Obliterative Bronchiolitis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vocal Cord Dysfunction: Analysis of 27 Cases and Updated Review of Pathophysiology & Management
THIEME Original Research 125 Vocal Cord Dysfunction: Analysis of 27 Cases and Updated Review of Pathophysiology & Management Shibu George1 Sandeep Suresh2 1 Department of ENT, Government Medical College, Kottayam, Kerala, India Address for correspondence ShibuGeorge,MS,DNB,Charivukalayil 2 Department of ENT, Little Flower Hospital, Ernakulam, Kerala, India (House), Ettumanoor, Kottayam 686631, Kerala, India (e-mail: [email protected]; [email protected]). Int Arch Otorhinolaryngol 2019;23:125–130. Abstract Introduction Vocal cord dysfunction is characterized by unintentional paradoxical vocal cord movement resulting in abnormal inappropriate adduction, especially during inspiration; this predominantly manifests as unresponsive asthma or unexplained stridor. It is prudent to be well informed about the condition, since the primary presentation may mask other airway disorders. Objective This descriptive study was intended to analyze presentations of vocal cord dysfunction in a tertiary care referral hospital. The current understanding regarding the pathophysiology and management of the condition were also explored. Methods A total of 27 patients diagnosed with vocal cord dysfunction were analyzed based on demographic characteristics, presentations, associations and examination findings. The mechanism of causation, etiological factors implicated, diagnostic considerations and treatment options were evaluated by analysis of the current literature. Results Therewasastrongfemalepredilection noted among the study population (n ¼ 27), which had a mean age of 31. The most common presentations were stridor Keywords (44%) and refractory asthma (41%). Laryngopharyngeal reflux disease was the most ► Vocal Cord common association in the majority (66%) of the patients, with a strong overlay of Dysfunction anxiety, demonstrable in 48% of the patients. ► paradoxical vocal Conclusion Being aware of the condition is key to avoid misdiagnosis in vocal cord cord motion dysfunction. -
Air Trapping on Computed Tomography: Regional Versus Diffuse
EDITORIAL | SMOKING Air trapping on computed tomography: regional versus diffuse Firdaus A. Mohamed Hoesein and Pim A. de Jong Affiliation: Dept of Radiology, University Medical Center Utrecht, Utrecht, The Netherlands. Correspondence: Firdaus A. Mohamed Hoesein, University Medical Center Utrecht, Department of Radiology, Heidelberglaan 100, PO box 855000, 3508 GA, Utrecht, The Netherlands. E-mail: [email protected] @ERSpublications Future studies on the distribution of air trapping in the lungs of COPD patients are needed http://ow.ly/86hc304JiIK Cite this article as: Mohamed Hoesein FA, de Jong PA. Air trapping on computed tomography: regional versus diffuse. Eur Respir J 2017; 49: 1601791 [https://doi.org/10.1183/13993003.01791-2016]. Chronic obstructive pulmonary disease (COPD) is diagnosed and classified by spirometry, assessing the presence of airflow obstruction and extent of forced expiratory flow deterioration. Spirometry, however, is unsuitable for characterising and quantifying the underlying pulmonary pathology of COPD, including alveolar destruction (emphysema) and airway remodelling (large- and small-airway disease). Accurate diagnosis of the pulmonary pathologies underlying COPD is seen as an important step towards better understanding its biology and “personalised” treatment. Computed tomography (CT) of the lungs provides an excellent opportunity to assess COPD in vivo and quantify its macroscopic pathology [1–3]. Emphysema and airway remodelling can be visually assessed and automatically quantified, and several studies have shown associations with morbidity and mortality [4–7]. In addition, CT can provide information on the spatial distribution of disease. In this issue of the European Respiratory Journal,KARIMI et al. [8] hypothesise that regional air trapping maybe a new imaging marker, in addition to emphysema, large-airway remodelling and diffuse air trapping. -

Middle Airway Obstructiondit May Be Happening Under Our Noses Philip G Bardin,1 Sebastian L Johnston,2 Garun Hamilton1
Thorax Online First, published on July 19, 2012 as 10.1136/thoraxjnl-2012-202221 Chest clinic OPINION Thorax: first published as 10.1136/thoraxjnl-2012-202221 on 19 July 2012. Downloaded from Middle airway obstructiondit may be happening under our noses Philip G Bardin,1 Sebastian L Johnston,2 Garun Hamilton1 < Additional materials are ABSTRACT for this conceptual error to be refuted.2 The virus is published online only. To view Background Lower airway obstruction has evolved to now understood to spread from nose to lung, and these files please visit the denote pathologies associated with diseases of the lung, appropriate recognition of the close association journal online (http://dx.doi.org/ 10.1136/ whereas, conditions proximal to the lung embody upper between upper and lower airway pathologies has thoraxjnl-2012-202221/content/ airway obstruction. This approach has disconnected had positive outcomes. An example is novel strat- early/recent). diseases of the larynx and trachea from the lung, and egies that may not be able to prevent colds, but 1Lung and Sleep Medicine, removed the ‘middle airway’ from the interest and that could ameliorate virus asthma exacerbations Monash University and Hospital involvement of respiratory physicians and scientists. through the use of inhaled interferon.3 and Monash Institute of Medical However, recent studies have indicated that dysfunction Accumulating evidence suggests that the middle Research (MIMR), Melbourne, of this anatomical region may be a key component of Australia airway plays a key role in airway obstruction either 2Respiratory Medicine, Imperial overall airway obstruction, either independently or in independently or with coexisting lung disease. -
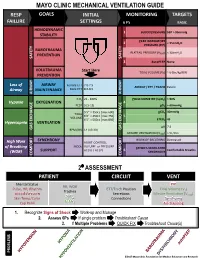
Mechanical Ventilation Guide
MAYO CLINIC MECHANICAL VENTILATION GUIDE RESP GOALS INITIAL MONITORING TARGETS FAILURE SETTINGS 6 P’s BASIC HEMODYNAMIC 1 BLOOD PRESSURE SBP > 90mmHg STABILITY PEAK INSPIRATORY 2 < 35cmH O PRESSURE (PIP) 2 BAROTRAUMA PLATEAU PRESSURE (P ) < 30cmH O PREVENTION PLAT 2 SAFETY SAFETY 3 AutoPEEP None VOLUTRAUMA Start Here TIDAL VOLUME (V ) ~ 6-8cc/kg IBW PREVENTION T Loss of AIRWAY Female ETT 7.0-7.5 AIRWAY / ETT / TRACH Patent Airway MAINTENANCE Male ETT 8.0-8.5 AIRWAY AIRWAY FiO2 21 - 100% PULSE OXIMETRY (SpO2) > 90% Hypoxia OXYGENATION 4 PEEP 5 [5-15] pO2 > 60mmHg 5’5” = 350cc [max 600] pCO2 40mmHg TIDAL 6’0” = 450cc [max 750] 5 VOLUME 6’5” = 500cc [max 850] ETCO2 45 Hypercapnia VENTILATION pH 7.4 GAS GAS EXCHANGE BPM (RR) 14 [10-30] GAS EXCHANGE MINUTE VENTILATION (VMIN) > 5L/min SYNCHRONY WORK OF BREATHING Decreased High Work ASSIST CONTROL MODE VOLUME or PRESSURE of Breathing PATIENT-VENTILATOR AC (V) / AC (P) 6 Comfortable Breaths (WOB) SUPPORT SYNCHRONY COMFORT COMFORT 2⁰ ASSESSMENT PATIENT CIRCUIT VENT Mental Status PIP RR, WOB Pulse, HR, Rhythm ETT/Trach Position Tidal Volume (V ) Trachea T Blood Pressure Secretions Minute Ventilation (V ) SpO MIN Skin Temp/Color 2 Connections Synchrony ETCO Cap Refill 2 Air-Trapping 1. Recognize Signs of Shock Work-up and Manage 2. Assess 6Ps If single problem Troubleshoot Cause 3. If Multiple Problems QUICK FIX Troubleshoot Cause(s) PROBLEMS ©2017 Mayo Clinic Foundation for Medical Education and Research CAUSES QUICK FIX MANAGEMENT Bleeding Hemostasis, Transfuse, Treat cause, Temperature control HYPOVOLEMIA Dehydration Fluid Resuscitation (End points = hypoxia, ↑StO2, ↓PVI) 3rd Spacing Treat cause, Beware of hypoxia (3rd spacing in lungs) Pneumothorax Needle D, Chest tube Abdominal Compartment Syndrome FLUID Treat Cause, Paralyze, Surgery (Open Abdomen) OBSTRUCTED BLOOD RETURN Air-Trapping (AutoPEEP) (if not hypoxic) Pop off vent & SEE SEPARATE CHART PEEP Reduce PEEP Cardiac Tamponade Pericardiocentesis, Drain. -

Imaging of Small Airways Disease
SYMPOSIA Imaging of Small Airways Disease Gerald F. Abbott, MD,* Melissa L. Rosado-de-Christenson, MD,w zy Santiago E. Rossi, MD,J and Saul Suster, MDz SECONDARY PULMONARY LOBULE Abstract: Small airways disease includes a spectrum of inflammatory The secondary pulmonary lobule (SPL) is a key and fibrotic pulmonary diseases centered on the small conducting structure in the lung anatomy and is distinguished as the airways. High-resolution computed tomography plays a key role in the detection and classification of small airways disease and, when smallest functioning subunit of lung that is bound by combined with relevant clinical and pathologic findings, leads to a connective tissue septa, supplied by a lobular bronchiole more accurate diagnosis. The imaging manifestations of small airways and arteriole, and drained by veins and lymphatics in the disease on high-resolution computed tomography may be direct or interlobular septa. Each SPL measures 1 to 2.5 cm and indirect signs of small airway involvement and include centrilobular contains 3 to 12 acini. The SPL are better formed and more nodules and branching nodular (tree-in-bud) opacities, or the easily recognized in the peripheral subpleural lung and demonstration of mosaic attenuation that is typically exaggerated on are smaller and less regular in the central lung. The SPL are expiratory computed tomography. This article reviews the normal not normally visible on radiography or computed tomo- anatomy and histology of bronchioles and the clinical, pathologic, and graphy (CT)/HRCT (Fig. 1). -
Exercise-Induced Laryngeal Obstruction
American Thoracic Society PATIENT EDUCATION | INFORMATION SERIES Exercise-induced Laryngeal Obstruction Exercise-induced laryngeal obstruction (EILO) is a breathing problem that affects people during exercise. EILO is defined by inappropriate narrowing of the upper airway at the level of the vocal cords (glottis) and/or supraglottis (above the vocal cords). This can make it hard to get air into your lungs during exercise and cause a noisy breathing that can be frightening. EILO has also been called vocal cord dysfunction (VCD) or paradoxical vocal fold motion (PVFM). Most people with EILO only have symptoms when they Common signs and symptoms of EILO exercise, those some people may have the problem at During (or immediately after) high-intensity exercise, other times as well. (See ATS Patient Information Series with EILO you may experience: fact sheet ‘Inducible Laryngeal Obstruction/Vocal Cord ■■ Profound shortness of breath or breathlessness Dysfunction’) ■■ Noisy breathing, particularly when breathing in Where are the vocal cords and what do they do? (stridor, gasping, raspy sounds, or “wheezing”) Your vocal cords are located in your upper airway or ■■ A feeling of choking or suffocation that can be scary larynx. Your supraglottic structures (including your ■■ CLIP AND COPY AND CLIP Feeling like there is a lump in the throat arytenoid cartilages and epiglottis) are located above the ■■ Throat or chest tightness vocal cords and are part of your larynx. The larynx is often called the voice box and is deep in your throat. When These symptoms often come on suddenly during you speak, the vocal cords vibrate as you breathe out, exercise, and are typically quite noticeable or concerning to people around you as well. -

Residual Volume and Total Lung Capacity to Assess Reversibility in Obstructive Lung Disease
Residual Volume and Total Lung Capacity to Assess Reversibility in Obstructive Lung Disease Conor T McCartney MD, Melissa N Weis MD, Gregg L Ruppel MEd RRT RPFT FAARC, and Ravi P Nayak MD BACKGROUND: Reversibility of obstructive lung disease is traditionally defined by changes in FEV1 or FVC in response to bronchodilators. These may not fully reflect changes due to a reduction in hyperinflation or air-trapping, which have important clinical implications. To date, only a handful of studies have examined bronchodilators’ effect on lung volumes. The authors sought to better characterize the response of residual volume and total lung capacity to bronchodilators. METHODS: Responsiveness of residual volume and total lung capacity to bronchodilators was assessed with a retrospective analysis of pulmonary function tests of 965 subjects with obstructive lung disease as defined by the lower limit of normal based on National Health and Nutritional Examination Survey III prediction equations. RESULTS: A statistically significant number of subjects demonstrated response to bronchodilators in their residual volume independent of re- sponse defined by FEV1 or FVC, the American Thoracic Society and European Respiratory Society criteria. Reduced residual volume weakly correlated with response to FEV1 and to FVC. No statistically significant correlation was found between total lung capacity and either FEV1 or FVC. CONCLUSIONS: A significant number of subjects classified as being nonresponsive based on spirometry have reversible residual volumes. Subjects whose residual volumes improve in response to bronchodilators represent an important subgroup of those with obstructive lung disease. The identification of this subgroup better characterizes the heterogeneity of obstructive lung disease. The clinical importance of these findings is unclear but warrants further study. -

Obliterative Bronchiolitis with Atypical Features: CT Scan and Necropsy Findings
Copyright @ERS Journals Ud 1993 Eur Aespir J, 1993, 6, 1221-1225 European Respiratory Journal Printed In UK - all rights reserved ISSN 0903 - 1936 CASE REPORT Obliterative bronchiolitis with atypical features: CT scan and necropsy findings M.I.M. Noble, B. Fox, K. Horsfield, I. Gordon, R. Heaton, W.A. Seed, A. Guz Ob/iterative bronchiolitis with atypical features: er scan and necropsy findings. M.l.M. Academic Unit of Cardiovascular Medi Noble, B. Fox, K. Horsjield, l. Gordon, R. Hearon, WA. Seed, A. Guz. ©ERS Journals cine and Depts of Medicine and Pathol l.Jd 1993. ogy, Charing Cross and Westminster ABSTRACT: We describe the natural history of cryptogenic bronchiolitis obliter Medical School. London, and the King ans in a patient foUowed for 24 yrs with serial pulmonary function tests and radi Edward VII Hospital, Midhurst, W . ology. Sussex, UK. Severe, progressive airway obstruction developed, with overinOation but preser Correspondence: M.I.M. Noble, Academic vation of Kco. There was progressive hypoxaemia, which worseroed on exertion; Unit of Cardiovascular Medicine, West hypercapnoca was modest until late in the illness. Neither bronchodilators nor ster minster Hospital, 369 Fulharn Rd, London oids were effective. The chest radiograph remained normal; CT showed irregular SWIO 9NH, UK. areas of low altentuation peripheroUy throughout the lungs, with Bounsfield nu m Keywords: Airway obstruction, bronchi bers typical of emphysema, but no bullae. Postmortem studies included histology olitis obliterans, lung diseases, obstructive and quantitative studies of a corrosion cast of one lung. They showed marked air respiratory insufficiency, pulmonary diffus way narrowing at all levels, with pruning of peripheral branches, mucus plugging, ing capacity. -

Bronchiolitis Obliterans in Workers Exposed to Food Flavorings
HEALTH ALERT Bronchiolitis Obliterans in Workers Exposed to Food Flavorings Recently, several investigations have identified clusters of workers diagnosed with bronchiolitis obliterans (commonly referred to as “popcorn workers’ lung” and “flavorings-related lung disease”), a form of fixed, irreversible airway obstruction, after exposure to mixtures of butter flavoring chemicals. Evaluations of these workers revealed high rates of both severe respiratory symptoms and significantly compromised lung function.1 These investigations concluded that there is a risk for occupational lung disease in workers with inhalation exposure to butter flavoring chemicals.2 Other investigations have also shown that workers that use or manufacture certain food flavoring additives have developed similar health problems. Diacetyl and Other Food Flavorings Used in Food and Flavoring Manufacturing Food flavorings can be either natural or manmade. Some are comprised of only one ingredient, but others are complex mixtures of several substances. Diacetyl is a chemical used in the manufacture of butter flavoring and other food flavorings and is the suspected cause of several cases of bronchiolitis obliterans in workers. During the manufacturing process, workers may be exposed to food flavorings in the form of vapors, dusts, or sprays. There are many different types of food flavorings and most have not been tested for respiratory toxicity. However, recent animal studies of diacetyl exposure conducted by the National Institute for Occupational Safety and Health (NIOSH) have shown an association between diacetyl and fixed obstructive pulmonary disease. What are the health effects associated with flavorings-related lung disease? Exposure to certain airborne food flavorings is associated with higher rates of respiratory symptoms such as coughing, shortness of breath, fatigue, and difficulty breathing with exertion or exercise. -

Focus on Bronchiectasis/COPD Overlap: an Under-Recognized but Critically Important Condition
Focus on Bronchiectasis/COPD Overlap: An Under-Recognized But Critically Important Condition Gary Hansen, PhD Former “Orphan Disease” Grows in Recognition Recognizing • Chronic productive cough Non-cystic fibrosis bronchiectasis (NCFB)1 is an important Bronchiectasis2 disease that remains largely unknown. Once thought to be a rare • Chronic mucus hypersecretion “orphan” condition—merely the aftermath of infectious diseases • Chronic antibiotic use that are now readily treated—emerging evidence now shows that NCFB is far more common than originally believed and is closely • Frequent hospitalizations associated with another better known major respiratory health • Reduced quality of life threat—COPD.3 Defined as the thickening and enlargement of the airways resulting from chronic inflammation, bronchiectasis damages normal airway clearance mechanisms and results in the The process is irreversible and there is no known cure— accumulation of excess secretions. As a result, patients face fortunately, appropriate care can substantially improve the chronic cough, excess sputum production, and a recurring cycle lives of affected patients. of hospitalizations.2 Appropriate diagnosis and treatment are key to improving quality of life and reducing the need for expensive While bronchiectasis may be found at any age, it is most often medical care. Specifically, airway clearance therapy directly a disease of middle-age and older. The profile of a patient with addresses the problem of purulent sputum retained in the bronchiectasis is in many ways similar to that of chronic airways and by “emptying the Petri dish” can help to reduce the bronchitis.8 Affected patients often have a chronic productive risk of future exacerbations without risking exposure to the cough for more than three months of the year along with negative effects of long-term orWhile rotating bronchiectasis antibiotics. -

Respiratory Distress
Respiratory Distress National Pediatric Nighttime Curriculum Written by Liane Campbell, MD Lucile Packard Children’s Hospital, Stanford University Learning Objectives Review the initial assessment of patient in respiratory distress Review management of specific causes of respiratory distress Upper airway obstruction Lower airway obstruction Lung tissue disease Disordered control of breathing During a busy night, you get the following page: FYI: Sally, a 2 year old with PNA had a desat to 88% while on 4L NC. What do you do next? What initial management steps would you take? How do you initially assess a patient in respiratory distress? Initial Assesment Rapid assessment Quickly determine severity of respiratory condition and stabilize child Respiratory distress can quickly lead to cardiac compromise Airway Support or open airway with jaw thrust Suction and position patient Breathing Provide high concentration oxygen Bag mask ventilation Prepare for intubation Administer medication ie albuterol, epinephrine Circulation Establish vascular access: IV/IO History and Physical Exam History Physical Exam Trauma Mental status Change in voice Position of comfort Onset of symptoms Nasal flaring Associated symptoms Accessory muscle use Exposures Respiratory rate and Underlying medical pattern conditions Auscultation for abnormal breath sounds What initial studies would you get for a patient in respiratory distress? Initial studies Pulse oximetry May be difficult in agitated patient May be falsely decreased in very anemic -
PFT Interpretation
PFT Interpretation Presented by: Shazhad Manawar, MD Medical Director Respiratory Care & Pulmonary Rehab McLaren Bay Region Introduction History or symptoms suggestive of lung disease. Risk factors for lung disease are present. Pulmonary Function Tests Spirometry Spirometry before and after bronchodilator Lung volumes Diffusing capacity for carbon monoxide Maximal respiratory pressures Flow volume loops Spirometry Volume of air exhaled at specific time points during forceful and complete exhalation. Total exhaled volume, know as the FVC (forced vital capacity). Volume exhaled in the first second, know as the forced expiratory volume in one second (FEV1) Spirometry - continued Ratio (FEV1/FVC) are the most important variables Minimal risk Key diagnostic test Asthma Chronic Obstructive Pulmonary Disease (COPD) Chronic cough Spirometry - continued Monitor a broad spectrum of respiratory diseases. Asthma COPD Interstitial Lung Disease Neuromuscular diseases affecting respiratory muscles Spirometry - continued Slow vital capacity (SVC) Useful measurement when FVC is reduced and airway obstruction is present Post-bronchodilator Determine the degree of reversibility Administration of albuterol Technique is important Increase in the FEV1 of more than 12% or greater than 0.2 L suggests acute bronchodilator responsiveness. Subjective improvements Post-bronchodilator - continued Thus, the lack of an acute bronchodilator response on spirometry should not preclude a one to eight week therapeutic trial of bronchodilators