Safety and Efficacy of a Continuous Infusion, Patient Controlled Anti
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medications and Alcohol Craving
Medications and Alcohol Craving Robert M. Swift, M.D., Ph.D. The use of medications as an adjunct to alcoholism treatment is based on the premise that craving and other manifestations of alcoholism are mediated by neurobiological mechanisms. Three of the four medications approved in the United States or Europe for treating alcoholism are reported to reduce craving; these include naltrexone (ReVia™), acamprosate, and tiapride. The remaining medication, disulfiram (Antabuse®), may also possess some anticraving activity. Additional medications that have been investigated include ritanserin, which has not been shown to decrease craving or drinking levels in humans, and ondansetron, which shows promise for treating early onset alcoholics, who generally respond poorly to psychosocial treatment alone. Use of anticraving medications in combination (e.g., naltrexone plus acamprosate) may enhance their effectiveness. Future studies should address such issues as optimal dosing regimens and the development of strategies to enhance patient compliance. KEY WORDS: AOD (alcohol and other drug) craving; anti alcohol craving agents; alcohol withdrawal agents; drug therapy; neurobiological theory; alcohol cue; disulfiram; naltrexone; calcium acetylhomotaurinate; dopamine; serotonin uptake inhibitors; buspirone; treatment outcome; reinforcement; neurotransmitters; patient assessment; literature review riteria for defining alcoholism Results of craving research are often tions (i.e., pharmacotherapy) to improve vary widely. Most definitions difficult to interpret, -

203050Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 203050Orig1s000 LABELING HIGHLIGHTS OF PRESCRIBING INFORMATION ------------------------------CONTRAINDICATIONS-------------------------------- These highlights do not include all the information needed to use Hypersensitivity to the drug or any of its components (4) PALONOSETRON HYDROCHLORIDE INJECTION safely and effectively. See full prescribing information for PALONOSETRON ------------------------WARNINGS AND PRECAUTIONS------------------------- HYDROCHLORIDE INJECTION. • Hypersensitivity reactions, including anaphylaxis, have been reported with or without known hypersensitivity to other selective 5-HT3 receptor antagonists PALONOSETRON HYDROCHLORIDE injection, for intravenous (5.1) use • Serotonin syndrome has been reported with 5-HT3 receptor antagonists alone Initial U.S. Approval: 2003 but particularly with concomitant use of serotonergic drugs (5.2, 7.1) -------------------------INDICATIONS AND USAGE------------------------ --------------------------------ADVERSE REACTIONS------------------------------- Palonosetron Hydrochloride (HCl) Injection is a serotonin-3 (5-HT3) The most common adverse reactions in chemotherapy-induced nausea and receptor antagonist indicated in adults for: vomiting (≥5%) are headache and constipation (6.1) • Moderately emetogenic cancer chemotherapy -- prevention of acute and delayed nausea and vomiting associated with initial and repeat The most common adverse reactions in postoperative nausea and vomiting (≥ courses (1.1) 2%) are QT prolongation, -

Haloperidol As Prophylactic Treatment for Postoperative
Document downloaded from http://http://www.revcolanest.com.co, day 15/02/2013. This copy is for personal use. Any transmission of this document by any media or format is strictly prohibited. r e v c o l o m b a n e s t e s i o l . 2 0 1 3;4 1(1):34–43 Revista Colombiana de Anestesiología Colombian Journal of Anesthesiology www.revcolanest.com.co Review Haloperidol as prophylactic treatment for postoperative ଝ nausea and vomiting: Systematic literature review ∗ Catalina Chaparro , Diego Moreno, Verónica Ramírez, Angélica Fajardo, David González, Alejandra Sanín, Reinaldo Grueso Anesthesiology Service, Hospital Universitario San Ignacio, Bogotá, Colombia a r t i c l e i n f o a b s t r a c t Article history: Introduction: The effectiveness of haloperidol for the prophylaxis of postoperative nausea Received 3 July 2012 and vomiting (PONV) has been proven in prior trials summarized by Buttner in 2004. New Accepted 24 July 2012 evidence has surfaced since then. Our objective is thus to update the current knowledge on the topic. A systematic review and a meta-analysis were performed, in order to determine the effectiveness and safety of the use of haloperidol as prophylaxis for PONV. Keywords: Methodology: The systematic search, the selection of relevant articles, the extraction of data, Haloperidol the critical analysis of the primary studies, the comparisons and analyses were all based on Vomiting the recommendations of the Cochrane Collaboration and using RevMan5 software. Nausea Results: Ten controlled clinical trials published between 1962 and 2010, that included 2,711 Clinical trials patients, met the selection criteria. -

Acute Migraine Treatment
Acute Migraine Treatment Morris Levin, MD Professor of Neurology Director, Headache Center UCSF Department of Neurology San Francisco, CA Mo Levin Disclosures Consulting Royalties Allergan Oxford University Press Supernus Anadem Press Amgen Castle Connolly Med. Publishing Lilly Wiley Blackwell Mo Levin Disclosures Off label uses of medication DHE Antiemetics Zolmitriptan Learning Objectives At the end of the program attendees will be able to 1. List all important options in the acute treatment of migraine 2. Discuss the evidence and guidelines supporting the major migraine acute treatment options 3. Describe potential adverse effects and medication- medication interactions in acute migraine pharmacological treatment Case 27 y/o woman has suffered ever since she can remember from “sick headaches” . Pain is frontal, increases over time and is generally accompanied by nausea and vomiting. She feels depressed. The headache lasts the rest of the day but after sleeping through the night she awakens asymptomatic 1. Diagnosis 2. Severe Headache relief Diagnosis: What do we need to beware of? • Misdiagnosis of primary headache • Secondary causes of headache Red Flags in HA New (recent onset or change in pattern) Effort or Positional Later onset than usual (middle age or later) Meningismus, Febrile AIDS, Cancer or other known Systemic illness - Neurological or psych symptoms or signs Basic principles of Acute Therapy of Headaches • Diagnose properly, including comorbid conditions • Stratify therapy rather than treat in steps • Treat early -
Hydroxyzine Prescribing Information
Hydroxyzine Hydroxyzine Hydrochloride Hydrochloride Injection, USP Injection, USP (For Intramuscular Use Only) (For Intramuscular Use Only) Rx Only Rx Only DESCRIPTION: Hydroxyzine hydrochloride has the chemical name of (±)-2-[2-[4-( p-Chloro- a- phenylbenzyl)-1-piperazinyl]ethoxy]ethanol dihydrochloride and occurs as a white, odorless powder which is very soluble in water. It has the following structural formula: Molecular Formula: C 21 H27 ClN 2O2•2HCl Molecular Weight: 447.83 Hydroxyzine Hydrochloride Injection, USP is a sterile aqueous solution intended for intramuscular administration. Each mL contains: Hydroxyzine HCl 25 mg or 50 mg, Benzyl Alcohol 0.9%, and Water for Injection q.s. pH adjusted with Sodium Hydroxide and/or Hydrochloric Acid. CLINICAL PHARMACOLOGY: Hydroxyzine hydrochloride is unrelated chemically to phenothiazine, reserpine, and meprobamate. Hydroxyzine has demonstrated its clinical effectiveness in the chemotherapeutic aspect of the total management of neuroses and emotional disturbances manifested by anxiety, tension, agitation, apprehension or confusion. Hydroxyzine has been shown clinically to be a rapid-acting true ataraxic with a wide margin of safety. It induces a calming effect in anxious, tense, psychoneurotic adults and also in anxious, hyperkinetic children without impairing mental alertness. It is not a cortical depressant, but its action may be due to a suppression of activity in certain key regions of the subcortical area of the central nervous system. Primary skeletal muscle relaxation has been demonstrated experimentally. Hydroxyzine has been shown experimentally to have antispasmodic properties, apparently mediated through interference with the mechanism that responds to spasmogenic agents such as serotonin, acetylcholine, and histamine. Antihistaminic effects have been demonstrated experimentally and confirmed clinically. -

5-HT3 Receptor Antagonists in Neurologic and Neuropsychiatric Disorders: the Iceberg Still Lies Beneath the Surface
1521-0081/71/3/383–412$35.00 https://doi.org/10.1124/pr.118.015487 PHARMACOLOGICAL REVIEWS Pharmacol Rev 71:383–412, July 2019 Copyright © 2019 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: JEFFREY M. WITKIN 5-HT3 Receptor Antagonists in Neurologic and Neuropsychiatric Disorders: The Iceberg Still Lies beneath the Surface Gohar Fakhfouri,1 Reza Rahimian,1 Jonas Dyhrfjeld-Johnsen, Mohammad Reza Zirak, and Jean-Martin Beaulieu Department of Psychiatry and Neuroscience, Faculty of Medicine, CERVO Brain Research Centre, Laval University, Quebec, Quebec, Canada (G.F., R.R.); Sensorion SA, Montpellier, France (J.D.-J.); Department of Pharmacodynamics and Toxicology, School of Pharmacy, Mashhad University of Medical Sciences, Mashhad, Iran (M.R.Z.); and Department of Pharmacology and Toxicology, University of Toronto, Toronto, Ontario, Canada (J.-M.B.) Abstract. ....................................................................................384 I. Introduction. ..............................................................................384 II. 5-HT3 Receptor Structure, Distribution, and Ligands.........................................384 A. 5-HT3 Receptor Agonists .................................................................385 B. 5-HT3 Receptor Antagonists. ............................................................385 Downloaded from 1. 5-HT3 Receptor Competitive Antagonists..............................................385 2. 5-HT3 Receptor -

The Vomiting Center and the Chemoreceptor Trigger Zone
Pharmacologic Control of Vomiting Todd R. Tams, DVM, Dipl. ACVIM VCA West Los Angeles Animal Hospital Pharmacologic Control of Acute Vomiting Initial nonspecific management of vomiting includes NPO (in minor cases a 6-12 hour period of nothing per os may be all that is required), fluid support, and antiemetics. Initial feeding includes small portions of a low fat, single source protein diet starting 6-12 hours after vomiting has ceased. Drugs used to control vomiting will be discussed here. The most effective antiemetics are those that act at both the vomiting center and the chemoreceptor trigger zone. Vomiting is a protective reflex and when it occurs only occasionally treatment is not generally required. However, patients that continue to vomit should be given antiemetics to help reduce fluid loss, pain and discomfort. For many years I strongly favored chlorpromazine (Thorazine), a phenothiazine drug, as the first choice for pharmacologic control of vomiting in most cases. The HT-3 receptor antagonists ondansetron (Zofran) and dolasetron (Anzemet) have also been highly effective antiemetic drugs for a variety of causes of vomiting. Metoclopramide (Reglan) is a reasonably good central antiemetic drug for dogs but not for cats. Maropitant (Cerenia) is a superior broad spectrum antiemetic drug and is now recognized as an excellent first choice for control of vomiting in dogs. Studies and clinical experience have now also shown maropitant to be an effective and safe antiemetic drug for cats. While it is labeled only for dogs, clinical experience has shown it is safe to use the drug in cats as well. Maropitant is also the first choice for prevention of motion sickness vomiting in both dogs and cats. -

Effect of Naltrexone and Ondansetron on Alcohol Cue–Induced Activation of the Ventral Striatum in Alcohol-Dependent People
ORIGINAL ARTICLE Effect of Naltrexone and Ondansetron on Alcohol Cue–Induced Activation of the Ventral Striatum in Alcohol-Dependent People Hugh Myrick, MD; Raymond F. Anton, MD; Xingbao Li, MD; Scott Henderson, BA; Patrick K. Randall, PhD; Konstantin Voronin, MD, PhD Context: Medication for the treatment of alcoholism is double-blind randomly assigned daily dosing with 50 mg currently not particularly robust. Neuroimaging tech- of naltrexone (n=23), 0.50 mg of ondansetron hydro- niques might predict which medications could be use- chloride (n=23), the combination of the 2 medications ful in the treatment of alcohol dependence. (n=20), or matching placebos (n=24). Objective: To explore the effect of naltrexone, ondanse- Main Outcome Measures: Difference in brain blood tron hydrochloride, or the combination of these medi- oxygen level–dependent magnetic resonance when view- cations on cue-induced craving and ventral striatum ac- ing alcohol pictures vs neutral beverage pictures with a tivation. particular focus on ventral striatum activity comparison across medication groups. Self-ratings of alcohol craving. Design: Functional brain imaging was conducted dur- ing alcohol cue presentation. Results: The combination treatment decreased craving for alcohol. Naltrexone with (P=.02) or without (P=.049) Setting: Participants were recruited from the general ondansetron decreased alcohol cue–induced activation community following media advertisement. Experimen- of the ventral striatum. Ondansetron by itself was simi- tal procedures were performed in the magnetic reso- lar to naltrexone and the combination in the overall analy- nance imaging suite of a major training hospital and medi- sis but intermediate in a region-specific analysis. cal research institute. -
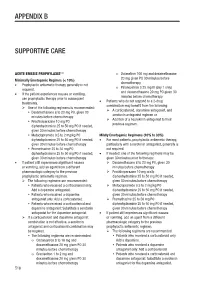
Appendix B Supportive Care
APPENDIX B SUPPORTIVE CARE 1-4 ACUTE EMESIS PROPHYLAXIS o Dolasetron 100 mg and dexamethasone 20 mg given PO 30 minutes before Minimally Emetogenic Regimes (< 10%) chemotherapy • Prophylactic antiemetic therapy generally is not Palonosetron 0.25 mg IV (day 1 only) required. o and dexamethasone 20 mg PO given 30 • If the patient experiences nausea or vomiting, minutes before chemotherapy use prophylactic therapy prior to subsequent Patients who do not respond to a 2-drug treatments. • combination may benefit from the following: One of the following regimens is recommended: A corticosteroid, dopamine antagonist, and Dexamethasone 8 to 20 mg PO, given 30 serotonin antagonist regimen or minutes before chemotherapy Addition of a neurokinin antagonist to their Prochlorperazine 10 mg PO ± previous regimen. diphenhydramine 25 to 50 mg PO if needed, given 30 minutes before chemotherapy Metoclopramide 0.5 to 2 mg/kg PO ± Mildly Emetogenic Regimens (10% to 30%) diphenhydramine 25 to 50 mg PO if needed, • For most patients, prophylactic antiemetic therapy, given 30 minutes before chemotherapy particularly with a serotonin antagonist, generally is Promethazine 25 to 50 mg PO ± not required. diphenhydramine 25 to 50 mg PO if needed, • If needed, one of the following regimens may be given 30 minutes before chemotherapy given 30 minutes prior to therapy: • If patient still experiences significant nausea Dexamethasone 8 to 20 mg PO, given 30 or vomiting, add an agent from a different minutes before chemotherapy pharmacologic category to the previous Prochlorperazine 10 mg orally ± prophylactic antiemetic regimen. diphenhydramine 25 to 50 mg PO if needed, The following regimens are recommended: given 30 minutes before chemotherapy Patients who received a corticosteroid only: Metoclopramide 0.5 to 2 mg/kg PO ± Add a dopamine antagonist. -

Hallucinogens: an Update
National Institute on Drug Abuse RESEARCH MONOGRAPH SERIES Hallucinogens: An Update 146 U.S. Department of Health and Human Services • Public Health Service • National Institutes of Health Hallucinogens: An Update Editors: Geraline C. Lin, Ph.D. National Institute on Drug Abuse Richard A. Glennon, Ph.D. Virginia Commonwealth University NIDA Research Monograph 146 1994 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service National Institutes of Health National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 ACKNOWLEDGEMENT This monograph is based on the papers from a technical review on “Hallucinogens: An Update” held on July 13-14, 1992. The review meeting was sponsored by the National Institute on Drug Abuse. COPYRIGHT STATUS The National Institute on Drug Abuse has obtained permission from the copyright holders to reproduce certain previously published material as noted in the text. Further reproduction of this copyrighted material is permitted only as part of a reprinting of the entire publication or chapter. For any other use, the copyright holder’s permission is required. All other material in this volume except quoted passages from copyrighted sources is in the public domain and may be used or reproduced without permission from the Institute or the authors. Citation of the source is appreciated. Opinions expressed in this volume are those of the authors and do not necessarily reflect the opinions or official policy of the National Institute on Drug Abuse or any other part of the U.S. Department of Health and Human Services. The U.S. Government does not endorse or favor any specific commercial product or company. -

Important Interaction Between Mirtazapine and Ondansetron
SCIENTIFIC LETTER | http://dx.doi.org/10.4314/ajpsy.v15i3.19 Afr J Psychiatry 2012;15:160 Important interaction between mirtazapine and ondansetron Drug interaction in psychiatry is a clinically important issue, as serotonergic antidepressant with a half-life of 20-40 hours. Apart it can cause side-effects and prevent adequate therapeutic from its presynaptic antagonistic effect on alpha 2-receptors with effect. We report an unexpected interaction between the release of both noradrenaline and serotonin – the postulated antidepressant mirtazapine and the antiemetic ondansetron in antidepressant effect – the compound antagonizes 5-HT2c, 5- a 72 year old patient, weighing 68 kg, with a height of 173 cm. HT2a (sedation, sleep, appetite) and 5-HT3-receptors (nausea). 1 The patient, who gave his informed consent for anonymous Ondansetron is a relatively specific 5-HT3-antagonist used publication, underwent electro-convulsive therapy (ECT), using particularly in postoperative nausea and vomiting (PONV) in a Thymatron System II, Somatics LLC with bitemporal electrode intravenous 4 mg doses. 2 Ki-value (binding affinity of an inhibitor, position, energy 40 repeated with 50 % (corresponding ligand concentration which occupies 50% of a receptor) of charge: 257 mC, current: 0.92 A, duration of stimulation 7 sec, ondansetron is 7.6 nMol, i. e. approximately 1/9 of the Ki-value of frequency 40 Hz) due to chronic severe depression. He was on mirtazapine (about 70 nMol). 3 The affinity of mirtazapine – with pharmacological treatment with mirtazapine (45 mg daily) and regard to normal antidepressant dose up to 45 mg - was venlafaxine (75 mg daily). The patient complained of severe obviously not sufficient to block acute PONV, however, was able nausea and vomiting after the first ECT session. -

ASCO's Antiemetics Drug, Dose, and Schedule Table
ASCO 2017 Antiemetics Guideline Update: Drug, Dose, Schedule Recommendations for Antiemetic Regimens Antiemetic Dosing by Chemotherapy Risk Category Agent Dose on Day of Chemotherapy Dose(s) on Subsequent Days High Emetic Risk: Cisplatin and other agents Aprepitant 125 mg oral 80 mg oral; days 2 and 3 Fosaprepitant 150 mg IV NK1 Receptor 300 mg netupitant/0.5 mg palonosetron oral in single Antagonist Netupitant-palonosetron capsule (NEPA) Rolapitant 180 mg oral 2 mg oral or 1 mg or 0.01 mg/kg IV or 1 transdermal Granisetron patch or 10 mg subcutaneous 8 mg oral twice daily or 8 mg oral dissolving tablet Ondansetron twice daily or three 8 mg oral soluble films or 8 mg or 5-HT3 Receptor 0.15 mg/kg IV Antagonista Palonosetron 0.50 mg oral or 0.25 mg IV Dolasetron 100 mg oral ONLY Tropisetron 5 mg oral or 5 mg IV Ramosetron 0.3 mg IV if aprepitant is usedb 12 mg oral or IV 8 mg oral or IV once daily on days 2-4 8 mg oral or IV on day 2; 8 mg oral or IV twice if fosaprepitant is usedb 12 mg oral or IV Dexamethasone daily on days 3-4 if netupitant-palonosetron 12 mg oral or IV 8 mg oral or IV once daily on days 2 to 4 is usedb This table is derived from recommendations in the Antiemetics Guideline Update (2017). This table is a practice tool based on ASCO® practice guidelines and is not intended to substitute for the independent professional judgment of the treating physician.