UPMC Telestroke Network Newsletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

University of Pittsburg Medical Center Acquisition of Western Maryland
Andrew N. Pollak, M.D. Ben Steffen CHAIR EXECUTIVE DIRECTOR MARYLAND HEALTH CARE COMMISSION 4160 PATTERSON AVENUE – BALTIMORE, MARYLAND 21215 TELEPHONE: 410-764-3460 FAX: 410-358-1236 January 29, 2020 Via E-Mail and USPS Howard L. Sollins, Esquire Baker Donelson 100 Light Street Baltimore, Maryland 21202 Re: Acquisition of Health Care Facilities: (1) Western Maryland Regional Medical Center 12500 Willowbrook Road Cumberland, Maryland 21502 (2) Western Maryland Health System Frostburg Nursing and Rehabilitation Center 48 Tarn Terrace Frostburg, Maryland 21532 (3) Western Maryland Health System Home Care 1050 West Industrial Boulevard, Suite 19 Cumberland, Maryland 21502 (4) Western Maryland Health System Hospice Services 1050 West Industrial Boulevard, Suite 19 Cumberland, Maryland 21502 Dear Mr. Sollins: I write in response to your letter of December 16, 2019, notifying the Maryland Health Care Commission (MHCC) of the intent of University of Pittsburgh Medical Center (UPMC) to become the sole member of Western Maryland Health System (WMHS) through an integration and affiliation agreement. This acquisition of WMHS will constitute the acquisition of four Maryland “health care facilities,” as that term is defined in Maryland Certificate of Need Law. Those facilities are: 1. Western Maryland Regional Medical Center, a general hospital, which operates a special rehabilitation hospital on its campus; 2. Western Maryland Health System Frostburg Nursing and Rehabilitation Center (FNRC), a comprehensive care facility or nursing home; TDD FOR DISABLED TOLL FREE MARYLAND RELAY SERVICE 1-877-245-1762 1-800-735-2258 Howard L. Sollins, Esquire January 29, 2020 Page 2 3. Western Maryland Health System Home Care, a home health agency, authorized to serve patients in Allegany and Garrett Counties; and 4. -

Highmark/Upmc Agreement Provider Q&A
HIGHMARK/UPMC AGREEMENT PROVIDER Q&A JULY 2019 Highmark and UPMC have agreed to a 10-year contract offering full in-network access for Highmark members in certain health products that include UPMC providers and facilities in their networks in the Pittsburgh and Erie areas. Below are some questions and answers about this agreement. Q. What does this agreement mean to community hospitals? A. Highmark Health is committed to its strategy of community-based, close-to-home care for its members and patients. Community hospitals will continue to play an important role in serving the needs of our members and patients going forward. A contract with UPMC does not change that. Q. What does this agreement mean for your patients right now? A. Commercial (non-ACA, non-MA) • In Western PA, commercial members in high-performing narrow network products such as Community Blue Flex or Connect Blue are in a high-quality, lower-cost plan. Members in these products will have access to some, but not all, UPMC facilities and doctors effective July 1, 2019. This is very similar to what they had before the negotiation of this new agreement. • Certain UPMC Providers will be in-network at the highest tier. These include: o UPMC Altoona o UPMC Bedford o UPMC Cole o UPMC Horizon (for Community Blue Flex, Horizon is moving from Standard to Enhanced tier) o UPMC Jameson (for Community Blue Flex, Jameson is moving from Standard to Enhanced tier) o UPMC Kane o UPMC Northwest o UPMC Somerset o Western Psychiatric Institute and Clinic of UPMC o UPMC physicians and ancillary providers affiliated with the hospitals listed above o Over 20 UPMC and Community Hospital Cancer Centers (e.g., Excela Arnold Palmer Cancer Center, St. -

UPMC Standard Network
UPMC Standard Network UPMC Health Plan participating hospitals for Effective February 2020 commercial employer group plans In-network hospitals and facilities Allegheny Bradford Elk Curahealth Pittsburgh Guthrie Towanda Memorial Penn Highlands Elk Heritage Valley Health System – Hospital Erie Heritage Valley Sewickley Robert Packer Hospital Corry Memorial Hospital LifeCare Behavioral Health Hospital of Troy Community Hospital Millcreek Community Hospital Pittsburgh Butler Select Specialty Hospital – Erie LifeCare Hospitals of Pittsburgh at Butler Memorial Hospital UPMC Hamot Main Campus UPMC Passavant – Cranberry Ohio Valley Hospital Fayette Select Specialty Hospital – McKeesport Cambria Highlands Hospital Select Specialty Hospital – Conemaugh Memorial Medical Center Uniontown Hospital Conemaugh Miners Medical Center Pittsburgh UPMC Greene St. Clair Hospital Select Specialty Hospital – Johnstown Washington Health System Greene The Children’s Home of Pittsburgh Chester The Children’s Institute of Pittsburgh Huntingdon Bryn Mawr Rehab Hospital Penn Highlands Huntingdon UPMC Children’s Hospital of Pittsburgh Paoli Hospital UPMC East Indiana UPMC Hillman Cancer Center Clarion Indiana Regional Medical Center Clarion Hospital UPMC Magee-Womens Hospital Jefferson UPMC McKeesport Clearfield Penn Highlands Brookville UPMC Mercy Penn Highlands Clearfield Punxsutawney Area Hospital UPMC Montefiore Penn Highlands DuBois Lancaster UPMC Passavant – McCandless Clinton UPMC Lititz UPMC Presbyterian UPMC Lock Haven UPMC St. Margaret Lawrence UPMC Shadyside Crawford UPMC Jameson UPMC Western Psychiatric Hospital Meadville Medical Center Lycoming Titusville Area Hospital Armstrong UPMC Muncy Armstrong County Memorial Hospital Cumberland UPMC Williamsport UPMC Carlisle UPMC Williamsport Divine Providence Beaver UPMC Pinnacle West Shore Campus Curahealth Hospital Heritage Valley Dauphin McKean Heritage Valley Health System – Penn State Health Children’s Hospital Bradford Regional Medical Center Heritage Valley Beaver Penn State Health Milton S. -

Acute-Care-Hospitals-Alphabetic.Pdf
Acute Care Hospitals Facility Name Facility # Facility Name Facility # Abington Health Center - Warminster 1410-09 Barnabas Health Jersey City Medical Center 2312-70 Campus(Warminster Hospital) Barnes-Kasson Hospital 1241-58 Abington Health-Lansdale Hospital 1432-46 Barnesville Hospital - Barnesville 1012-72 Abington Memorial Hospital 1001-46 Bath VA Medical Center 1062-71 Acuity Specialty Hospital of New Jersey (LTAC) 2310-70 (within Atlanticare Reg. Med.Ctr. Atlantic City Bayhealth Hospital, Sussex Campus 1012-68 Campu Bayshore Community Hospital 1039-70 AHN Harmar Neighborhood Hospital 1465-02 Beebe Medical Center - Lewes, DE 1003-68 AHN Hempfield Neighborhood Hospital 1130-65 Bellevue Hospital Center- New York, NY 1012-71 AHN McCandless Neighborhood Hospital 1464-02 Belmont Community Hospital (The Bellaire City 1002-72 AHN Neighborhood Hospital - Brentwood 1463-02 Hospital) Akron General Medical Center 1033-72 Belmont Hospital Bel Air 1026-72 Albany Medical Center Hospital - Albany, NY 1043-71 Benedictine Hospital 1001-71 Aliquippa Community Hospital (UPMC Beaver 1002-04 Berwick Hospital Center 1013-19 Valley Hospital) Beth Israel Hospital - Newark 1035-70 Allegheny General Hospital 1184-02 Beth Israel Med Ctr-Petrie Division (Manhattan) 1057-71 Allegheny Valley Hospital (Alle-Kiski Medical 1124-02 Center) Bloomsburg Hospital 1016-19 Anne Arundel Medical Center 1035-69 Bluefield Regional Medical Center 1029-73 Ardern Hill Hospital - Goshen 1017-71 Blythedale Children's Hospital 1063-71 Aria Health - Bucks County (formerly Delaware -

NOTICES DEPARTMENT of AGRICULTURE Article I
2494 NOTICES DEPARTMENT OF AGRICULTURE Article I. General Provisions and Definitions. (a) Purpose of the Program. The purpose of this pro- Pennsylvania Certified Hemp Sampling Program; gram is as follows: General Standards and Requirements for Penn- (1) To establish provisions under which persons may sylvania Certified Hemp Sampling Agents apply to become certified by the Department to take official hemp samples and be recognized as Certified Recitals. Hemp Sampling Agents by the Department. A. The Act relating to Controlled Plants and Noxious (2) To establish hemp sampling procedures and re- Weeds (‘‘Act’’) (3 Pa.C.S.A. § 1501 et seq.) authorizes quirements. the Department of Agriculture (Department) through (3) To establish procedures and requirements for docu- the Controlled Plant and Noxious Weed Committee (Com- mentation and reporting by Certified Hemp Sampling mittee) to establish a controlled plant list and to add Agents to the Department. plants to or remove plants from the controlled plant list (3 Pa.C.S.A. § 1511(b)(3)(ii)(iii)). (4) To establish procedures for Department oversight of Certified Hemp Sampling Agents and for denial, revoca- B. The Act provides for publication of the noxious weed tion, or suspension of Hemp Sampling Agent certification. and the controlled plant list and additions or removals or changes thereto to be published as a notice in the (b) Definitions. Pennsylvania Bulletin and for such additions or removals Act. The act of October 30, 2017, P.L. 774, No. 46, at to become effective sixty (60) days from publication 3 Pa.C.S.A. §§ 1501—1562, related to controlled plants (3 Pa.C.S.A. -
Ready; Comprehensive Stroke Center
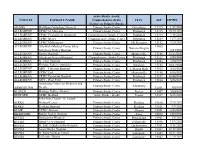
Acute Stroke -ready; COUNTY FACILITY NAME Comprehensive stroke CITY ZIP EXPIRES Center; or Primary Stroke ADAMS WellSpan Gettysburg Hospital Primary Stroke Center Gettysburg 17325 1/22/2024 ALLEGHENY UPMC St. Margaret Primary Stroke Center Pittsburgh 15215 10/20/2022 ALLEGHENY UPMC Presbyterian Shadyside Comprehensive Stroke Center Pittsburgh 15213 7/18/2021 ALLEGHENY UPMC Mercy Comprehensive Stroke Center Pittsburgh 15219 12/7/2021 ALLEGHENY UPMC McKeesport Primary Stroke Center Mc Keesport 15132 7/20/2021 ALLEGHENY Alle-Kiski Medical Center d/b/a/ 15065 Primary Stroke Center Natrona Heights Allegheny Valley Hospital 3/14/2021 ALLEGHENY Forbes Hospital Primary Stroke Center Monroeville 15146 11/17/2022 ALLEGHENY Allegheny General Hospital Comprehensive Stroke Center Pittsburgh 15212 3/20/2021 ALLEGHENY St. Clair Hospital Primary Stroke Center Pittsburgh 15243 2/24/2023 ALLEGHENY Heritage Valley - Swickley Primary Stroke Center Swickley 15143 10/17/2021 ALLEGHENY AHN - Jefferson Hospital Primary Stroke Center Jefferson Hills 15025 3/13/2023 ALLEGHENY UPMC East Primary Stroke Center Monroeville 15146 6/16/2023 ALLEGHENY UPMC Passavant Hospital Primary Stroke Center Pittsburgh 15237 10/28/2022 ALLEGHENY AHN - West Penn Primary Stroke Center Pittsburgh 15224 5/26/2021 Armstrong Center for Medicine and Primary Stroke Center Kittanning ARMSTRONG Health 16201 3/8/2022 BEAVER Heritage Valley - Beaver Primary Stroke Center Beaver 15009 10/4/2021 BEDFORD UPMC Bedford Acute Stroke - Ready Everett 15537 6/25/2021 Penn State Health - St. Joseph BERKS Medical Center Primary Stroke Center Reading 19610 7/24/2022 BERKS Reading Hospital Primary Stroke Center Reading 19611 9/9/2021 BLAIR UPMC Altoona Primary Stroke Center Altoona 16601 5/15/2023 BRADFORD Robert Packer Hospital Primary Stroke Center Sayre 18840 12/5/2022 BUCKS Doylestown Hospital Primary Stroke Center Doylestown 18901 3/5/2021 BUCKS Grand View Hospital Primary Stroke Center Sellersville 18960 11/4/2022 BUCKS St. -

The Relationship Between UPMC and Highmark Is Changing
The relationship between UPMC and Highmark is changing. After June 30, 2019, many UPMC hospitals and other facilities in western Pennsylvania will be out-of-network for patients with Highmark commercial insurance. Below are answers to frequently asked questions about how these changes may impact your health care. Q: Will UPMC Somerset be out-of-network after June 30, 2019? Network status of UPMC hospitals A: No. UPMC Somerset will remain in-network for most Highmark in western Pennsylvania after June 30, 2019 commercial members after June 30, 2019. Out-of- Hospital/Facility Name In-Network* Q: Do all Highmark plans provide full, in-network access to Network UPMC Somerset? UPMC Altoona ü A: No. My Direct Blue, a plan offered on the Affordable Care Act’s insurance exchange, is considered out-of-network for all UPMC UPMC Bedford ü physicians and hospitals except UPMC Children’s Hospital of UPMC Children’s Hospital Pittsburgh and its physicians. of Pittsburgh ü Q: Will UPMC doctors be out-of-network after June 30, 2019? UPMC East û If you would like to see a doctor at or near a UPMC hospital or facility A: UPMC Hamot that will be in-network for you after June 30, 2019, such as UPMC û Somerset, you can expect that doctor to be in-network as well. UPMC Horizon (both campuses) ü If you would like to see a doctor at or near a UPMC hospital or facility UPMC Jameson that will be out-of-network for you after June 30, 2019, such as UPMC ü Passavant, you can expect that doctor to be out-of-network as well. -

There's a Plan in Here with All Over
There’s a plan in here with your name all over it. Your guide to finding just the right Individual or Family plan for you. For Benefit Period: January 1 to December 31, 2021 Plans may be offered by Highmark Blue Cross Blue Shield, Highmark Health Insurance Company, or Highmark Coverage Advantage. Go ahead. Get picky about your plan. With lots of great coverage options from Highmark, this book will help you find the plan, the product, and the network access that matters most to you. Looking for something in particular? You can easily navigate through the guide by clicking on the headings in the Table of Contents. Why choose Highmark? . 1 Affordable Care Act basics ������������������������������������������������������������������������������6 Financial help info ����������������������������������������������������������������������������������������������8 Enrollment dates ���������������������������������������������������������������������������������������������� 10 Enrollment checklist ����������������������������������������������������������������������������������������� 11 Product and network highlights ���������������������������������������������������������������������12 Plan details by county . 26 Helpful health insurance definitions ������������������������������������������������������������ 41 Legal info ���������������������������������������������������������������������������������������������������������� 42 Why choose a Highmark health plan? Woah. So many reasons. Here are three big ones right off the top of our heads. -

COVID-19 Labs.Pdf
Labs Name TestName FacilityAddress A2Z Diagnostics, LLC COVID-19 6 Industrial Way West, Suite F19 Eatontown , NJ 07724 Abington Memorial Hospital COVID-19 1200 Old York Road Abington, PA 19001 Absolute Genomics COVID-19 1300 Old Plank Rd., Suite 400 Mayfield, PA 18433 Access Dx Laboratory, LLC COVID-19 8920 Kirby Dr. Houston, TX 77054 Access Medical Laboratories COVID-19 5151 Corporate Way Jupiter, FL 33458 Accu Reference Medical Laboratory COVID-19 1901 East Linden Avenue Suite 4 Linden, NJ 07036 Accurate Diagnostic Labs, Inc. COVID-19 3000 Hadley Road South Plainfield, NJ 07080 ACMH Hospital Laboratory COVID-19 One Nolte Drive Kittanning, PA 16201 ACULABS INC COVID-19 2 KENNEDY BOULEVARD 3RD FLOOR EAST BRUNSWICK, NJ 08816 ACUPATH LABORATORIES INC COVID-19 28 SOUTH TERMINAL DRIVE PLAINVIEW, NY 11803 Acutis Diagnostics COVID-19 400 Karin Lane Hicksville, NY 11801 Adaptive Biotechnologies Corporation COVID-19 1551 Eastlake Avenue East, Suite 200 Seattle, WA 98102 AdvaGenix COVID-19 9430 Key West Hwy, Suite 130 Rockville, MD 20850 Advaite, Inc COVID-19 365 Phoenixville Pike Malvern, PA 19355 Advanced Diagnostic Laboratory COVID-19 1077 Central Parkway S Suite 200 San Antonio, TX 78232 Advanced Lab Solutions LLC COVID-19 3729 Easton Nazareth Hwy L2 Easton, PA 18045 Aegis Sciences Corporation COVID-19 501 Great Circle Road Nashville, TN 37228 Akesogen COVID-19 3155 Northwoods Place Norcross, GA 30071 Albert Einstein Medical Center North COVID-19 5501 Old York Road Philadelphia, PA 18141 ALLEG COUNTY HEALTH DEPARTMENT COVID-19 3901 Penn Avenue Building 8 Pittsburgh, PA 15224 ALLEGHENY GENERAL HOSP DEPT OF LAB MED COVID-19 320 E NORTH AVENUE PITTSBURGH, PA 15212 ALLEGHENY GENERAL HOSPITAL LAB COVID-19 1307 FEDERAL STREET Pittsburgh, PA 15212 ALLE-KISKI MD CTR DBA AVH COVID-19 1301 CARLISLE STREET NATRONA HEIGHTS, PA 15065 Alliance Laboratories COVID-19 3611 14th Avenue Ste 102 Brooklyn, NY 11218 Allora Laboratory, LLC COVID-19 405 St. -

University of Pittsburgh Writing Style Manual
Writing Style Manual THIRD EDITION The University of Pittsburgh, as an educational institution and as an employer, values equality of opportunity, human dignity, and racial/ethnic and cultural diversity. Accordingly, as fully explained in Policy 07-01-03, the University prohibits and will not engage in discrimination or harassment on the basis of race, color, religion, national origin, ancestry, sex, age, marital status, familial status, sexual orientation, gender identity and expression, genetic information, disability, or status as a veteran. The University also prohibits and will not engage in retaliation against any person who makes a claim of discrimination or harassment or who provides information in such an investigation. Further, the University will continue to take afrmative steps to support and advance these values consistent with the University’s mission. This policy applies to admissions, employment, and access to and treatment in University programs and activities*. This is a commitment made by the University and is in accordance with federal, state, and/or local laws and regulations. For information on University equal opportunity and afrmative action programs, please contact: University of Pittsburgh; Ofce of Diversity and Inclusion; Katie Pope, Title IX Coordinator, and Cheryl Rufn, 504 and ADA Coordinator; Second Floor, Webster Hall; 4415 Fifth Avenue; Pittsburgh, PA 15260; 412-648-7860. For complete details on the University’s Nondiscrimination Policy, please refer to Policy 07-01-03. For information on how to fle a complaint under this policy, please refer to Procedure 07-01-03. *Except where exempt by federal or state laws. The University of Pittsburgh is an afrmative action, equal opportunity institution. -

UPMC Inside Advantage Network Listing
UPMC Inside Advantage Network listing of UPMC Health Plan participating Effective March 2021 hospitals for commercial employer group plans Level 1 Hospitals and Facilities Lycoming Level 2 Hospitals and Facilities UPMC Muncy Allegheny Allegheny UPMC Williamsport Curahealth Pittsburgh Heritage Valley Health System – UPMC Williamsport Divine Select Specialty Hospital – McKeesport Heritage Valley Kennedy Providence Campus Select Specialty Hospital – Heritage Valley Health System – Pittsburgh UPMC McKean Heritage Valley Sewickley UPMC Children’s Hospital of Pittsburgh Bradford Regional Medical Center Jefferson Hospital UPMC East UPMC Kane LifeCare Behavioral Health Hospital of UPMC Hillman Cancer Center Pittsburgh Mercer UPMC Magee-Womens Hospital Grove City Medical Center LifeCare Hospitals of Pittsburgh at UPMC McKeesport UPMC Horizon – Greenville Main Campus UPMC Mercy UPMC Horizon – Shenango Valley St. Clair Hospital UPMC Montefiore The Children’s Home of Pittsburgh UPMC Passavant – McCandless Potter The Children’s Institute UPMC Presbyterian UPMC Cole Armstrong UPMC St. Margaret Somerset Armstrong County Memorial UPMC Shadyside UPMC Somerset Hospital UPMC Western Psychiatric Hospital Tioga Beaver Bedford UPMC Wellsboro Curahealth Hospital Heritage Valley UPMC Bedford Memorial Venango Heritage Valley Health System – Blair UPMC Northwest Heritage Valley Beaver UPMC Altoona Warren Berks Butler Warren General Hospital Penn State Health St. Joseph UPMC Passavant – Cranberry Reading Hospital Westmoreland Surgical Institute of Reading Cambria -

Honors Awards
AWARDS Pam Cupec, MS, RN, ONC, CRRN, ACM – Outstanding Award for Commitment and Excellence in Service Contribution to NAON – award from the National (ACES) Association of Orthopaedic Nurses Patricia Hurley, RN Cassandra McClelleand, RN James Hennigan, MSSL, BS, RN – scholarship from the Marissa McWhirthe, RN Nightingale Awards of Pennsylvania Carrie Miller, RN, CPN Jennifer Hicks, MSN, RN – 2020 Richard L. Simmons, MD, Maureen Pentz, RN, CCM Speak Up for Safety Award Kelly Schneiderlochner, RN, CCRN Christi Sylvester, CRNP, MSN Sheryl Lynch, RN – 2020 Richard L. Simmons, MD, Susan Wesner, RN, MSN, CS Speak Up for Safety Award Rose Margiotta, RN – 2020 Richard L. Simmons, MD, Cameos of Caring® (presented by the Speak Up for Safety Award University of Pittsburgh School of Nursing) Christie Santure, BSN, RN, OCN, UPMC Hillman Cancer Honorees Center - one of the three finalists for the Extraordinary Healer Award for Oncology Nursing presented by Andrea Alfano CURE® magazine. Salvator Mundi Rhonda Sebastian, MSN, RN, CNOR, OR Excellence Abby Arthur Award in Patient Safety from Outpatient UPMC Altoona Surgery Magazine. Melanie Augustine Jennifer Shaffer, RN – Neonatal Abstinence Syndrome UPMC Horizon Quality Improvement (Sub-award, $15,000). Shannon Casey Pennsylvania Perinatal Quality Collaborative UPMC Center for Nursing Excellence UPMC Hamot Emergency Department received the 2020 Catherine S. Cannon ENA (Emergency Nurses Association) Lantern Award UPMC Western Psychiatric Hospital UPMC Hamot Endoscopy Unit – designated an ASGE Amber N. Cole Center of Excellence by the American Society for UPMC St. Margaret Gastrointestinal Endoscopy Gillian M. Covert UPMC Passavant Cardiovascular ICU – American UPMC Pinnacle, Wound & Hyperbaric Centers Association of Critical Care Gold Nurses Beacon Award of Excellence™ Janet Dye UPMC East UPMC Presbyterian Cardiothoracic ICU – American Association of Critical-Care Silver Nurses Beacon Award Amy Folk of Excellence™ UPMC Shadyside UPMC St.