2) non-steroidal anti-inflammatory drugs (NSAIDs), (3) ergotamines, (4) triptans, and (5) antiemetics. For severe migraines including status migrainosus and migraine attacks refractory to treatment, (6) anesthetics, and (7) corticosteroids (dexamethasone) are used (Tables 1 and 2).1)-9) There are two approaches to the selection and sequencing of these medications: “step care” and “stratified care”. -

Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin Healthcare
Benzodiazepines: Uses and Risks Charlie Reznikoff, MD Hennepin healthcare 4/22/2020 Overview benzodiazepines • Examples of benzos and benzo like drugs • Indications for benzos • Pharmacology of benzos • Side effects and contraindications • Benzo withdrawal • Benzo tapers 12/06/2018 Sedative/Hypnotics • Benzodiazepines • Alcohol • Z-drugs (Benzo-like sleeping aids) • Barbiturates • GHB • Propofol • Some inhalants • Gabapentin? Pregabalin? 12/06/2018 Examples of benzodiazepines • Midazolam (Versed) • Triazolam (Halcion) • Alprazolam (Xanax) • Lorazepam (Ativan) • Temazepam (Restoril) • Oxazepam (Serax) • Clonazepam (Klonopin) • Diazepam (Valium) • Chlordiazepoxide (Librium) 4/22/2020 Sedatives: gaba stimulating drugs have incomplete “cross tolerance” 12/06/2018 Effects from sedative (Benzo) use • Euphoria/bliss • Suppresses seizures • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Sleep inducing • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 Tolerance to benzo effects? • Effects quickly diminish with repeated use (weeks) • Euphoria/bliss • Suppresses seizures • Effects incompletely diminish with repeated use • Amnesia • Muscle relaxation • Clumsiness, visio-spatial impairment • Seep inducing • Durable effects with repeated use • Respiratory suppression • Anxiolysis/disinhibition 12/06/2018 If you understand this pharmacology you can figure out the rest... • Potency • 1 mg diazepam <<< 1 mg alprazolam • Duration of action • Half life differences • Onset of action • Euphoria, clinical utility in acute -

ERJ-01090-2018.Supplement
Shaheen et al Online data supplement Prescribed analgesics in pregnancy and risk of childhood asthma Seif O Shaheen, Cecilia Lundholm, Bronwyn K Brew, Catarina Almqvist. 1 Shaheen et al Figure E1: Data available for analysis Footnote: Numbers refer to adjusted analyses (complete data on covariates) 2 Shaheen et al Table E1. Three classes of analgesics included in the analyses ATC codes Generic drug name Opioids N02AA59 Codeine, combinations excluding psycholeptics N02AA79 Codeine, combinations with psycholeptics N02AA08 Dihydrocodeine N02AA58 Dihydrocodeine, combinations N02AC04 Dextropropoxyphene N02AC54 Dextropropoxyphene, combinations excluding psycholeptics N02AX02 Tramadol Anti-migraine N02CA01 Dihydroergotamine N02CA02 Ergotamine N02CA04 Methysergide N02CA07 Lisuride N02CA51 Dihydroergotamine, combinations N02CA52 Ergotamine, combinations excluding psycholeptics N02CA72 Ergotamine, combinations with psycholeptics N02CC01 Sumatriptan N02CC02 Naratriptan N02CC03 Zolmitriptan N02CC04 Rizatriptan N02CC05 Almotriptan N02CC06 Eletriptan N02CC07 Frovatriptan N02CX01 Pizotifen N02CX02 Clonidine N02CX03 Iprazochrome N02CX05 Dimetotiazine N02CX06 Oxetorone N02CB01 Flumedroxone Paracetamol N02BE01 Paracetamol N02BE51 Paracetamol, combinations excluding psycholeptics N02BE71 Paracetamol, combinations with psycholeptics 3 Shaheen et al Table E2. Frequency of analgesic classes prescribed to the mother during pregnancy Opioids Anti- Paracetamol N % migraine No No No 459,690 93.2 No No Yes 9,091 1.8 Yes No No 15,405 3.1 No Yes No 2,343 0.5 Yes No -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

Menstrually Related and Nonmenstrual Migraines in A
MENSTRUALLY RELATED AND NONMENSTRUAL MIGRAINES IN A FREQUENT MIGRAINE POPULATION: FEATURES, CORRELATES, AND ACUTE TREATMENT DIFFERENCES A dissertation presented to the faculty of the College of Arts and Sciences of Ohio University In partial fulfillment of the requirements for the degree Doctor of Philosophy Brenda F. Pinkerman March 2006 This dissertation entitled MENSTRUALLY RELATED AND NONMENSTRUAL MIGRAINES IN A FREQUENT MIGRAINE POPULATION: FEATURES, CORRELATES, AND ACUTE TREATMENT DIFFERENCES by BRENDA F. PINKERMAN has been approved for the Department of Psychology and the College of Arts and Sciences by Kenneth A. Holroyd Distinguished Professor of Psychology Benjamin M. Ogles Interim Dean, College of Arts and Sciences PINKERMAN, BRENDA F. Ph.D. March 2006. Clinical Psychology Menstrually Related and Nonmenstrual Migraines in a Frequent Migraine Population: Features, Correlates, and Acute Treatment Differences (307 pp.) Director of Dissertation: Kenneth A. Holroyd This research describes and compares menstrually related migraines as defined by recent proposed guidelines of the International Headache Society (IHS, 2004) to nonmenstrual migraines in a population of female migraineurs with frequent, disabling migraines. Migraines are compared by frequency per day of the menstrual cycle, headache features, use of abortive and rescue medications, and acute migraine treatment outcomes. In addition, this study explores predictors of acute treatment response and headache recurrence within 24 hours following acute migraine treatment for menstrually related migraines. Participants are 107 menstruating female migaineurs who met IHS (2004) proposed criteria for menstrually related migraines and completed headache diaries using hand-held computers. Diary data are analyzed using repeated measures logistic regression. The frequency of migraines is significantly increased during the perimenstrual period, and menstrually related migraines are of longer duration and greater frequency with longer lasting disability than nonmenstrual migraines. -

Medications and Alcohol Craving
Medications and Alcohol Craving Robert M. Swift, M.D., Ph.D. The use of medications as an adjunct to alcoholism treatment is based on the premise that craving and other manifestations of alcoholism are mediated by neurobiological mechanisms. Three of the four medications approved in the United States or Europe for treating alcoholism are reported to reduce craving; these include naltrexone (ReVia™), acamprosate, and tiapride. The remaining medication, disulfiram (Antabuse®), may also possess some anticraving activity. Additional medications that have been investigated include ritanserin, which has not been shown to decrease craving or drinking levels in humans, and ondansetron, which shows promise for treating early onset alcoholics, who generally respond poorly to psychosocial treatment alone. Use of anticraving medications in combination (e.g., naltrexone plus acamprosate) may enhance their effectiveness. Future studies should address such issues as optimal dosing regimens and the development of strategies to enhance patient compliance. KEY WORDS: AOD (alcohol and other drug) craving; anti alcohol craving agents; alcohol withdrawal agents; drug therapy; neurobiological theory; alcohol cue; disulfiram; naltrexone; calcium acetylhomotaurinate; dopamine; serotonin uptake inhibitors; buspirone; treatment outcome; reinforcement; neurotransmitters; patient assessment; literature review riteria for defining alcoholism Results of craving research are often tions (i.e., pharmacotherapy) to improve vary widely. Most definitions difficult to interpret, -

Use of Analgesics in Exotic Felids Edward C. Ramsay, DVM Professor, Department of Small Animal Clinical Sciences, University Of
Use of Analgesics in Exotic Felids Formatted: Centered Edward C. Ramsay, DVM Professor, Department of Small Animal Clinical Sciences, University of Tennessee, and Consulting Veterinarian, Knoxville Zoological Gardens, Knoxville, Tennessee. Corresponding address: Ed Ramsay Dept. of Sm Animal Clin Sci C247, Veterinary Teaching Hospital University of Tennessee Knoxville, TN 37996-4544 Phone: 865-755-8219 FAX: 865-974-5554 Email: [email protected] 2 Treatment of pain in domestic and non-domestic cats has been a challenge for the clinician. Many cat species are stoic and show few or very subtle external signs of pain. Additionally, the adverse effects of nonsteroidal antiinflammatory drugs (NSAIDs) in domestic cats are well documented and have discouraged many practitioners from trying novel NSAID’s in exotic felids. As in other animals, each cat’s response to pain and analgesics will vary, necessitating an individualized treatment plan. As a rule, always treat painful felids to effect, and not by rote reliance on published dosages. It is frequently necessary to try different agents and combinations to find which produces the optimal analgesic effect in exotic felids. In order to minimize adverse effects, it is desirable to work toward treatment with the lowest effective dose when treating chronic pain. Non-steroidal Antiinflammatory Drugs NSAIDs are antiinflammatory drugs which act both centrally and peripherally. The primary effects are believed to be caused by their ability to inhibit cyclooxygenase (COX) enzymes in the arachidonic acid metabolism cascade. The COX-1 isoform is regarded as constitutive (continuously expressed) and is responsible for many homeostatic processes, such as maintenance of gastric mucosal integrity, platelet function, and renal autoregulation. -

Lasmiditan Is an Effective Acute Treatment for Migraine: a Phase 3 Randomized Study Bernice Kuca, Stephen D
ARTICLE OPEN ACCESS CLASS OF EVIDENCE Lasmiditan is an effective acute treatment for migraine A phase 3 randomized study Bernice Kuca, BA, MS, Stephen D. Silberstein, MD, Linda Wietecha, BSN, MS, Paul H. Berg, MS, Correspondence Gregory Dozier, MPH, and Richard B. Lipton, MD, on behalf of the COL MIG-301 Study Group Ms. Wietecha [email protected] Neurology® 2018;91:e2222-e2232. doi:10.1212/WNL.0000000000006641 Abstract RELATED ARTICLE Objective Article To assess the efficacy and safety of lasmiditan in the acute treatment of migraine. Galcanezumab in chronic migraine: The randomized, Methods double-blind, placebo- Adult patients with migraine were randomized (1:1:1) to a double-blind dose of oral lasmiditan controlled REGAIN study 200 mg, lasmiditan 100 mg, or placebo and were asked to treat their next migraine attack within Page 1082 4 hours of onset. Over 48 hours after dosing, patients used an electronic diary to record headache pain and the presence of nausea, phonophobia, and photophobia, one of which was MORE ONLINE designated their most bothersome symptom (MBS). Class of Evidence Criteria for rating Results ≥ therapeutic and diagnostic Of the 1,856 patients who treated an attack, 77.9% had 1 cardiovascular risk factors in addition studies to migraine. Compared with placebo, more patients dosed with lasmiditan 200 mg were free of NPub.org/coe headache pain at 2 hours after dosing (32.2% vs 15.3%; odds ratio [OR] 2.6, 95% confidence interval [CI] 2.0–3.6, p< 0.001), similar to those dosed with lasmiditan 100 mg (28.2%; OR 2.2, 95% CI 1.6–3.0, p< 0.001). -

Antimigraine Agents, Triptans Review 07/21/2008
Antimigraine Agents, Triptans Review 07/21/2008 Copyright © 2004 - 2008 by Provider Synergies, L.L.C. All rights reserved. Printed in the United States of America. All rights reserved. No part of this publication may be reproduced or transmitted in any form or by any means, electronic or mechanical, including photocopying, recording, digital scanning, or via any information storage and retrieval system without the express written consent of Provider Synergies, L.L.C. All requests for permission should be mailed to: Attention: Copyright Administrator Intellectual Property Department Provider Synergies, L.L.C. 5181 Natorp Blvd., Suite 205 Mason, Ohio 45040 The materials contained herein represent the opinions of the collective authors and editors and should not be construed to be the official representation of any professional organization or group, any state Pharmacy and Therapeutics committee, any state Medicaid Agency, or any other clinical committee. This material is not intended to be relied upon as medical advice for specific medical cases and nothing contained herein should be relied upon by any patient, medical professional or layperson seeking information about a specific course of treatment for a specific medical condition. All readers of this material are responsible for independently obtaining medical advice and guidance from their own physician and/or other medical professional in regard to the best course of treatment for their specific medical condition. This publication, inclusive of all forms contained herein, is intended -

Frovatriptan Versus Zolmitriptan for the Acute Treatment of Migraine: a Double-Blind, Randomized, Multicenter, Italian Study
Neurol Sci (2010) 31 (Suppl 1):S51–S54 DOI 10.1007/s10072-010-0273-x SYMPOSIUM: NEWS IN TREATMENT OF MIGRAINE ATTACK Frovatriptan versus zolmitriptan for the acute treatment of migraine: a double-blind, randomized, multicenter, Italian study Vincenzo Tullo • Gianni Allais • Michel D. Ferrari • Marcella Curone • Eliana Mea • Stefano Omboni • Chiara Benedetto • Dario Zava • Gennaro Bussone Ó The Author(s) 2010. This article is published with open access at Springerlink.com Abstract The objective of this study is to assess patients’ of PF episodes at 2 h was 26% with F and 31% with Z satisfaction with migraine treatment with frovatriptan (F) (p = NS). PR episodes at 2 h were 57% for F and 58% for or zolmitriptan (Z), by preference questionnaire. 133 sub- Z(p = NS). Rate of recurrence was 21 (F) and 24% jects with a history of migraine with or without aura (IHS (Z; p = NS). Time to recurrence within 48 h was better for criteria) were randomized to F 2.5 mg or Z 2.5 mg. The F especially between 4 and 16 h (p \ 0.05). SPF episodes study had a multicenter, randomized, double-blind, cross- were 18 (F) versus 22% (Z; p = NS). Drug-related adverse over design, with each of the two treatment periods lasting events were significantly (p \ 0.05) less under F (3 vs. 10). no more than 3 months. At the end of the study, patients In conclusion, our study suggests that F has a similar were asked to assign preference to one of the treatments efficacy of Z, with some advantage as regards tolerability (primary endpoint). -

Safety and Efficacy of a Continuous Infusion, Patient Controlled Anti
Bone Marrow Transplantation, (1999) 24, 561–566 1999 Stockton Press All rights reserved 0268–3369/99 $15.00 http://www.stockton-press.co.uk/bmt Safety and efficacy of a continuous infusion, patient controlled anti- emetic pump to facilitate outpatient administration of high-dose chemotherapy SP Dix, MK Cord, SJ Howard, JL Coon, RJ Belt and RB Geller Blood and Marrow Transplant Program, Oncology and Hematology Associates and Saint Luke’s Hospital of Kansas City, Kansas City, MO, USA Summary: and colleagues1 described an outpatient BMT care model utilizing intensive clinic support following inpatient admin- We evaluated the combination of diphenhydramine, lor- istration of HDC. This approach facilitated early patient azepam, and dexamethasone delivered as a continuous discharge and significantly decreased the total number of i.v. infusion via an ambulatory infusion pump with days of hospitalization associated with BMT. More patient-activated intermittent dosing (BAD pump) for recently, equipped BMT centers have extended the out- prevention of acute and delayed nausea/vomiting in patient care approach to include administration of HDC in patients receiving high-dose chemotherapy (HDC) for the clinic setting. Success of the total outpatient care peripheral blood progenitor cell (PBPC) mobilization approach is dependent upon the availability of experienced (MOB) or prior to autologous PBPC rescue. The BAD staff and necessary resources as well as implementation of pump was titrated to patient response and tolerance, supportive care strategies designed to minimize morbidity and continued until the patient could tolerate oral anti- in the outpatient setting. emetics. Forty-four patients utilized the BAD pump Despite improvements in supportive care strategies, during 66 chemotherapy courses, 34 (52%) for MOB chemotherapy-induced nausea and vomiting continues to be and 32 (48%) for HDC with autologous PBPC rescue.