Buproprion Metabolites for Treating Dementia and Other
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

124.210 Schedule IV — Substances Included. 1
1 CONTROLLED SUBSTANCES, §124.210 124.210 Schedule IV — substances included. 1. Schedule IV shall consist of the drugs and other substances, by whatever official name, common or usual name, chemical name, or brand name designated, listed in this section. 2. Narcotic drugs. Unless specifically excepted or unless listed in another schedule, any material, compound, mixture, or preparation containing any of the following narcotic drugs, or their salts calculated as the free anhydrous base or alkaloid, in limited quantities as set forth below: a. Not more than one milligram of difenoxin and not less than twenty-five micrograms of atropine sulfate per dosage unit. b. Dextropropoxyphene (alpha-(+)-4-dimethylamino-1,2-diphenyl-3-methyl-2- propionoxybutane). c. 2-[(dimethylamino)methyl]-1-(3-methoxyphenyl)cyclohexanol, its salts, optical and geometric isomers and salts of these isomers (including tramadol). 3. Depressants. Unless specifically excepted or unless listed in another schedule, any material, compound, mixture, or preparation which contains any quantity of the following substances, including its salts, isomers, and salts of isomers whenever the existence of such salts, isomers, and salts of isomers is possible within the specific chemical designation: a. Alprazolam. b. Barbital. c. Bromazepam. d. Camazepam. e. Carisoprodol. f. Chloral betaine. g. Chloral hydrate. h. Chlordiazepoxide. i. Clobazam. j. Clonazepam. k. Clorazepate. l. Clotiazepam. m. Cloxazolam. n. Delorazepam. o. Diazepam. p. Dichloralphenazone. q. Estazolam. r. Ethchlorvynol. s. Ethinamate. t. Ethyl Loflazepate. u. Fludiazepam. v. Flunitrazepam. w. Flurazepam. x. Halazepam. y. Haloxazolam. z. Ketazolam. aa. Loprazolam. ab. Lorazepam. ac. Lormetazepam. ad. Mebutamate. ae. Medazepam. af. Meprobamate. ag. Methohexital. ah. Methylphenobarbital (mephobarbital). -

Narcolepsy: Current Treatment Options and Future Approaches
REVIEW Narcolepsy: current treatment options and future approaches Michel Billiard Abstract: The management of narcolepsy is presently at a turning point. Three main avenues Department of Neurology, Gui de are considered in this review: 1) Two tendencies characterize the conventional treatment of Chauliac Hospital, Montpellier, France narcolepsy. Modafi nil has replaced methylphenidate and amphetamine as the fi rst-line treat- ment of excessive daytime sleepiness (EDS) and sleep attacks, based on randomized, double blind, placebo-controlled clinical trials of modafi nil, but on no direct comparison of modafi nil versus traditional stimulants. For cataplexy, sleep paralysis, and hypnagogic hallucinations, new antidepressants tend to replace tricyclic antidepressants and selective serotonin reuptake inhibitors (SSRIs) in spite of a lack of randomized, double blind, placebo-controlled clinical trials of these compounds; 2) The conventional treatment of narcolepsy is now challenged by sodium oxybate, the sodium salt of gammahydroxybutyrate, based on a series of randomized, double-blind, placebo-controlled clinical trials and a long-term open label study. This treatment has a fairly good effi cacy and is active on all symptoms of narcolepsy. Careful titration up to an adequate level is essential both to obtain positive results and avoid adverse effects; 3) A series of new treatments are currently being tested, either in animal models or in humans, They include novel stimulant and anticataplectic drugs, endocrine therapy, and, more attractively, -

(12) Patent Application Publication (10) Pub. No.: US 2009/0005722 A1 Jennings-Spring (43) Pub
US 20090005722A1 (19) United States (12) Patent Application Publication (10) Pub. No.: US 2009/0005722 A1 Jennings-Spring (43) Pub. Date: Jan. 1, 2009 (54) SKIN-CONTACTING-ADHESIVE FREE Publication Classification DRESSING (51) Int. Cl. Inventor: Barbara Jennings-Spring, Jupiter, A61N L/30 (2006.01) (76) A6F I3/00 (2006.01) FL (US) A6IL I5/00 (2006.01) Correspondence Address: AOIG 7/06 (2006.01) Irving M. Fishman AOIG 7/04 (2006.01) c/o Cohen, Tauber, Spievack and Wagner (52) U.S. Cl. .................. 604/20: 602/43: 602/48; 4771.5; Suite 2400, 420 Lexington Avenue 47/13 New York, NY 10170 (US) (57) ABSTRACT (21) Appl. No.: 12/231,104 A dressing having a flexible sleeve shaped to accommodate a Substantially cylindrical body portion, the sleeve having a (22) Filed: Aug. 29, 2008 lining which is substantially non-adherent to the body part being bandaged and having a peripheral securement means Related U.S. Application Data which attaches two peripheral portions to each other without (63) Continuation-in-part of application No. 1 1/434,689, those portions being circumferentially adhered to the sleeve filed on May 16, 2006. portion. Patent Application Publication Jan. 1, 2009 Sheet 1 of 9 US 2009/0005722 A1 Patent Application Publication Jan. 1, 2009 Sheet 2 of 9 US 2009/0005722 A1 10 8 F.G. 5 Patent Application Publication Jan. 1, 2009 Sheet 3 of 9 US 2009/0005722 A1 13 FIG.6 2 - Y TIII Till "T fift 11 10 FIG.7 8 13 6 - 12 - Timir" "in "in "MINIII. -
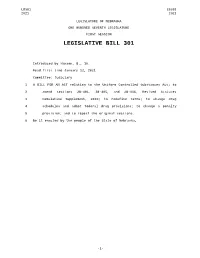
Introduced B.,Byhansen, 16
LB301 LB301 2021 2021 LEGISLATURE OF NEBRASKA ONE HUNDRED SEVENTH LEGISLATURE FIRST SESSION LEGISLATIVE BILL 301 Introduced by Hansen, B., 16. Read first time January 12, 2021 Committee: Judiciary 1 A BILL FOR AN ACT relating to the Uniform Controlled Substances Act; to 2 amend sections 28-401, 28-405, and 28-416, Revised Statutes 3 Cumulative Supplement, 2020; to redefine terms; to change drug 4 schedules and adopt federal drug provisions; to change a penalty 5 provision; and to repeal the original sections. 6 Be it enacted by the people of the State of Nebraska, -1- LB301 LB301 2021 2021 1 Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2 2020, is amended to read: 3 28-401 As used in the Uniform Controlled Substances Act, unless the 4 context otherwise requires: 5 (1) Administer means to directly apply a controlled substance by 6 injection, inhalation, ingestion, or any other means to the body of a 7 patient or research subject; 8 (2) Agent means an authorized person who acts on behalf of or at the 9 direction of another person but does not include a common or contract 10 carrier, public warehouse keeper, or employee of a carrier or warehouse 11 keeper; 12 (3) Administration means the Drug Enforcement Administration of the 13 United States Department of Justice; 14 (4) Controlled substance means a drug, biological, substance, or 15 immediate precursor in Schedules I through V of section 28-405. 16 Controlled substance does not include distilled spirits, wine, malt 17 beverages, tobacco, hemp, or any nonnarcotic substance if such substance 18 may, under the Federal Food, Drug, and Cosmetic Act, 21 U.S.C. -

BMJ Open Is Committed to Open Peer Review. As Part of This Commitment We Make the Peer Review History of Every Article We Publish Publicly Available
BMJ Open is committed to open peer review. As part of this commitment we make the peer review history of every article we publish publicly available. When an article is published we post the peer reviewers’ comments and the authors’ responses online. We also post the versions of the paper that were used during peer review. These are the versions that the peer review comments apply to. The versions of the paper that follow are the versions that were submitted during the peer review process. They are not the versions of record or the final published versions. They should not be cited or distributed as the published version of this manuscript. BMJ Open is an open access journal and the full, final, typeset and author-corrected version of record of the manuscript is available on our site with no access controls, subscription charges or pay-per-view fees (http://bmjopen.bmj.com). If you have any questions on BMJ Open’s open peer review process please email [email protected] BMJ Open Pediatric drug utilization in the Western Pacific region: Australia, Japan, South Korea, Hong Kong and Taiwan Journal: BMJ Open ManuscriptFor ID peerbmjopen-2019-032426 review only Article Type: Research Date Submitted by the 27-Jun-2019 Author: Complete List of Authors: Brauer, Ruth; University College London, Research Department of Practice and Policy, School of Pharmacy Wong, Ian; University College London, Research Department of Practice and Policy, School of Pharmacy; University of Hong Kong, Centre for Safe Medication Practice and Research, Department -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -

Fencamfamin Hydrochloride
2156 Stimulants and Anorectics Preparations recognised.1-3 Both reversible and irreversible cases have been reported and in some cases it has proved fatal.1,4-9 The condition BP 2008: Doxapram Injection; H appears to be linked to prolonged or repeated therapy.1,10 In 1992 USP 31: Doxapram Hydrochloride Injection. 1 N CH3 the UK CSM advised that treatment should not exceed 3 months Proprietary Preparations (details are given in Part 3) but later in 1997 it revised its recommendations for fenfluramine Austral.: Dopram†; Austria: Dopram; Belg.: Dopram; Denm.: Dopram; and dexfenfluramine allowing treatment for up to 12 months un- Fin.: Dopram; Fr.: Dopram; Ger.: Dopram; Gr.: Dopram; Hong Kong: der certain conditions.2 The CSM stated that treatment could be Dopram†; Irl.: Dopram; Neth.: Dopram; Norw.: Dopram; NZ: Dopram†; S.Afr.: Dopram; Spain: Docatone†; Switz.: Dopram†; UK: Dopram; continued beyond 3 months only if there had been a satisfactory USA: Dopram. response (more than 10% weight loss) and that this loss was maintained. Patients should also be monitored for symptoms of (fencamfamin) pulmonary hypertension. For other anorectics such as phenter- mine the maximum duration of treatment remained 3 months. Etamivan (BAN, rINN) ⊗ Profile However, shortly after this, a report was published11 that outlined Etamivaani; Étamivan; Etamiván; Etamivanum; Ethamivan (USAN); Fencamfamin hydrochloride has been given orally as a central an association between the use of a fenfluramine-phentermine NSC-406087; Vanillic Acid Diethylamide; Vanillic Diethylamide. stimulant. combination and the development of valvular heart disease in 24 patients. Initially, the response by the CSM was to advise against N,N-Diethylvanillamide. -

Laws 2021, LB236, § 4
LB236 LB236 2021 2021 LEGISLATIVE BILL 236 Approved by the Governor May 26, 2021 Introduced by Brewer, 43; Clements, 2; Erdman, 47; Slama, 1; Lindstrom, 18; Murman, 38; Halloran, 33; Hansen, B., 16; McDonnell, 5; Briese, 41; Lowe, 37; Groene, 42; Sanders, 45; Bostelman, 23; Albrecht, 17; Dorn, 30; Linehan, 39; Friesen, 34; Aguilar, 35; Gragert, 40; Kolterman, 24; Williams, 36; Brandt, 32. A BILL FOR AN ACT relating to law; to amend sections 28-1202 and 69-2436, Reissue Revised Statutes of Nebraska, and sections 28-401 and 28-405, Revised Statutes Cumulative Supplement, 2020; to redefine terms, change drug schedules, and adopt federal drug provisions under the Uniform Controlled Substances Act; to provide an exception to the offense of carrying a concealed weapon as prescribed; to define a term; to change provisions relating to renewal of a permit to carry a concealed handgun; to provide a duty for the Nebraska State Patrol; to eliminate an obsolete provision; to harmonize provisions; and to repeal the original sections. Be it enacted by the people of the State of Nebraska, Section 1. Section 28-401, Revised Statutes Cumulative Supplement, 2020, is amended to read: 28-401 As used in the Uniform Controlled Substances Act, unless the context otherwise requires: (1) Administer means to directly apply a controlled substance by injection, inhalation, ingestion, or any other means to the body of a patient or research subject; (2) Agent means an authorized person who acts on behalf of or at the direction of another person but does not include a common or contract carrier, public warehouse keeper, or employee of a carrier or warehouse keeper; (3) Administration means the Drug Enforcement Administration of the United States Department of Justice; (4) Controlled substance means a drug, biological, substance, or immediate precursor in Schedules I through V of section 28-405. -

Mechanisms of Cocaine Abuse and Toxicity
Mechanisms of Cocaine Abuse and Toxicity U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES • Public Health Service • Alcohol, Drug Abuse, and Mental Health Administration I Mechanisms of Cocaine Abuse and Toxicity Editors: Doris Clouet, Ph.D. Khursheed Asghar, Ph.D. Roger Brown, Ph.D. Division of Preclinical Research National Institute on Drug Abuse NIDA Research Monograph 88 1988 U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse 5600 Fishers Lane Rockville, MD 20857 For sale by the Superintendent of Documents, U.S. Government Printing Office Washington, DC 20402 NIDA Research Monographs are prepared by the research divisions of the National Institute on Drug Abuse and published by its Office of Science. The primary objective of the series is to provide critical reviews of research problem areas and techniques, the content of state-of-the-art conferences, and integrative research reviews. Its dual publication emphasis is rapid and targeted dissemination to the scientific and professional community. Editorial Advisors MARTIN W. ADLER, Ph.D. MARY L. JACOBSON Temple University School of Medicine National Federation of Parents for Philadelphia,Pennsylvania Drug-Free Youth Omaha, Nebraska SYDNEY ARCHER, Ph.D. Rensselaer Polytechnic lnstitute Troy, New York REESE T. JONES, M.D. Langley Porter Neuropsychiatric lnstitute RICHARD E. BELLEVILLE, Ph.D. San Francisco, California NB Associates, Health Sciences RockviIle, Maryland DENISE KANDEL, Ph.D. KARST J. BESTEMAN College of Physicians and Surgeons of Alcohol and Drug Problems Association Columbia University of North America New York, New York Washington, D.C. GILBERT J. -

2019 Prohibited List
THE WORLD ANTI-DOPING CODE INTERNATIONAL STANDARD PROHIBITED LIST JANUARY 2019 The official text of the Prohibited List shall be maintained by WADA and shall be published in English and French. In the event of any conflict between the English and French versions, the English version shall prevail. This List shall come into effect on 1 January 2019 SUBSTANCES & METHODS PROHIBITED AT ALL TIMES (IN- AND OUT-OF-COMPETITION) IN ACCORDANCE WITH ARTICLE 4.2.2 OF THE WORLD ANTI-DOPING CODE, ALL PROHIBITED SUBSTANCES SHALL BE CONSIDERED AS “SPECIFIED SUBSTANCES” EXCEPT SUBSTANCES IN CLASSES S1, S2, S4.4, S4.5, S6.A, AND PROHIBITED METHODS M1, M2 AND M3. PROHIBITED SUBSTANCES NON-APPROVED SUBSTANCES Mestanolone; S0 Mesterolone; Any pharmacological substance which is not Metandienone (17β-hydroxy-17α-methylandrosta-1,4-dien- addressed by any of the subsequent sections of the 3-one); List and with no current approval by any governmental Metenolone; regulatory health authority for human therapeutic use Methandriol; (e.g. drugs under pre-clinical or clinical development Methasterone (17β-hydroxy-2α,17α-dimethyl-5α- or discontinued, designer drugs, substances approved androstan-3-one); only for veterinary use) is prohibited at all times. Methyldienolone (17β-hydroxy-17α-methylestra-4,9-dien- 3-one); ANABOLIC AGENTS Methyl-1-testosterone (17β-hydroxy-17α-methyl-5α- S1 androst-1-en-3-one); Anabolic agents are prohibited. Methylnortestosterone (17β-hydroxy-17α-methylestr-4-en- 3-one); 1. ANABOLIC ANDROGENIC STEROIDS (AAS) Methyltestosterone; a. Exogenous* -

I (Acts Whose Publication Is Obligatory) COMMISSION
13.4.2002 EN Official Journal of the European Communities L 97/1 I (Acts whose publication is obligatory) COMMISSION REGULATION (EC) No 578/2002 of 20 March 2002 amending Annex I to Council Regulation (EEC) No 2658/87 on the tariff and statistical nomenclature and on the Common Customs Tariff THE COMMISSION OF THE EUROPEAN COMMUNITIES, Nomenclature in order to take into account the new scope of that heading. Having regard to the Treaty establishing the European Commu- nity, (4) Since more than 100 substances of Annex 3 to the Com- bined Nomenclature, currently classified elsewhere than within heading 2937, are transferred to heading 2937, it is appropriate to replace the said Annex with a new Annex. Having regard to Council Regulation (EEC) No 2658/87 of 23 July 1987 on the tariff and statistical nomenclature and on the Com- mon Customs Tariff (1), as last amended by Regulation (EC) No 2433/2001 (2), and in particular Article 9 thereof, (5) Annex I to Council regulation (EEC) No 2658/87 should therefore be amended accordingly. Whereas: (6) This measure does not involve any adjustment of duty rates. Furthermore, it does not involve either the deletion of sub- stances or addition of new substances to Annex 3 to the (1) Regulation (EEC) No 2658/87 established a goods nomen- Combined Nomenclature. clature, hereinafter called the ‘Combined Nomenclature’, to meet, at one and the same time, the requirements of the Common Customs Tariff, the external trade statistics of the Community and other Community policies concerning the (7) The measures provided for in this Regulation are in accor- importation or exportation of goods. -

Chapter 124 Controlled Substances
1 CONTROLLED SUBSTANCES, Ch 124 CHAPTER 124 CONTROLLED SUBSTANCES Referred to in §124B.2, 124C.1, 124E.12, 124E.16, 155A.3, 155A.6, 155A.6A, 155A.6B, 155A.12, 155A.13A, 155A.13C, 155A.17, 155A.17A, 155A.23, 155A.26, 155A.27, 155A.42, 189.16, 204.7, 204.8, 204.14, 204.15, 205.3, 205.11, 205.12, 205.13, 232.45, 232.52, 321.19, 321.215, 422.72, 462A.2, 702.6, 809A.21, 811.1, 811.2, 901.5, 914.7 See §205.11 – 205.13 for additional provisions relating to administration and enforcement This chapter not enacted as a part of this title; transferred from chapter 204 in Code 1993 SUBCHAPTER I 124.302 Registration requirements. 124.303 Registration. DEFINITIONS — CONTROLLED SUBSTANCES ADMINISTRATION — IMITATION CONTROLLED 124.304 Revocation, suspension, or SUBSTANCES restriction of registration. 124.305 Contested case proceedings. 124.101 Definitions. 124.306 Records of registrants. 124.101A Administration of controlled 124.307 Order forms. substances — delegation. 124.308 Prescriptions. 124.101B Factors indicating an imitation controlled substance. SUBCHAPTER IV OFFENSES AND PENALTIES SUBCHAPTER II STANDARDS AND SCHEDULES 124.401 Prohibited acts — manufacture, delivery, possession — 124.201 Duty to recommend changes counterfeit substances, in schedules — temporary simulated controlled amendments to schedules. substances, imitation 124.201A Cannabis-derived products — controlled substances — rules. penalties. 124.202 Controlled substances — listed 124.401A Enhanced penalty for regardless of name. manufacture or distribution 124.203 Substances listed in schedule I — to persons on certain real criteria. property. 124.204 Schedule I — substances 124.401B Possession of controlled included.