Synergistic Action of 5-HT2A Antagonists and Selective Serotonin Reuptake Inhibitors in Neuropsychiatric Disorders
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pindolol of the Activation of Postsynaptic 5-HT1A Receptors
Potentiation by (-)Pindolol of the Activation of Postsynaptic 5-HT1A Receptors Induced by Venlafaxine Jean-Claude Béïque, Ph.D., Pierre Blier, M.D., Ph.D., Claude de Montigny, M.D., Ph.D., and Guy Debonnel, M.D. The increase of extracellular 5-HT in brain terminal regions antagonist WAY 100635 (100 g/kg, i.v.). A short-term produced by the acute administration of 5-HT reuptake treatment with VLX (20 mg/kg/day ϫ 2 days) resulted in a inhibitors (SSRI’s) is hampered by the activation of ca. 90% suppression of the firing activity of 5-HT neurons somatodendritic 5-HT1A autoreceptors in the raphe nuclei. in the dorsal raphe nucleus. This was prevented by the The present in vivo electrophysiological studies were coadministration of (-)pindolol (15 mg/kg/day ϫ 2 days). undertaken, in the rat, to assess the effects of the Taken together, these results indicate that (-)pindolol coadministration of venlafaxine, a dual 5-HT/NE reuptake potentiated the activation of postsynaptic 5-HT1A receptors inhibitor, and (-)pindolol on pre- and postsynaptic 5-HT1A resulting from 5-HT reuptake inhibition probably by receptor function. The acute administration of venlafaxine blocking the somatodendritic 5-HT1A autoreceptor, but not and of the SSRI paroxetine (5 mg/kg, i.v.) induced a its postsynaptic congener. These results support and extend suppression of the firing activity of dorsal hippocampus CA3 previous findings providing a biological substratum for the pyramidal neurons. This effect of venlafaxine was markedly efficacy of pindolol as an accelerating strategy in major potentiated by a pretreatment with (-)pindolol (15 mg/kg, depression. -

Molecular Signatures of G-Protein-Coupled Receptors A
REVIEW doi:10.1038/nature11896 Molecular signatures of G-protein-coupled receptors A. J. Venkatakrishnan1, Xavier Deupi2, Guillaume Lebon1,3,4,5, Christopher G. Tate1, Gebhard F. Schertler2,6 & M. Madan Babu1 G-protein-coupled receptors (GPCRs) are physiologically important membrane proteins that sense signalling molecules such as hormones and neurotransmitters, and are the targets of several prescribed drugs. Recent exciting developments are providing unprecedented insights into the structure and function of several medically important GPCRs. Here, through a systematic analysis of high-resolution GPCR structures, we uncover a conserved network of non-covalent contacts that defines the GPCR fold. Furthermore, our comparative analysis reveals characteristic features of ligand binding and conformational changes during receptor activation. A holistic understanding that integrates molecular and systems biology of GPCRs holds promise for new therapeutics and personalized medicine. ignal transduction is a fundamental biological process that is comprehensively, and in the process expand the current frontiers of required to maintain cellular homeostasis and to ensure coordi- GPCR biology. S nated cellular activity in all organisms. Membrane proteins at the In this analysis, we objectively compare known structures and reveal cell surface serve as the communication interface between the cell’s key similarities and differences among diverse GPCRs. We identify a external and internal environments. One of the largest and most diverse consensus structural scaffold of GPCRs that is constituted by a network membrane protein families is the GPCRs, which are encoded by more of non-covalent contacts between residues on the transmembrane (TM) than 800 genes in the human genome1. GPCRs function by detecting a helices. -

Appendix A: Potentially Inappropriate Prescriptions (Pips) for Older People (Modified from ‘STOPP/START 2’ O’Mahony Et Al 2014)
Appendix A: Potentially Inappropriate Prescriptions (PIPs) for older people (modified from ‘STOPP/START 2’ O’Mahony et al 2014) Consider holding (or deprescribing - consult with patient): 1. Any drug prescribed without an evidence-based clinical indication 2. Any drug prescribed beyond the recommended duration, where well-defined 3. Any duplicate drug class (optimise monotherapy) Avoid hazardous combinations e.g.: 1. The Triple Whammy: NSAID + ACE/ARB + diuretic in all ≥ 65 year olds (NHS Scotland 2015) 2. Sick Day Rules drugs: Metformin or ACEi/ARB or a diuretic or NSAID in ≥ 65 year olds presenting with dehydration and/or acute kidney injury (AKI) (NHS Scotland 2015) 3. Anticholinergic Burden (ACB): Any additional medicine with anticholinergic properties when already on an Anticholinergic/antimuscarinic (listed overleaf) in > 65 year olds (risk of falls, increased anticholinergic toxicity: confusion, agitation, acute glaucoma, urinary retention, constipation). The following are known to contribute to the ACB: Amantadine Antidepressants, tricyclic: Amitriptyline, Clomipramine, Dosulepin, Doxepin, Imipramine, Nortriptyline, Trimipramine and SSRIs: Fluoxetine, Paroxetine Antihistamines, first generation (sedating): Clemastine, Chlorphenamine, Cyproheptadine, Diphenhydramine/-hydrinate, Hydroxyzine, Promethazine; also Cetirizine, Loratidine Antipsychotics: especially Clozapine, Fluphenazine, Haloperidol, Olanzepine, and phenothiazines e.g. Prochlorperazine, Trifluoperazine Baclofen Carbamazepine Disopyramide Loperamide Oxcarbazepine Pethidine -

Emerging Evidence for a Central Epinephrine-Innervated A1- Adrenergic System That Regulates Behavioral Activation and Is Impaired in Depression
Neuropsychopharmacology (2003) 28, 1387–1399 & 2003 Nature Publishing Group All rights reserved 0893-133X/03 $25.00 www.neuropsychopharmacology.org Perspective Emerging Evidence for a Central Epinephrine-Innervated a1- Adrenergic System that Regulates Behavioral Activation and is Impaired in Depression ,1 1 1 1 1 Eric A Stone* , Yan Lin , Helen Rosengarten , H Kenneth Kramer and David Quartermain 1Departments of Psychiatry and Neurology, New York University School of Medicine, New York, NY, USA Currently, most basic and clinical research on depression is focused on either central serotonergic, noradrenergic, or dopaminergic neurotransmission as affected by various etiological and predisposing factors. Recent evidence suggests that there is another system that consists of a subset of brain a1B-adrenoceptors innervated primarily by brain epinephrine (EPI) that potentially modulates the above three monoamine systems in parallel and plays a critical role in depression. The present review covers the evidence for this system and includes findings that brain a -adrenoceptors are instrumental in behavioral activation, are located near the major monoamine cell groups 1 or target areas, receive EPI as their neurotransmitter, are impaired or inhibited in depressed patients or after stress in animal models, and a are restored by a number of antidepressants. This ‘EPI- 1 system’ may therefore represent a new target system for this disorder. Neuropsychopharmacology (2003) 28, 1387–1399, advance online publication, 18 June 2003; doi:10.1038/sj.npp.1300222 Keywords: a1-adrenoceptors; epinephrine; motor activity; depression; inactivity INTRODUCTION monoaminergic systems. This new system appears to be impaired during stress and depression and thus may Depressive illness is currently believed to result from represent a new target for this disorder. -

Strategies for Managing Sexual Dysfunction Induced by Antidepressant Medication
King’s Research Portal DOI: 10.1002/14651858.CD003382.pub3 Document Version Publisher's PDF, also known as Version of record Link to publication record in King's Research Portal Citation for published version (APA): Taylor, M. J., Rudkin, L., Bullemor-Day, P., Lubin, J., Chukwujekwu, C., & Hawton, K. (2013). Strategies for managing sexual dysfunction induced by antidepressant medication. Cochrane Database of Systematic Reviews, (5). https://doi.org/10.1002/14651858.CD003382.pub3 Citing this paper Please note that where the full-text provided on King's Research Portal is the Author Accepted Manuscript or Post-Print version this may differ from the final Published version. If citing, it is advised that you check and use the publisher's definitive version for pagination, volume/issue, and date of publication details. And where the final published version is provided on the Research Portal, if citing you are again advised to check the publisher's website for any subsequent corrections. General rights Copyright and moral rights for the publications made accessible in the Research Portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognize and abide by the legal requirements associated with these rights. •Users may download and print one copy of any publication from the Research Portal for the purpose of private study or research. •You may not further distribute the material or use it for any profit-making activity or commercial gain •You may freely distribute the URL identifying the publication in the Research Portal Take down policy If you believe that this document breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. -

Adrenergic Antagonist
PHARMACOLOGY Adrenergic antagonist OBJECTIVES: • Describe the different classifications for drugs that can block sympathetic nervous system. •Describe the kinetics, dynamics, uses and side effects of alpha adrenergic drugs. • Identify Difference between selective and non selective alpha blockers. • Know the difference between tamsulosin and other selective alpha receptor blockers. •Identify the different classifications for beta receptors blockers. •Describe the kinetics, dynamics, uses and side effects of beta adrenergic drugs. •Know the preferable drug for diseases as hypertension, glaucoma, arrythmia, myocardial infarction, anxiety, migraine and ect…. • Important. • Extra notes It’s a recall, if you know it you can skip it! Adrenergic receptors Adrenergic receptors Dopaminergic adrenoceptors adrenoceptors α− β− receptors β3 α1 α2 β1 β2 e.g. D1 α1 β2 β1 β3 Post-synaptic excitatory in function (cause inhibitory in function excitatory in In adipose contraction) except in GIT. (cause relaxation) function, present tissue mainly in heart Present mainly in smooth muscles. Contraction of pregnant Relaxation of the uterus ↑ heart rate: ↑ lipolysis uterus. (Delay premature labor) + chronotropic ↑ free fatty effect, Vasoconstriction of skin & Relaxation of skeletal & acids. Tachycardia peripheral blood vessels coronary blood vessels →increased peripheral (vasodilatation) ↑ force of → resistance hypertension. contraction : Relaxation of GIT muscles & urinary bladder’s muscles. + inotropic effect Contraction of GIT sphincter (constipation) & urinary -
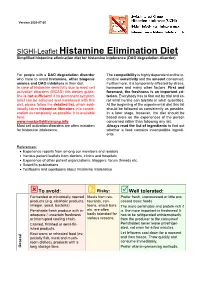
SIGHI-Leaflet Histamine Elimination Diet Simplified Histamine Elimination Diet for Histamine Intolerance (DAO Degradation Disorder)
Version 2020-07-20 SIGHI-Leaflet Histamine Elimination Diet Simplified histamine elimination diet for histamine intolerance (DAO degradation disorder) For people with a DAO degradation disorder The compatibility is highly dependent on the in- who have to avoid histamine, other biogenic dividual sensitivity and the amount consumed. amines and DAO inhibitors in their diet. Furthermore, it is temporarily affected by stress, In case of histamine sensitivity due to mast cell hormones and many other factors. First and activation disorders (MCAD) this dietary guide- foremost, the freshness is an important cri- line is not sufficient! If no permanent symptom terion. Everybody has to find out by trial and er- relief can be achieved and maintained with this ror what he/she can tolerate in what quantities. diet, please follow the detailed list, which addi- At the beginning of the experimental diet this list tionally takes histamine liberators into consid- should be followed as consistently as possible. eration as completely as possible. It is available In a later stage, however, the diet should be here: based more on the experiences of the person www.mastzellaktivierung.info concerned rather than following any list. Mast cell activation disorders are often mistaken Always read the list of ingredients to find out for histamine intolerance. whether a food contains incompatible ingredi- ents. References: • Experience reports from among our members and readers • Various patient leaflets from doctors, clinics and hospitals • Experience of other patient organizations, bloggers, forum threads etc. • Scientific publications • Textbooks and cookbooks about histamine intolerance To avoid: ? Risky: Well tolerated: Fermented or microbially ripened Meals from res- Prefer fresh, unprocessed or little pro- products (e.g. -

The In¯Uence of Medication on Erectile Function
International Journal of Impotence Research (1997) 9, 17±26 ß 1997 Stockton Press All rights reserved 0955-9930/97 $12.00 The in¯uence of medication on erectile function W Meinhardt1, RF Kropman2, P Vermeij3, AAB Lycklama aÁ Nijeholt4 and J Zwartendijk4 1Department of Urology, Netherlands Cancer Institute/Antoni van Leeuwenhoek Hospital, Plesmanlaan 121, 1066 CX Amsterdam, The Netherlands; 2Department of Urology, Leyenburg Hospital, Leyweg 275, 2545 CH The Hague, The Netherlands; 3Pharmacy; and 4Department of Urology, Leiden University Hospital, P.O. Box 9600, 2300 RC Leiden, The Netherlands Keywords: impotence; side-effect; antipsychotic; antihypertensive; physiology; erectile function Introduction stopped their antihypertensive treatment over a ®ve year period, because of side-effects on sexual function.5 In the drug registration procedures sexual Several physiological mechanisms are involved in function is not a major issue. This means that erectile function. A negative in¯uence of prescrip- knowledge of the problem is mainly dependent on tion-drugs on these mechanisms will not always case reports and the lists from side effect registries.6±8 come to the attention of the clinician, whereas a Another way of looking at the problem is drug causing priapism will rarely escape the atten- combining available data on mechanisms of action tion. of drugs with the knowledge of the physiological When erectile function is in¯uenced in a negative mechanisms involved in erectile function. The way compensation may occur. For example, age- advantage of this approach is that remedies may related penile sensory disorders may be compen- evolve from it. sated for by extra stimulation.1 Diminished in¯ux of In this paper we will discuss the subject in the blood will lead to a slower onset of the erection, but following order: may be accepted. -

Medications and Alcohol Craving
Medications and Alcohol Craving Robert M. Swift, M.D., Ph.D. The use of medications as an adjunct to alcoholism treatment is based on the premise that craving and other manifestations of alcoholism are mediated by neurobiological mechanisms. Three of the four medications approved in the United States or Europe for treating alcoholism are reported to reduce craving; these include naltrexone (ReVia™), acamprosate, and tiapride. The remaining medication, disulfiram (Antabuse®), may also possess some anticraving activity. Additional medications that have been investigated include ritanserin, which has not been shown to decrease craving or drinking levels in humans, and ondansetron, which shows promise for treating early onset alcoholics, who generally respond poorly to psychosocial treatment alone. Use of anticraving medications in combination (e.g., naltrexone plus acamprosate) may enhance their effectiveness. Future studies should address such issues as optimal dosing regimens and the development of strategies to enhance patient compliance. KEY WORDS: AOD (alcohol and other drug) craving; anti alcohol craving agents; alcohol withdrawal agents; drug therapy; neurobiological theory; alcohol cue; disulfiram; naltrexone; calcium acetylhomotaurinate; dopamine; serotonin uptake inhibitors; buspirone; treatment outcome; reinforcement; neurotransmitters; patient assessment; literature review riteria for defining alcoholism Results of craving research are often tions (i.e., pharmacotherapy) to improve vary widely. Most definitions difficult to interpret, -

Schizophrenia Care Guide
August 2015 CCHCS/DHCS Care Guide: Schizophrenia SUMMARY DECISION SUPPORT PATIENT EDUCATION/SELF MANAGEMENT GOALS ALERTS Minimize frequency and severity of psychotic episodes Suicidal ideation or gestures Encourage medication adherence Abnormal movements Manage medication side effects Delusions Monitor as clinically appropriate Neuroleptic Malignant Syndrome Danger to self or others DIAGNOSTIC CRITERIA/EVALUATION (PER DSM V) 1. Rule out delirium or other medical illnesses mimicking schizophrenia (see page 5), medications or drugs of abuse causing psychosis (see page 6), other mental illness causes of psychosis, e.g., Bipolar Mania or Depression, Major Depression, PTSD, borderline personality disorder (see page 4). Ideas in patients (even odd ideas) that we disagree with can be learned and are therefore not necessarily signs of schizophrenia. Schizophrenia is a world-wide phenomenon that can occur in cultures with widely differing ideas. 2. Diagnosis is made based on the following: (Criteria A and B must be met) A. Two of the following symptoms/signs must be present over much of at least one month (unless treated), with a significant impact on social or occupational functioning, over at least a 6-month period of time: Delusions, Hallucinations, Disorganized Speech, Negative symptoms (social withdrawal, poverty of thought, etc.), severely disorganized or catatonic behavior. B. At least one of the symptoms/signs should be Delusions, Hallucinations, or Disorganized Speech. TREATMENT OPTIONS MEDICATIONS Informed consent for psychotropic -

THE USE of MIRTAZAPINE AS a HYPNOTIC O Uso Da Mirtazapina Como Hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa
ARTIGO ESPECIAL THE USE OF MIRTAZAPINE AS A HYPNOTIC O uso da mirtazapina como hipnótico Francisca Magalhães Scoralicka, Einstein Francisco Camargosa, Otávio Toledo Nóbregaa Prescription of approved hypnotics for insomnia decreased by more than 50%, whereas of antidepressive agents outstripped that of hypnotics. However, there is little data on their efficacy to treat insomnia, and many of these medications may be associated with known side effects. Antidepressants are associated with various effects on sleep patterns, depending on the intrinsic pharmacological properties of the active agent, such as degree of inhibition of serotonin or noradrenaline reuptake, effects on 5-HT1A and 5-HT2 receptors, action(s) at alpha-adrenoceptors, and/or histamine H1 sites. Mirtazapine is a noradrenergic and specific serotonergic antidepressive agent that acts by antagonizing alpha-2 adrenergic receptors and blocking 5-HT2 and 5-HT3 receptors. It has high affinity for histamine H1 receptors, low affinity for dopaminergic receptors, and lacks anticholinergic activity. In spite of these potential beneficial effects of mirtazapine on sleep, no placebo-controlled randomized clinical trials of ABSTRACT mirtazapine in primary insomniacs have been conducted. Mirtazapine was associated with improvements in sleep on normal sleepers and depressed patients. The most common side effects of mirtazapine, i.e. dry mouth, drowsiness, increased appetite and increased body weight, were mostly mild and transient. Considering its use in elderly people, this paper provides a revision about studies regarding mirtazapine for sleep disorders. KEYWORDS: sleep; antidepressive agents; sleep disorders; treatment� A prescrição de hipnóticos aprovados para insônia diminuiu em mais de 50%, enquanto de antidepressivos ultrapassou a dos primeiros. -

Serotonin and Drug-Induced Therapeutic Responses in Major Depression, Obsessive–Compulsive and Panic Disorders Pierre Blier, M.D., Ph.D
Serotonin and Drug-Induced Therapeutic Responses in Major Depression, Obsessive–Compulsive and Panic Disorders Pierre Blier, M.D., Ph.D. and Claude de Montigny, M.D., Ph.D. The therapeutic effectiveness of antidepressant drugs in major development of treatment strategies producing greater efficacy depression was discovered by pure serendipity. It took over 20 and more rapid onset of antidepressant action; that, is lithium years before the neurobiological modifications that could addition and pindolol combination, respectively. It is expected mediate the antidepressive response were put into evidence. that the better understanding recently obtained of the Indeed, whereas the immediate biochemical effects of these mechanism of action of certain antidepressant drugs in drugs had been well documented, their antidepressant action obsessive– compulsive and panic disorders will also lead to generally does not become apparent before 2 to 3 weeks of more effective treatment strategies for those disorders. treatment. The different classes of antidepressant [Neuropsychopharmacology 21:91S–98S, 1999] treatments were subsequently shown to enhance serotonin © 1999 American College of Neuropsychopharmacology. neurotransmission albeit via different pre- and postsynaptic Published by Elsevier Science Inc. mechanisms. Clinical trials based on this hypothesis led to the KEY WORDS: Antidepressant; Electroconvulsive shocks; electroconvulsive shock treatment (ECT), which was Lithium; Pindolol; Hippocampus; Orbito-frontal cortex generally given only to hospitalized patients. It took several years after the demonstration of the In the late 1950s, the therapeutic effect of certain drugs antidepressant effect of iproniazide and imipramine to in major depression was discovered by serendipity. An understand that these drugs could interfere with the ca- antidepressant response was observed in patients with tabolism of monoamines.