Exercise-Induced Laryngeal Obstruction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Larynx Anatomy
LARYNX ANATOMY Elena Rizzo Riera R1 ORL HUSE INTRODUCTION v Odd and median organ v Infrahyoid region v Phonation, swallowing and breathing v Triangular pyramid v Postero- superior base àpharynx and hyoid bone v Bottom point àupper orifice of the trachea INTRODUCTION C4-C6 Tongue – trachea In women it is somewhat higher than in men. Male Female Length 44mm 36mm Transverse diameter 43mm 41mm Anteroposterior diameter 36mm 26mm SKELETAL STRUCTURE Framework: 11 cartilages linked by joints and fibroelastic structures 3 odd-and median cartilages: the thyroid, cricoid and epiglottis cartilages. 4 pair cartilages: corniculate cartilages of Santorini, the cuneiform cartilages of Wrisberg, the posterior sesamoid cartilages and arytenoid cartilages. Intrinsic and extrinsic muscles THYROID CARTILAGE Shield shaped cartilage Right and left vertical laminaà laryngeal prominence (Adam’s apple) M:90º F: 120º Children: intrathyroid cartilage THYROID CARTILAGE Outer surface à oblique line Inner surface Superior border à superior thyroid notch Inferior border à inferior thyroid notch Superior horns à lateral thyrohyoid ligaments Inferior horns à cricothyroid articulation THYROID CARTILAGE The oblique line gives attachement to the following muscles: ¡ Thyrohyoid muscle ¡ Sternothyroid muscle ¡ Inferior constrictor muscle Ligaments attached to the thyroid cartilage ¡ Thyroepiglottic lig ¡ Vestibular lig ¡ Vocal lig CRICOID CARTILAGE Complete signet ring Anterior arch and posterior lamina Ridge and depressions Cricothyroid articulation -

Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St
Vocal Cord Dysfunction JAMES DECKERT, MD, Saint Louis University School of Medicine, St. Louis, Missouri LINDA DECKERT, MA, CCC-SLP, Special School District of St. Louis County, Town & Country, Missouri Vocal cord dysfunction involves inappropriate vocal cord motion that produces partial airway obstruction. Patients may present with respiratory distress that is often mistakenly diagnosed as asthma. Exercise, psychological conditions, airborne irritants, rhinosinusitis, gastroesophageal reflux disease, or use of certain medications may trigger vocal cord dysfunction. The differential diagnosis includes asthma, angioedema, vocal cord tumors, and vocal cord paralysis. Pulmo- nary function testing with a flow-volume loop and flexible laryngoscopy are valuable diagnostic tests for confirming vocal cord dysfunction. Treatment of acute episodes includes reassurance, breathing instruction, and use of a helium and oxygen mixture (heliox). Long-term manage- ment strategies include treatment for symptom triggers and speech therapy. (Am Fam Physician. 2010;81(2):156-159, 160. Copyright © 2010 American Academy of Family Physicians.) ▲ Patient information: ocal cord dysfunction is a syn- been previously diagnosed with asthma.8 A handout on vocal cord drome in which inappropriate Most patients with vocal cord dysfunction dysfunction, written by the authors of this article, is vocal cord motion produces par- have intermittent and relatively mild symp- provided on page 160. tial airway obstruction, leading toms, although some patients may have pro- toV subjective respiratory distress. When a per- longed and severe symptoms. son breathes normally, the vocal cords move Laryngospasm, a subtype of vocal cord away from the midline during inspiration and dysfunction, is a brief involuntary spasm of only slightly toward the midline during expi- the vocal cords that often produces aphonia ration.1 However, in patients with vocal cord and acute respiratory distress. -

How the Larynx (Voice Box) Works
How the Larynx (Voice Box) Works Charles R. Larson, PhD If you love opera, or if you admire the voices of pop singers such as Celine Dion or Barbra Streisand, you may have wondered how it is these marvelous singers are able to create such beautiful music with this instrument we call the human voice. You may also know of someone who has a bad voice or has had to have their voice box, or larynx, removed because of illness or injury. The larynx is a critical organ of human speech and singing, and it serves important biological functions as well. Let's have a look at the larynx to understand its functions, what it looks like and how it works. It is thought that the same factors that favored the evolution of air‐breathing animals on earth led to the evolution of the larynx. Lungs are comprised of very delicate tissues that must be maintained within strict biological limits, that is, temperature, humidity and freedom from foreign particles. Thus, along with the first air‐breathing animals, there appeared a primitive sort of larynx, whose one and only function was protection of the lung. This function remains the most important of those the larynx has assumed in subsequent evolutionary developments. Now, of course we recognize that the larynx is critical for human speech and singing. But we also should realize that the larynx is important for swallowing, coughing, vomiting and eliminating contents of the abdomen. If you have ever felt your 'Adam's Apple', then you know where the larynx is. -
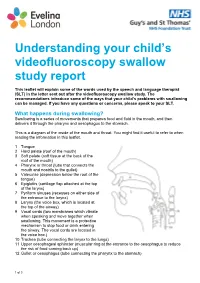
Understanding Your Child's Videofluoroscopy
Understanding your child’s videofluoroscopy swallow study report This leaflet will explain some of the words used by the speech and language therapist (SLT) in the letter sent out after the videofluoroscopy swallow study. The recommendations introduce some of the ways that your child’s problems with swallowing can be managed. If you have any questions or concerns, please speak to your SLT. What happens during swallowing? Swallowing is a series of movements that prepares food and fluid in the mouth, and then delivers it through the pharynx and oesophagus to the stomach. This is a diagram of the inside of the mouth and throat. You might find it useful to refer to when reading the information in this leaflet. 1 Tongue 2 Hard palate (roof of the mouth) 3 Soft palate (soft tissue at the back of the roof of the mouth) 4 Pharynx or throat (tube that connects the mouth and nostrils to the gullet) 5 Valeculae (depression below the root of the tongue) 6 Epiglottis (cartilage flap attached at the top of the larynx) 7 Pyriform sinuses (recesses on either side of the entrance to the larynx) 8 Larynx (the voice box, which is located at the top of the airway) 9 Vocal cords (two membranes which vibrate when speaking and move together when swallowing. This movement is a protective mechanism to stop food or drink entering the airway. The vocal cords are located in the voice box.) 10 Trachea (tube connecting the larynx to the lungs) 11 Upper oesophageal sphincter (muscular ring at the entrance to the oesophagus to reduce the risk of food coming back up) 12 Gullet or oesophagus (tube connecting the pharynx to the stomach) 1 of 3 Swallowing phases Swallowing involves three phases: 1. -

Inhalation of “Borax”
Journal of Paediatrics and Neonatal Disorders Volume 4 | Issue 1 ISSN: 2456-5482 Case Report Open Access Inhalation of “Borax” and Risk of Severe Stridor Obaid O* Department of Pediatrics, MOH, Makkah, Saudi Arabia *Corresponding author: Obaid O, Department of Pediatrics, MOH, Makkah, Saudi Arabia, Tel: 00966500606352, E-mail: [email protected] Citation: Obaid O (2019) Inhalation of “Borax” and Risk of Severe Stridor. J Paedatr Neonatal Dis 4(1): 105 Received Date: March 21, 2019 Accepted Date: June 26, 2019 Published Date: June 28, 2019 Abstract Stridor in children is not uncommon reason to visit emergency department and usually due to croup but inhalation of toxic substance may cause severe stridor which is uncommon. Keywords: Stridor; Pediatric; Sodium Burate Case Report A 9 year old Saudi girl presented to emergency department accompanied by her grandmother with history of dry cough, shortness of breath and audible wheeze for more than12 hours. She has no history of fever, foreign body ingestion and chronic cough. No history of contact with sick person and no history of lip swelling or skin rash. Her vaccination status up to date. She was a Preterm 30 weeks, admitted to Neonatal intensive care for 2 months and discharge well. In emergency room she was ill looking with biphasic stridor, kept on oxygen 10 liter/min and given one dose IM epinephrine 0.3 mg and nebulizer Racemic epinephrine, connected to Cardiorespiratory monitor and 2 IV lines was inserted started on IV Fluids and given one dose of dexamethasone. Urgent consultation to ENT was done and they recommend bronchoscopy to rule out Foreign body ingestion. -

Larynx 2017‐2018 Naaccr Webinar Series
NAACCR 2017-2018 Webinar Series 11/2/2017 COLLECTING CANCER DATA: LARYNX 2017‐2018 NAACCR WEBINAR SERIES Q&A • Please submit all questions concerning webinar content through the Q&A panel. • Reminder: • If you have participants watching this webinar at your site, please collect their names and emails. • We will be distributing a Q&A document in about one week. This document will fully answer questions asked during the webinar and will contain any corrections that we may discover after the webinar. 2 Larynx 1 NAACCR 2017-2018 Webinar Series 11/2/2017 Fabulous Prizes 3 AGENDA • Anatomy • Epi Moment • Quiz 1 • Staging • Treatment • Quiz 2 • Case Scenarios 4 Larynx 2 NAACCR 2017-2018 Webinar Series 11/2/2017 ANATOMY LARYNX 5 LARYNX ANATOMY • Voice Box • Passageway of air • Extends from C3 to C6 vertebrae 6 Larynx 3 NAACCR 2017-2018 Webinar Series 11/2/2017 LARYNX ANATOMY • Divided into 3 Sections • Supraglottis • area above vocal cords, contains epiglottis • arytenoids, aryepiglottic folds and false cords • Glottis • containing true vocal cords, anterior and posterior commissures • Subglottis • below the vocal cords 7 LARYNX ANATOMY • Epiglottis • Aryepiglottic Folds • Anterior and Posterior • False vocal cords Commissure • True vocal cords • Arytenoids 8 Larynx 4 NAACCR 2017-2018 Webinar Series 11/2/2017 LARYNX ANATOMY • Thyroid cartilage • Arytenoid cartilage • Adam’s apple • Influence position and tension of the • Thyrohyoid membrane vocal cords • Cricoid cartilage • Corniculate cartilage • Inferior wall of larynx • Horn shaped pieces located -

Management of Airway Obstruction and Stridor in Pediatric Patients
November 2017 Management of Airway Volume 14, Number 11 Obstruction and Stridor in Authors Ashley Marchese, MD Department of Pediatrics, Yale-New Haven Hospital, New Haven, CT Pediatric Patients Melissa L. Langhan, MD, MHS Associate Professor of Pediatrics and Emergency Medicine; Fellowship Director, Director of Education, Pediatric Emergency Abstract Medicine, Yale University School of Medicine, New Haven, CT Peer Reviewers Stridor is a result of turbulent air-flow through the trachea from Steven S. Bin, MD upper airway obstruction, and although in children it is often Associate Clinical Professor of Emergency Medicine and Pediatrics; Medical Director, Emergency Department, UCSF School of Medicine, due to croup, it can also be caused by noninfectious and/or con- Benioff Children’s Hospital, San Francisco, CA genital conditions as well as life-threatening etiologies. The his- Alexander Toledo, DO, PharmD, FAAEM, FAAP tory and physical examination guide initial management, which Chief, Section of Pediatric Emergency Medicine; Director, Pediatric Emergency Department, Arizona Children’s Center at Maricopa includes reduction of airway inflammation, treatment of bacterial Medical Center, Phoenix, AZ infection, and, less often, imaging, emergent airway stabilization, Prior to beginning this activity, see “Physician CME Information” or surgical management. This issue discusses the most common on the back page. as well as the life-threatening etiologies of acute and chronic stridor and its management in the emergency department. Editor-in-Chief -
Epiglottis Reconstruction with Auricular Free Flap For
ISSN: 2572-4193 Bottini et al. J Otolaryngol Rhinol 2017, 3:032 DOI: 10.23937/2572-4193.1510032 Volume 3 | Issue 2 Journal of Open Access Otolaryngology and Rhinology CASE REPORT Epiglottis Reconstruction with Auricular Free Flap for Re- habilitation of Dysphagia: A Case Study Battista Bottini G1*, Brandtner C1, Rasp G2 and Gaggl A1 1Department of Oral and Maxillofacial Surgery, University Hospital, Private Medical University Paracelsus, Austria 2Department of Ear, Nose and Throat, University Hospital, Private Medical University Paracelsus, Check for updates Austria *Corresponding author: Gian Battista Bottini, MD, DMD, Department of Oral and Maxillofacial Surgery, Uni- versity Hospital, Private Medical University Paracelsus, 48 Muellner Hauptstrasse, 5020 Salzburg, Austria, Tel: +43(0)57255-57230, Fax: +43(0)57255-26499, E-mail: [email protected] and requires a coordinated activity of nerves, muscles, Abstract the hyoid bone and the larynx [1]. The process can be Supraglottic laryngectomy for laryngeal cancer aims to remove divided in stages: oral pharyngeal and oesophageal [1]. cancer of the larynx whilst preserving its functions of airway protection, breathing and voice production. A well-known long- During the pharyngeal stage, the vocal cords adduct term complication of this procedure is aspiration. to seal the glottis and the arytenoid tilt forward to con- We present a case of a delayed epiglottis reconstruction tact the epiglottis base. with auricular free flap for surgical rehabilitation of dyspha- gia. Primarily the patient underwent supraglottic laryngecto- When the hyo-laryngeal complex is pulled in anterior my, bilateral neck dissection and radiotherapy. She had a and superior direction against the base of the tongue, permanent tracheostoma because of a complete paralysis the epiglottis, acting like a shield, tilts backwards and of the right vocal cord and a residual minimal mobility of the covers completely the glottis [1]. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Diagnostic Direct Laryngoscopy, Bronchoscopy & Esophagoscopy
Post-Operative Instruction Sheet Diagnostic Direct Laryngoscopy, Bronchoscopy & Esophagoscopy Direct Laryngoscopy: Examination of the voice box or larynx (pronounced “lair-inks”) under general anesthesia. An instrument called a laryngoscope is carefully placed into the mouth and used to visualize the larynx and surrounding structures. Bronchoscopy: Examination of the windpipe below the voice box in the neck and chest under general anesthesia. A long narrow telescope is passed through the larynx and used to carefully inspect the structures of the trachea and bronchi. Esophagoscopy: Examination of the swallowing pipe in the neck and chest under general anesthesia. An instrument called an esophagoscope is passed into the esophagus (just behind the larynx and trachea) and used to visualize the mucus membranes and surrounding structures of the esophagus. Frequently a small biopsy is taken to evaluate for signs of esophageal inflammation (esophagitis). What to Expect: Diagnostic airway endoscopy procedures generally take about 45 minutes to complete. Usually the procedure is well-tolerated and the child is back-to-normal the next day. Mild throat or tongue discomfort may persist for a few days after the procedure and is usually well-controlled with over-the-counter acetaminophen (Tylenol) or ibuprofen (Motrin). Warning Signs: Contact the office immediately at (603) 650-4399 if any of the following develop: • Worsening harsh, high-pitched noisy-breathing (stridor) • Labored breathing with chest retractions or flaring of the nostrils • Bluish discoloration of the lips or fingernails (cyanosis) • Persistent fever above 102°F that does not respond to Tylenol or Motrin • Excessive coughing or respiratory distress during feeding • Coughing or throwing up bright red blood • Excessive drowsiness or unresponsiveness Diet: Resume baseline diet (no special postoperative diet restrictions). -

Vocal Cord Dysfunction: Analysis of 27 Cases and Updated Review of Pathophysiology & Management
THIEME Original Research 125 Vocal Cord Dysfunction: Analysis of 27 Cases and Updated Review of Pathophysiology & Management Shibu George1 Sandeep Suresh2 1 Department of ENT, Government Medical College, Kottayam, Kerala, India Address for correspondence ShibuGeorge,MS,DNB,Charivukalayil 2 Department of ENT, Little Flower Hospital, Ernakulam, Kerala, India (House), Ettumanoor, Kottayam 686631, Kerala, India (e-mail: [email protected]; [email protected]). Int Arch Otorhinolaryngol 2019;23:125–130. Abstract Introduction Vocal cord dysfunction is characterized by unintentional paradoxical vocal cord movement resulting in abnormal inappropriate adduction, especially during inspiration; this predominantly manifests as unresponsive asthma or unexplained stridor. It is prudent to be well informed about the condition, since the primary presentation may mask other airway disorders. Objective This descriptive study was intended to analyze presentations of vocal cord dysfunction in a tertiary care referral hospital. The current understanding regarding the pathophysiology and management of the condition were also explored. Methods A total of 27 patients diagnosed with vocal cord dysfunction were analyzed based on demographic characteristics, presentations, associations and examination findings. The mechanism of causation, etiological factors implicated, diagnostic considerations and treatment options were evaluated by analysis of the current literature. Results Therewasastrongfemalepredilection noted among the study population (n ¼ 27), which had a mean age of 31. The most common presentations were stridor Keywords (44%) and refractory asthma (41%). Laryngopharyngeal reflux disease was the most ► Vocal Cord common association in the majority (66%) of the patients, with a strong overlay of Dysfunction anxiety, demonstrable in 48% of the patients. ► paradoxical vocal Conclusion Being aware of the condition is key to avoid misdiagnosis in vocal cord cord motion dysfunction. -

Efficacy of Fiberoptic Laryngoscopy in the Diagnosis of Inhalation Injuries
ORIGINAL ARTICLE Efficacy of Fiberoptic Laryngoscopy in the Diagnosis of Inhalation Injuries Thomas Muehlberger, MD; Dario Kunar, MD; Andrew Munster, MD; Marion Couch, MD, PhD Background: Asignificantproportionofburnpatientswith Results: Six (55%) of 11 patients had clinical findings and inhalation injuries incur difficulties with airway protection, symptoms that indicated, under traditional criteria, endo- dysphagia, and aspiration. In assessing the need for intu- tracheal intubation for airway protection. Visualization of bation in burn patients, the efficacy of fiberoptic laryngos- the upper airway with fiberoptic laryngoscopy obviated the copy was compared with clinical findings and the findings need for endotracheal intubation in all 11 patients. These of diagnostic tests, such as arterial blood gas analysis, mea- patients also failed to evidence an increased risk of aspira- surement of carboxyhemoglobin levels, pulmonary func- tion or other swallowing dysfunction. tion tests, and radiography of the lateral aspect of the neck. Conclusions: In comparison with other diagnostic cri- Objective: To determine if these patients were at risk teria, fiberoptic laryngoscopy allows differentiation of for aspiration or dysphagia, barium-enhanced fluoro- those patients with inhalation injuries who, while at scopic swallowing studies were performed. risk for upper airway obstruction, do not require intu- bation. These patients may be safely observed in a moni- Design: Prospective study. tored setting with serial fiberoptic examinations, thus avoiding the possible complications associated with in- Settings: Burn intensive care unit in an academic ter- tubation of an airway with a compromised mucosalized tiary referral center. surface. In these patients, swallowing abnormalities do not manifest. Main Outcome Measures: Need for endotracheal in- tubation and potential for aspiration.