Managing Airway Obstruction
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

ABCDE Approach
The ABCDE and SAMPLE History Approach Basic Emergency Care Course Objectives • List the hazards that must be considered when approaching an ill or injured person • List the elements to approaching an ill or injured person safely • List the components of the systematic ABCDE approach to emergency patients • Assess an airway • Explain when to use airway devices • Explain when advanced airway management is needed • Assess breathing • Explain when to assist breathing • Assess fluid status (circulation) • Provide appropriate fluid resuscitation • Describe the critical ABCDE actions • List the elements of a SAMPLE history • Perform a relevant SAMPLE history. Essential skills • Assessing ABCDE • Needle-decompression for tension • Cervical spine immobilization pneumothorax • • Full spine immobilization Three-sided dressing for chest wound • • Head-tilt and chin-life/jaw thrust Intravenous (IV) line placement • • Airway suctioning IV fluid resuscitation • • Management of choking Direct pressure/ deep wound packing for haemorrhage control • Recovery position • Tourniquet for haemorrhage control • Nasopharyngeal (NPA) and oropharyngeal • airway (OPA) placement Pelvic binding • • Bag-valve-mask ventilation Wound management • • Skin pinch test Fracture immobilization • • AVPU (alert, voice, pain, unresponsive) Snake bite management assessment • Glucose administration Why the ABCDE approach? • Approach every patient in a systematic way • Recognize life-threatening conditions early • DO most critical interventions first - fix problems before moving on -

Job Hazard Analysis
Identifying and Evaluating Hazards in Research Laboratories Guidelines developed by the Hazards Identification and Evaluation Task Force of the American Chemical Society’s Committee on Chemical Safety Copyright 2013 American Chemical Society Table of Contents FOREWORD ................................................................................................................................................... 3 ACKNOWLEDGEMENTS ................................................................................................................................. 5 Task Force Members ..................................................................................................................................... 6 1. SCOPE AND APPLICATION ..................................................................................................................... 7 2. DEFINITIONS .......................................................................................................................................... 7 3. HAZARDS IDENTIFICATION AND EVALUATION ................................................................................... 10 4. ESTABLISHING ROLES AND RESPONSIBILITIES .................................................................................... 14 5. CHOOSING AND USING A TECHNIQUE FROM THIS GUIDE ................................................................. 17 6. CHANGE CONTROL .............................................................................................................................. 19 7. ASSESSING -

Airway – Oropharyngeal: Insertion; Maintenance; Suction; Removal
Policies & Procedures Title: AIRWAY – OROPHARYNGEAL: INSERTION; MAINTENANCE; SUCTION; REMOVAL I.D. Number: 1159 Authorization Source: Nursing Date Revised: September 2014 [X] SHR Nursing Practice Committee Date Effective: October 2002 Date Reaffirmed: January 2016 Scope: SHR Acute, Parkridge Centre Any PRINTED version of this document is only accurate up to the date of printing 30-May-16. Saskatoon Health Region (SHR) cannot guarantee the currency or accuracy of any printed policy. Always refer to the Policies and Procedures site for the most current versions of documents in effect. SHR accepts no responsibility for use of this material by any person or organization not associated with SHR. No part of this document may be reproduced in any form for publication without permission of SHR. 1. PURPOSE 1.1 To safely and effectively use Oropharyngeal Airway (OPA). 2. POLICY 2.1 The Registered Nurse (RN), Registered Psychiatric Nurse (RPN), Licensed Practical Nurse (LPN), Graduate Nurse (GN), Graduate Psychiatric Nurse (GPN), Graduate Licensed Practical Nurse (GLPN) will insert, maintain, suction and remove an oropharyngeal airway (OPA). 2.2 The OPA may be inserted to establish and assist in maintaining a patent airway. 2.3 An OPA should only be used in patients with decreased level of consciousness or decreased gag reflex. 2.4 Patients with OPAs that have been inserted for airway protection should not be left unattended due to risk of aspiration if gag reflex returns unexpectedly. Page 1 of 4 Policies and Procedures: Airway – Oropharyngeal: Insertion; Maintenance; I.D. # 1159 Suction; Removal 3. PROCEDURE 3.1 Equipment: • Oropharyngeal airway of appropriate size • Tongue blade (optional) • Clean gloves • Optional: suction equipment, bag-valve-mask device 3.2 Estimate the appropriate size of airway by aligning the tube on the side of the patient’s face parallel to the teeth and choosing an airway that extends from the ear lobe to the corner of the mouth. -

Inhalation of “Borax”
Journal of Paediatrics and Neonatal Disorders Volume 4 | Issue 1 ISSN: 2456-5482 Case Report Open Access Inhalation of “Borax” and Risk of Severe Stridor Obaid O* Department of Pediatrics, MOH, Makkah, Saudi Arabia *Corresponding author: Obaid O, Department of Pediatrics, MOH, Makkah, Saudi Arabia, Tel: 00966500606352, E-mail: [email protected] Citation: Obaid O (2019) Inhalation of “Borax” and Risk of Severe Stridor. J Paedatr Neonatal Dis 4(1): 105 Received Date: March 21, 2019 Accepted Date: June 26, 2019 Published Date: June 28, 2019 Abstract Stridor in children is not uncommon reason to visit emergency department and usually due to croup but inhalation of toxic substance may cause severe stridor which is uncommon. Keywords: Stridor; Pediatric; Sodium Burate Case Report A 9 year old Saudi girl presented to emergency department accompanied by her grandmother with history of dry cough, shortness of breath and audible wheeze for more than12 hours. She has no history of fever, foreign body ingestion and chronic cough. No history of contact with sick person and no history of lip swelling or skin rash. Her vaccination status up to date. She was a Preterm 30 weeks, admitted to Neonatal intensive care for 2 months and discharge well. In emergency room she was ill looking with biphasic stridor, kept on oxygen 10 liter/min and given one dose IM epinephrine 0.3 mg and nebulizer Racemic epinephrine, connected to Cardiorespiratory monitor and 2 IV lines was inserted started on IV Fluids and given one dose of dexamethasone. Urgent consultation to ENT was done and they recommend bronchoscopy to rule out Foreign body ingestion. -

Management of Airway Obstruction and Stridor in Pediatric Patients
November 2017 Management of Airway Volume 14, Number 11 Obstruction and Stridor in Authors Ashley Marchese, MD Department of Pediatrics, Yale-New Haven Hospital, New Haven, CT Pediatric Patients Melissa L. Langhan, MD, MHS Associate Professor of Pediatrics and Emergency Medicine; Fellowship Director, Director of Education, Pediatric Emergency Abstract Medicine, Yale University School of Medicine, New Haven, CT Peer Reviewers Stridor is a result of turbulent air-flow through the trachea from Steven S. Bin, MD upper airway obstruction, and although in children it is often Associate Clinical Professor of Emergency Medicine and Pediatrics; Medical Director, Emergency Department, UCSF School of Medicine, due to croup, it can also be caused by noninfectious and/or con- Benioff Children’s Hospital, San Francisco, CA genital conditions as well as life-threatening etiologies. The his- Alexander Toledo, DO, PharmD, FAAEM, FAAP tory and physical examination guide initial management, which Chief, Section of Pediatric Emergency Medicine; Director, Pediatric Emergency Department, Arizona Children’s Center at Maricopa includes reduction of airway inflammation, treatment of bacterial Medical Center, Phoenix, AZ infection, and, less often, imaging, emergent airway stabilization, Prior to beginning this activity, see “Physician CME Information” or surgical management. This issue discusses the most common on the back page. as well as the life-threatening etiologies of acute and chronic stridor and its management in the emergency department. Editor-in-Chief -

CARBON MONOXIDE: the SILENT KILLER Information You Should
CARBON MONOXIDE: THE SILENT KILLER Information You Should Know Carbon monoxide is a silent killer that can lurk within fossil fuel burning household appliances. Many types of equipment and appliances burn different types of fuel to provide heat, cook, generate electricity, power vehicles and various tools, such as chain saws, weed eaters and leaf blowers. When these units operate properly, they use fresh air for combustion and vent or exhaust carbon dioxide. When fresh air is restricted, through improper ventilation, the units create carbon monoxide, which can saturate the air inside the structure. Carbon Monoxide can be lethal when accidentally inhaled in concentrated doses. Such a situation is referred to as carbon monoxide poisoning. This is a serious condition that is a medical emergency that should be taken care of right away. What Is It? Carbon monoxide, often abbreviated as CO, is a gas produced by burning fossil fuel. What makes it such a silent killer is that it is odorless and colorless. It is extremely difficult to detect until the body has inhaled a detrimental amount of the gas, and if inhaled in high concentrations, it can be fatal. Carbon monoxide causes tissue damage by blocking the body’s ability to absorb enough oxygen. In fact, poisoning from this gas is one of the leading causes of unintentional death from poison. Common Sources of CO Kerosene or fuel-based heaters Fireplaces Gasoline powered equipment and generators Charcoal grills Automobile exhaust Portable generators Tobacco smoke Chimneys, furnaces, and boilers Gas water heaters Wood stoves and gas stoves Properly installed and maintained appliances are safe and efficient. -

Vocal Cord Dysfunction: Analysis of 27 Cases and Updated Review of Pathophysiology & Management
THIEME Original Research 125 Vocal Cord Dysfunction: Analysis of 27 Cases and Updated Review of Pathophysiology & Management Shibu George1 Sandeep Suresh2 1 Department of ENT, Government Medical College, Kottayam, Kerala, India Address for correspondence ShibuGeorge,MS,DNB,Charivukalayil 2 Department of ENT, Little Flower Hospital, Ernakulam, Kerala, India (House), Ettumanoor, Kottayam 686631, Kerala, India (e-mail: [email protected]; [email protected]). Int Arch Otorhinolaryngol 2019;23:125–130. Abstract Introduction Vocal cord dysfunction is characterized by unintentional paradoxical vocal cord movement resulting in abnormal inappropriate adduction, especially during inspiration; this predominantly manifests as unresponsive asthma or unexplained stridor. It is prudent to be well informed about the condition, since the primary presentation may mask other airway disorders. Objective This descriptive study was intended to analyze presentations of vocal cord dysfunction in a tertiary care referral hospital. The current understanding regarding the pathophysiology and management of the condition were also explored. Methods A total of 27 patients diagnosed with vocal cord dysfunction were analyzed based on demographic characteristics, presentations, associations and examination findings. The mechanism of causation, etiological factors implicated, diagnostic considerations and treatment options were evaluated by analysis of the current literature. Results Therewasastrongfemalepredilection noted among the study population (n ¼ 27), which had a mean age of 31. The most common presentations were stridor Keywords (44%) and refractory asthma (41%). Laryngopharyngeal reflux disease was the most ► Vocal Cord common association in the majority (66%) of the patients, with a strong overlay of Dysfunction anxiety, demonstrable in 48% of the patients. ► paradoxical vocal Conclusion Being aware of the condition is key to avoid misdiagnosis in vocal cord cord motion dysfunction. -
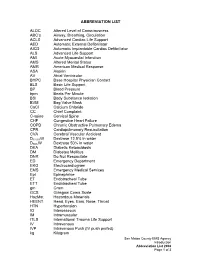
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

Supraglottoplasty Home Care Instructions Hospital Stay Most Children Stay Overnight in the Hospital for at Least One Night
10914 Hefner Pointe Drive, Suite 200 Oklahoma City, OK 73120 Phone: 405.608.8833 Fax: 405.608.8818 Supraglottoplasty Home Care Instructions Hospital Stay Most children stay overnight in the hospital for at least one night. Bleeding There is typically very little to no bleeding associated with this procedure. Though very unlikely to happen, if your child were to spit or cough up blood you should contact your physician immediately. Diet After surgery your child will be able to eat the foods or formula that they usually do. It is important after surgery to encourage your child to drink fluids and remain hydrated. Daily fluid needs are listed below: • Age 0-2 years: 16 ounces per day • Age 2-4 years: 24 ounces per day • Age 4 and older: 32 ounces per day It is our experience that most children experience a significant improvement in eating after this procedure. However, we have found about that approximately 4% of otherwise healthy infants may experience a transient onset of coughing or choking with feeding after surgery. In our experience these symptoms resolve over 1-2 months after surgery. We have also found that infants who have other illnesses (such as syndromes, prematurity, heart trouble, or other congenital abnormalities) have a greater risk of experiencing swallowing difficulties after a supraglottoplasty (this number can be as high as 20%). In time the child usually will return to normal swallowing but there is a small risk of feeding difficulties. You will be given a prescription before you leave the hospital for an acid reducing (anti-reflux) medication that must be filled before you are discharged. -

Effects of Anaesthesia Techniques and Drugs on Pulmonary Function
Review Article Effects of anaesthesia techniques and drugs on pulmonary function Address for correspondence: Vijay Saraswat Dr. Vijay Saraswat, Department of Anaesthesiology, Apollo Hospitals, Nashik, Maharashtra, India Apollo Hospitals, Nashik, Maharashtra, India. E‑mail: drvsaraswat@gmail. ABSTRACT com The primary task of the lungs is to maintain oxygenation of the blood and eliminate carbon dioxide through the network of capillaries alongside alveoli. This is maintained by utilising ventilatory reserve capacity and by changes in lung mechanics. Induction of anaesthesia impairs pulmonary functions by the loss of consciousness, depression of reflexes, changes in rib cage and haemodynamics. All drugs used during anaesthesia, including inhalational agents, affect pulmonary functions directly by acting on respiratory system or indirectly through their actions on other systems. Volatile anaesthetic agents have more pronounced effects on pulmonary functions compared to intravenous induction agents, leading to hypercarbia and hypoxia. The posture of the patient also leads to major changes in pulmonary functions. Anticholinergics and neuromuscular blocking agents have little effect. Analgesics and Access this article online sedatives in combination with volatile anaesthetics and induction agents may exacerbate Website: www.ijaweb.org their effects. Since multiple agents are used during anaesthesia, ultimate effect may be DOI: 10.4103/0019‑5049.165850 different from when used in isolation. Literature search was done using MeSH key words ‘anesthesia’, -

Stridor in the Newborn
Stridor in the Newborn Andrew E. Bluher, MD, David H. Darrow, MD, DDS* KEYWORDS Stridor Newborn Neonate Neonatal Laryngomalacia Larynx Trachea KEY POINTS Stridor originates from laryngeal subsites (supraglottis, glottis, subglottis) or the trachea; a snoring sound originating from the pharynx is more appropriately considered stertor. Stridor is characterized by its volume, pitch, presence on inspiration or expiration, and severity with change in state (awake vs asleep) and position (prone vs supine). Laryngomalacia is the most common cause of neonatal stridor, and most cases can be managed conservatively provided the diagnosis is made with certainty. Premature babies, especially those with a history of intubation, are at risk for subglottic pathologic condition, Changes in voice associated with stridor suggest glottic pathologic condition and a need for otolaryngology referral. INTRODUCTION Families and practitioners alike may understandably be alarmed by stridor occurring in a newborn. An understanding of the presentation and differential diagnosis of neonatal stridor is vital in determining whether to manage the child with further observation in the primary care setting, specialist referral, or urgent inpatient care. In most cases, the management of neonatal stridor is outside the purview of the pediatric primary care provider. The goal of this review is not, therefore, to present an exhaustive review of causes of neonatal stridor, but rather to provide an approach to the stridulous newborn that can be used effectively in the assessment and triage of such patients. Definitions The neonatal period is defined by the World Health Organization as the first 28 days of age. For the purposes of this discussion, the newborn period includes the first 3 months of age. -

Respiratory System
Respiratory System 1 Respiratory System 2 Respiratory System 3 Respiratory System 4 Respiratory System 5 Respiratory System 6 Respiratory System 7 Respiratory System 8 Respiratory System 9 Respiratory System 10 Respiratory System 11 Respiratory System • Pulmonary Ventilation 12 Respiratory System 13 Respiratory System 14 Respiratory System • Measuring of Lung Function œ Compliance œ the ease at which the lungs and thoracic wall can be expanded œ if reduced it is more difficult to inflate the lungs œ causes: • Damaged lung tissue • Fluid within lung tissue • Decrease in pulmonary surfactant • Anything that impedes lung expansion or contraction œ Respiratory Volumes and Capacities will be covered in Lab œ 15 Respiratory System • Exchange of Oxygen and Carbon Dioxide œ Charles‘ Law œ the volume of a gas is directly proportional to the absolute temperature, assuming the pressure remains constant As gases enter the lung they warm and expand, increasing lung volume œ Dalton‘s Law œ each gas of a mixture of gases exerts its own pressure as if all the other gases were not present œ Henry‘s Law œ the quantity of a gas that will dissolve in a liquid is proportional to the partial pressure of the gas and its solubility coefficient, when the temperature remains constant 16 Respiratory System • External and Internal Respiration 17 Respiratory System • Transport of Oxygen and Carbon Dioxide by the Blood œ Oxygen Transport • 1.5% dissolved in plasma • 98.5% carried with Hbinside of RBC‘s as oxyhemoglobin œ Hbœ made up of protein portion called the globinportion