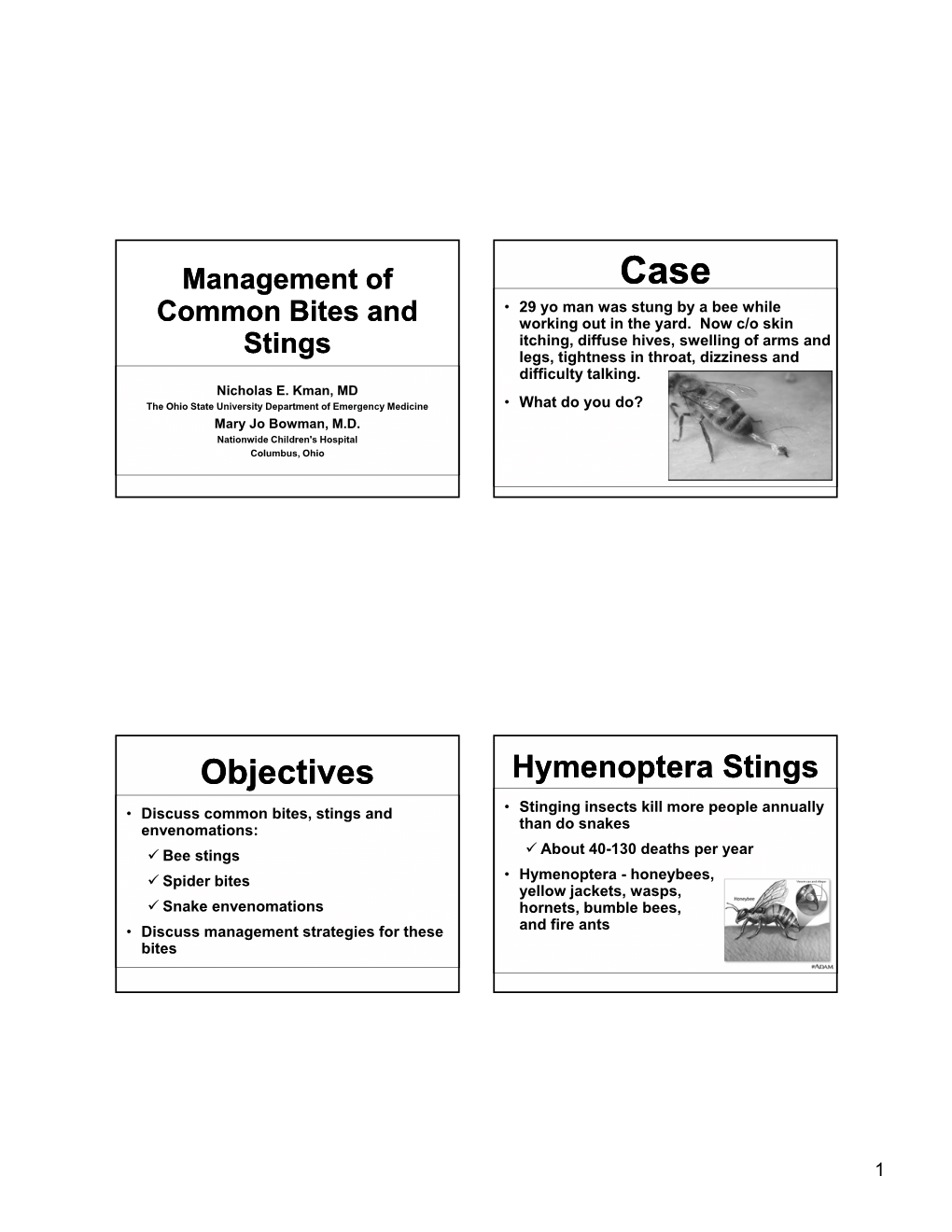
Objectives Hymenoptera Stings
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Rachel Carson for SILENT SPRING
Silent Spring THE EXPLOSIVE BESTSELLER THE WHOLE WORLD IS TALKING ABOUT RACHEL CARSON Author of THE SEA AROUND US SILENT SPRING, winner of 8 awards*, is the history making bestseller that stunned the world with its terrifying revelation about our contaminated planet. No science- fiction nightmare can equal the power of this authentic and chilling portrait of the un-seen destroyers which have already begun to change the shape of life as we know it. “Silent Spring is a devastating attack on human carelessness, greed and irresponsibility. It should be read by every American who does not want it to be the epitaph of a world not very far beyond us in time.” --- Saturday Review *Awards received by Rachel Carson for SI LENT SPRING: • The Schweitzer Medal (Animal Welfare Institute) • The Constance Lindsay Skinner Achievement Award for merit in the realm of books (Women’s National Book Association) • Award for Distinguished Service (New England Outdoor Writers Association) • Conservation Award for 1962 (Rod and Gun Editors of Metropolitan Manhattan) • Conservationist of the Year (National Wildlife Federation) • 1963 Achievement Award (Albert Einstein College of Medicine --- Women’s Division) • Annual Founders Award (Isaak Walton League) • Citation (International and U.S. Councils of Women) Silent Spring ( By Rachel Carson ) • “I recommend SILENT SPRING above all other books.” --- N. J. Berrill author of MAN’S EMERGING MIND • "Certain to be history-making in its influence upon thought and public policy all over the world." --Book-of-the-Month Club News • "Miss Carson is a scientist and is not given to tossing serious charges around carelessly. -

Medical Problems and Treatment Considerations for the Red Imported Fire Ant
MEDICAL PROBLEMS AND TREATMENT CONSIDERATIONS FOR THE RED IMPORTED FIRE ANT Bastiaan M. Drees, Professor and Extension Entomologist DISCLAIMER: This fact sheet provides a review of information gathered regarding medical aspects of the red imported fire ant. As such, this fact sheet is not intended to provide treatment recommendations for fire ant stings or reactions that may develop as a result of a stinging incident. Readers are encouraged to seek health-related advice and recommendations from their medical doctors, allergists or other appropriate specialists. Imported fire ants, which include the red imported fire ant - Solenopsis invicta Buren (Hymenoptera: Formicidae), the black imported fire ant - Solenopsis richteri Forel and the hybrid between S. invicta and S. richteri, cause medical problems when sterile female worker ants from a colony sting and inject a venom that cause localized sterile blisters, whole body allergic reactions such as anaphylactic shock and occasionally death. In Texas, S. invicta is the only imported fire ant, although several species of native fire ants occur in the state such as the tropical fire ant, S. geminata (Fabricius), and the desert fire ant, S. xyloni McCook, which are also capable of stinging (see FAPFS010 and 013 for identification keys). Over 40 million people live in areas infested by the red imported fire ant in the southeastern United States. An estimated 14 million people are stung annually. According to The Scripps Howard Texas Poll (March 2000), 79 percent of Texans have been stung by fire ants in the year of the survey, while 20% of Texans report not ever having been stung. -
The Venom Produced by Different Classes of Arthropods and Uses It As a Biological Control Agent
Archive of SID The venom produced by different classes of arthropods and uses it as a biological control agent Kabir Eyidozehi1, Sultan Ravan2 1Ph.D. student of Agricultural Entomology, University of Zabol, Iran 2 Associate Professor Plant Protection Department, University of Zabol, Iran (Corresponding Author: Kabir Eyidozehi) Abstract Animal kingdom possesses numerous poisonous species that produce venoms or toxins. The biodiversity of venoms and toxins made it a unique source of leads and structural templates from which new therapeutic agents may be developed. Such richness can be useful to biotechnology and/or pharmacology in many ways, with the prospection of new toxins in this field. Venoms of several animal species such as snakes, scorpions, toads, frogs and their active components have shown potential biotechnological applications. Recently, using molecular biology techniques and advanced methods of fractionation, researchers have obtained different native and/or recombinant toxins and enough material to afford deeper insight into the molecular action of these toxins. Now a day to visualize the boundaries between cancerous tissues and normal tissues florescent labeled scorpion venom peptides are used. Still a lot of peptides in scorpion venom are not identified. Further studies are needed to identify therapeutically crucial peptides in scorpion venom. This paper reviews the knowledge about the various aspects related to the name, biological and medical importance of poisonous animals of different major animal phyla. Key words: Poisonous animals, Scorpion, Spider, Venoms, Insects www.SID.ir Archive of SID INTRODUCTION 1. The biological and medical significance of poisonous animals Animal venoms and toxins are now recognized as major sources of bioactive molecules that may be tomorrow’s new drug leads. -
Why Do We Study Animal Toxins?
ZOOLOGICAL RESEARCH Why do we study animal toxins? Yun ZHANG* Key Laboratory of Animal Models and Human Disease Mechanisms of The Chinese Academy of Sciences & Yunnan Province, Kunming Institute of Zoology, Chinese Academy of Sciences, Kunming Yunnan 650223, China ABSTRACT Biological roles of venoms........................................................................(187) Predation.....................................................................................................(187) Defense .......................................................................................................(187) Venom (toxins) is an important trait evolved along Competition ................................................................................................(188) the evolutionary tree of animals. Our knowledges on Antimicrobial defense ................................................................................(188) venoms, such as their origins and loss, the biological Communication ..........................................................................................(188) relevance and the coevolutionary patterns with other Venom loss..................................................................................................(188) Toxins in animal venoms..........................................................................(188) organisms are greatly helpful in understanding many Selection pressures and animal toxins........................................................(188) fundamental biological questions, i.e., -

Evolução Do Veneno Em Cnidários Baseada Em Dados De Genomas E Proteomas
Adrian Jose Jaimes Becerra Evolução do veneno em cnidários baseada em dados de genomas e proteomas Venom evolution in cnidarians based on genomes and proteomes data São Paulo 2015 i Adrian Jose Jaimes Becerra Evolução do veneno em cnidários baseada em dados de genomas e proteomas Venom evolution in cnidarians based on genomes and proteomes data Dissertação apresentada ao Instituto de Biociências da Universidade de São Paulo, para a obtenção de Título de Mestre em Ciências, na Área de Zoologia. Orientador: Prof. Dr. Antonio C. Marques São Paulo 2015 ii Jaimes-Becerra, Adrian J. Evolução do veneno em cnidários baseada em dados de genomas e proteomas. 103 + VI páginas Dissertação (Mestrado) - Instituto de Biociências da Universidade de São Paulo. Departamento de Zoologia. 1. Veneno; 2. Evolução; 3. Proteoma. 4. Genoma I. Universidade de São Paulo. Instituto de Biociências. Departamento de Zoologia. Comissão Julgadora Prof(a) Dr(a) Prof(a) Dr(a) Prof. Dr. Antonio Carlos Marques iii Agradecimentos Eu gostaria de agradecer ao meu orientador Antonio C. Marques, pela confiança desde o primeiro dia e pela ajuda tanto pessoal como profissional durantes os dois anos de mestrado. Obrigado por todo. Ao CAPES, pela bolsa de mestrado concedida. Ao FAPESP pelo apoio financeiro durante minha estadia em Londres. Ao Instituto de Biociências da Universidade de São Paulo, pela estrutura oferecida durante a execução desde estudo. Ao Dr. Paul F. Long pelas conversas, por toda sua ajuda, por acreditar no meu trabalho. Aos colegas e amigos de Laboratório de Evolução Marinha (LEM), Jimena Garcia, María Mendoza, Thaís Miranda, Amanda Cunha, Karla Paresque, Marina Fernández, Fernanda Miyamura e Lucília Miranda, pela amizade, dicas e ajuda em tudo e por me fazer sentir em casa, muito obrigado mesmo! Aos meus amigos fora do laboratório, John, Soly, Chucho, Camila, Faride, Cesar, Angela, Camilo, Isa, Nathalia, Susana e Steffania, pelo apoio e por me fazer sentir em casa. -

HERO Bestiary 1 HERO Bestiaryª
HERO Bestiary 1 HERO Bestiary™ CREDITS Author: Doug Tabb Contributing Authors: Darrin C. Zielinski, Brian Nystul, Mark Bennett Editors: George MacDonald, Steve Peterson, and Coleman Charlton Cover Illustration: Storn Cook Colorist: Frank Cirocco Interior Illustration: Storn Cook, Stephan Peregrine, Mitch Byrd, Paul Jaquays, Liz Danforth, Albert Deschesne, Dennis Loubet, Luther, Elissa Martin, Darrell Midgette, Giorgia Ponticelli, Roger Raupp, Paulo Romano, Shawn Sharp, Jason Waltrip. A bibliography for the Dover Publication art and copyright free art used in this product can be found on the last page. Project Specific Contributions: Pagemaking & Layout: Coleman Charlton; Cover Graphics: Terry K. Amthor; Art Direction: Jessica Ney; Editorial Contributions: Ray Greer, Monte Cook Proofreading: Lori Ralston Dedication: To Gary Gygax who gave me role-playing games; to George MacDonald and Steve Peterson who gave me the rules; to Rob Bell who gave me a chance; to Ray Greer who treated me like a real human being; and to Jim, my long time collaborator. ICE Staff — Sales Manager: Deane Begiebing; Editing & Development Manager: Coleman Charlton; President: Peter Fenlon; CEO: Bruce Neidlinger; Editing, Development, & Production Staff: Kevin Barrett, Monte Cook, Jessica Ney, Pete Fenlon, Terry Amthor; Sales, Customer Service & Operations Staff: Heike Kubasch, Chad McCully; Shipping Staff: John Breckenridge, Jasper Merendino, Sterling Williams. HERO Bestiary™ is Hero Games’ trademark for its superhero roleplaying game using the Hero system. Champions® and Champions, The Super Roleplaying Game™ are Hero Games trademarks for its superhero roleplaying game using the Hero System. Hero System™ is Hero Games’ trademark for its roleplaying system. HERO Bestiary Copyright © 1992 Hero Games. All rights reserved. -
PRICK TESTING in INSECT BITE REACTION Dissertation Submitted
PRICK TESTING IN INSECT BITE REACTION Dissertation submitted to The Tamil Nadu Dr. M.G.R Medical University, Chennai In fulfilment of the requirements for the award of the degree of Doctor of Medicine in Dermatology, Venereology and Leprology Under the guidance of Dr. SHANMUGA SEKAR .C, MD., Department of Dermatology, Venereology and Leprology PSG INSTITUTE OF MEDICAL SCIENCES & RESEARCH, COIMBATORE THE TAMILNADU DR. M.G.R MEDICAL UNIVERSITY, CHENNAI, TAMILNADU MAY 2018 CERTIFICATE This is to certify that the thesis entitled “PRICK TESTING IN INSECT BITE REACTION” is a bonafide work of Dr. IYSHWARIYA SIVADASAN done under the direct guidance and supervision of Dr.C.R. SRINIVAS, MD and Dr. SHANMUGA SEKAR .C, MD, in the department of Dermatology, Venereology and Leprology, PSG Institute of Medical Sciences and Research, Coimbatore in fulfillment of the regulations of The Tamil Nadu Dr.MGR Medical University for the award of MD degree in Dermatology, Venereology and Leprology. Dr. REENA RAI Dr. RAMALINGAM Professor & Head of Department DEAN Department of DVL DECLARATION I hereby declare that this dissertation entitled “PRICK TESTING IN INSECT BITE REACTION” was prepared by me under the direct guidance and supervision of Dr.C.R.SRINIVAS, MD and Dr. SHANMUGA SEKAR C., MD, PSG Institute of Medical Sciences and Research, Coimbatore. The dissertation is submitted to The Tamil Nadu Dr. MGR Medical University in fulfillment of the University regulation for the award of MD degree in Dermatology, Venereology and Leprology. This dissertation has not been submitted for the award of any other Degree or Diploma. Dr. IYSHWARIYA SIVADASAN CERTIFICATE BY THE GUIDE This is to certify that the thesis entitled “PRICK TESTING IN INSECT BITE REACTION” is a bonafide work of Dr. -

Table I. Genodermatoses with Known Gene Defects 92 Pulkkinen
92 Pulkkinen, Ringpfeil, and Uitto JAM ACAD DERMATOL JULY 2002 Table I. Genodermatoses with known gene defects Reference Disease Mutated gene* Affected protein/function No.† Epidermal fragility disorders DEB COL7A1 Type VII collagen 6 Junctional EB LAMA3, LAMB3, ␣3, 3, and ␥2 chains of laminin 5, 6 LAMC2, COL17A1 type XVII collagen EB with pyloric atresia ITGA6, ITGB4 ␣64 Integrin 6 EB with muscular dystrophy PLEC1 Plectin 6 EB simplex KRT5, KRT14 Keratins 5 and 14 46 Ectodermal dysplasia with skin fragility PKP1 Plakophilin 1 47 Hailey-Hailey disease ATP2C1 ATP-dependent calcium transporter 13 Keratinization disorders Epidermolytic hyperkeratosis KRT1, KRT10 Keratins 1 and 10 46 Ichthyosis hystrix KRT1 Keratin 1 48 Epidermolytic PPK KRT9 Keratin 9 46 Nonepidermolytic PPK KRT1, KRT16 Keratins 1 and 16 46 Ichthyosis bullosa of Siemens KRT2e Keratin 2e 46 Pachyonychia congenita, types 1 and 2 KRT6a, KRT6b, KRT16, Keratins 6a, 6b, 16, and 17 46 KRT17 White sponge naevus KRT4, KRT13 Keratins 4 and 13 46 X-linked recessive ichthyosis STS Steroid sulfatase 49 Lamellar ichthyosis TGM1 Transglutaminase 1 50 Mutilating keratoderma with ichthyosis LOR Loricrin 10 Vohwinkel’s syndrome GJB2 Connexin 26 12 PPK with deafness GJB2 Connexin 26 12 Erythrokeratodermia variabilis GJB3, GJB4 Connexins 31 and 30.3 12 Darier disease ATP2A2 ATP-dependent calcium 14 transporter Striate PPK DSP, DSG1 Desmoplakin, desmoglein 1 51, 52 Conradi-Hu¨nermann-Happle syndrome EBP Delta 8-delta 7 sterol isomerase 53 (emopamil binding protein) Mal de Meleda ARS SLURP-1 -

Adverse Reactions to Ants Other Than Imported Fire Ants John H
Adverse reactions to ants other than imported fire ants John H. Klotz, PhD*; Richard D. deShazo, MD†; Jacob L. Pinnas, MD‡; Austin M. Frishman, PhD§; Justin O. Schmidt, PhD¶; Daniel R. Suiter, PhDʈ; Gary W. Price, MD**; and Stephen A. Klotz, MD‡ Objective: To identify ants other than Solenopsis invicta and Solenopsis richteri reported to cause adverse reactions in humans. Data Sources: We conducted a literature review to identify reports of medical reactions to ants other than S invicta and S richteri. Our review of medical and entomological literature on stinging ants was generated from MEDLINE and FORMIS, respectively, using the key words stinging ants and ant stings. The search was limited to articles in English published from 1966 to 2004 on MEDLINE and all years on FORMIS. We also present 3 new case reports of severe reactions to stings by 2 different species of ants, Pseudomyrmex ejectus and Hypoponera punctatissima. Study Selection: Articles that concerned anaphylactic (IgE-mediated) or anaphylactic-like (resembling anaphylaxis but mechanism unknown) immediate reactions to ant stings or bites were included in this review. Results: Taken together, our data demonstrate that S invicta and S richteri are not alone in their capability to cause serious allergic or adverse reactions. A diverse array of ant species belonging to 6 different subfamilies (Formicinae, Myrmeciinae, Ponerinae, Ectatomminae, Myrmicinae, and Pseudomyrmecinae) and 10 genera (Solenopsis, Formica, Myrmecia, Tetramorium, Pogonomyrmex, Pachycondyla, Odontomachus, Rhytidoponera, Pseudomyrmex, and Hypoponera) have now been shown to have this capability. Conclusion: Awareness that species other than imported fire ants may cause severe reactions should lead to more rapid evaluation and treatment and further investigation of the medical entomology of these ants. -

The Insect Sting Pain Scale: How the Pain and Lethality of Ant, Wasp, and Bee Venoms Can Guide the Way for Human Benefit
Preprints (www.preprints.org) | NOT PEER-REVIEWED | Posted: 27 May 2019 1 (Article): Special Issue: "Arthropod Venom Components and their Potential Usage" 2 The Insect Sting Pain Scale: How the Pain and Lethality of Ant, 3 Wasp, and Bee Venoms Can Guide the Way for Human Benefit 4 Justin O. Schmidt 5 Southwestern Biological Institute, 1961 W. Brichta Dr., Tucson, AZ 85745, USA 6 Correspondence: [email protected]; Tel.: 1-520-884-9345 7 Received: date; Accepted: date; Published: date 8 9 Abstract: Pain is a natural bioassay for detecting and quantifying biological activities of venoms. The 10 painfulness of stings delivered by ants, wasps, and bees can be easily measured in the field or lab using the 11 stinging insect pain scale that rates the pain intensity from 1 to 4, with 1 being minor pain, and 4 being extreme, 12 debilitating, excruciating pain. The painfulness of stings of 96 species of stinging insects and the lethalities of 13 the venoms of 90 species was determined and utilized for pinpointing future promising directions for 14 investigating venoms having pharmaceutically active principles that could benefit humanity. The findings 15 suggest several under- or unexplored insect venoms worthy of future investigations, including: those that have 16 exceedingly painful venoms, yet with extremely low lethality – tarantula hawk wasps (Pepsis) and velvet ants 17 (Mutillidae); those that have extremely lethal venoms, yet induce very little pain – the ants, Daceton and 18 Tetraponera; and those that have venomous stings and are both painful and lethal – the ants Pogonomyrmex, 19 Paraponera, Myrmecia, Neoponera, and the social wasps Synoeca, Agelaia, and Brachygastra. -

Hypersensitivity to Hymenoptera Stings
The new england journal of medicine clinical practice Hypersensitivity to Hymenoptera Stings Theodore M. Freeman, M.D. This Journal feature begins with a case vignette highlighting a common clinical problem. Evidence supporting various strategies is then presented, followed by a review of formal guidelines, when they exist. The article ends with the author’s clinical recommendations. A 29-year-old man reported that he was stung by a flying hymenopteran — he does not know what type — outside his door, where he had previously noted a nest. Skin itching, diffuse hives, swelling of his arms and legs, tightness in his throat, dizziness, and difficulty talking developed immediately, and he was taken to a local clinic where he received epinephrine and antihistamines. He was observed for two hours, and all symptoms resolved. How should his case be managed subsequently? the clinical problem From the Department of Allergy and Im- Insects of the order Hymenoptera, which includes ants, bees, hornets, wasps, and yel- munology, Wilford Hall Medical Center, low jackets, have a stinging apparatus at the tail end of their abdominal segment and Lackland Air Force Base, San Antonio, TX. 1 2 Address reprint requests to Dr. Freeman are capable of delivering between 100 ng (fire ants) and 50 µg (bees) of venom (Table 1 at the Department of Allergy and Immu- and Fig. 1). Although the venoms have various peptide and protein components, some nology, Wilford Hall Medical Center, Lack- of which are capable of inducing toxic or vasoactive responses, it has been estimated land Air Force Base, San Antonio, TX, 78023, or at [email protected]. -

Selected Topics: Toxicology
ARTICLE IN PRESS The Journal of Emergency Medicine, Vol. xx, No. xx, pp. xxx, 2007 Copyright © 2007 Elsevier Inc. Printed in the USA. All rights reserved 0736-4679/07 $–see front matter doi:10.1016/j.jemermed.2007.06.018 Selected Topics: Toxicology ANIMAL BITES AND STINGS WITH ANAPHYLACTIC POTENTIAL John H. Klotz, PHD,* Stephen A. Klotz, MD,† and Jacob L. Pinnas, MD† *Department of Entomology, University of California, Riverside, Riverside, California and †Department of Medicine, University of Arizona School of Medicine, Tucson, Arizona Reprint Address: John H. Klotz, PHD, Department of Entomology, University of California, Riverside, CA 92521 e Abstract—Anaphylaxis to animal bites and stings poses INTRODUCTION a significant medical risk of vascular or respiratory reac- tions that vary according to the patient’s response and Historical Perspective and Definition nature of the insult. Emergency Physicians frequently see patients who complain of an allergic reaction to an animal bite or sting. Although Hymenoptera stings, specifically Anaphylaxis, meaning “without protection,” was coined those of wasps, bees, and hornets, account for the majority in the early 1900s by Richet, who, with Portier, dis- of these cases, other invertebrates and vertebrates are ca- covered the phenomenon while conducting experi- pable of causing allergic reactions and anaphylaxis. Many ments on venom from the Portuguese man-of-war and of the causative animals are quite unusual, and their bites sea anemone. They exposed dogs to small doses of and stings are not commonly appreciated as potential venom and then, several weeks later, repeated the causes of anaphylaxis. We conducted a literature review to injection on these healthy dogs.