Pre-Placement Information 2016 - 2017
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

16 Hampton Court Inchicore Dublin 8 D08 V9V3 for SALE
FOR SALE BY PRIVATE TREATY 16 Hampton Court Inchicore Dublin 8 D08 V9V3 One Bedroom Apartment c.47.3.sq.m /510sq.ft Price: €199,000 raycooke.ie DESCRIPTION FEATURES RAY COOKE AUCTIONEERS proudly present this stunning - Fantastic location ground floor own front door one bedroom apartment to the - 5 minutes from The Luas market in a very popular and well located development of - Renovated from top to bottom Hampton Court, Dublin 8. Hampton Court is a very popular - c.510 sq.ft. size development within easy reach of all local amenities including shopping facilities, pubs, schools and has excellent transport - Gas heating links. The area is well serviced with excellent road networks - STUNNING APARTMENT and also has the Red Luas Line within striking distance. - Double Glazed windows Neighbouring amenities include the Grand Canal walkway, - Management fees €850 Grattan Crescent Park and the Irish Museum of Modern Art to name but a few. The city centre is only 10 minutes by car and public transport access is available via a series of central bus routes and the Red Line LUAS at the Blackhorse stop. This bright and tastefully decorated living accommodation of 510sq.ft comprises of entrance hall, double bedroom, family bathroom, open plan lounge/dining room and kitchen area. No. 16 comes to the market in pristine condition throughout. Interest is sure to be expected from 1st time buyers and investors alike so call Ray Cooke Auctioneers for further information or to arrange viewing! raycooke.ie ACCOMMODATION LOUNGE Bright lounge to the front of the property with laminate flooring and open plan to kitchen. -

Dublin-1.Pdf
Duration County Institution Name Eircode Course Title in Years QQI Level SUSI Course Code Dublin Ballsbridge CFE D04 R201 Advanced Certificate in Business 1 6 DC16M4985 Dublin Ballsbridge CFE D04 R201 Advanced Certificate in Event Management 1 6 DC16M4985A Dublin Ballsbridge CFE D04 R201 Applied Psychology 1 5 DC15M4468 Dublin Ballsbridge CFE D04 R201 Auctioneering, Estate Agency and Valuation 1 5 DC15M2102 Dublin Ballsbridge CFE D04 R201 Business Studies 1 5 DC15M2102A Dublin Ballsbridge CFE D04 R201 Business Studies with Chinese 1 5 DC15M2102B Dublin Ballsbridge CFE D04 R201 Community Development 1 6 DC16M3674 Dublin Ballsbridge CFE D04 R201 Computerised Office Skills 1 5 DC15M2102C Dublin Ballsbridge CFE D04 R201 Criminology and Social Studies 1 5 DC15M4468A Dublin Ballsbridge CFE D04 R201 Digital Marketing 1 5 DC15M2069 Dublin Ballsbridge CFE D04 R201 English (EFL) and Business Communications 1 5 DC15M2102D Dublin Ballsbridge CFE D04 R201 Event Management 1 5 DC15M2102E Dublin Ballsbridge CFE D04 R201 FinTech- Financial Technology Skills 1 5 DC15M2102J Dublin Ballsbridge CFE D04 R201 Health Sector Studies 1 5 DC15M4468B Dublin Ballsbridge CFE D04 R201 Human Resource Management 1 5 DC15M2102F Dublin Ballsbridge CFE D04 R201 International Aid and Development 1 5 DC15M2102G Dublin Ballsbridge CFE D04 R201 Marketing, Advertising and Management 1 5 DC15M2069A Dublin Ballsbridge CFE D04 R201 Property Management 1 5 DC15M2102H Dublin Ballsbridge CFE D04 R201 Start Your Own Business 1 5 DC15M2102I Dublin Ballsbridge CFE D04 R201 TEFL with Business Management 1 6 DC16M4985B Dublin Ballsbridge CFE D04 R201 Web Authoring and Multimedia 1 5 DC15M2146 Dublin Ballyfermot CFE D10 TX46 Advanced Certificate in Tourism with Business. -

The Traveller Parish Newsletter
The Traveller Parish Newsletter Autumn 2011 PARISH ATTENDS INTERNATIONAL CONFERENCE, HOLLAND CELEBRATING OLDER FIRST HOLY COMMUNIONS & MAKING A YOUTH ZONE TRAVELLERS’ CONTRIBUTION CONFIRMATIONS DIFFERENCE YELLOW FLAG AWARDS WELCOME uring the month of November it is our strong tradition here in Ireland, and certainly nowhere more so than Dwithin the Traveller community, to give extra-special thought, time and prayer to our deceased loved ones, family members, friends, and all the faithful departed. As well as the day celebrating the Feast of All Souls on November 2nd, many Masses will be offered, candles lit, memories shared, and prayers said all through the month for those who have passed from this world. In the darkness of wintry November days the warmth and brightness of loving prayer for our deceased is itself a a country at war when he was a child, and he had been forced blessing, both for those who pray, and also those we pray for. to become a child soldier, so witnessing and being part of In this edition we remember especially those who have taken some terrible events. ‘What was the one thing’, the conference their own lives, and we include each one in our prayers. We speaker asked,’ that the man was looking for, specific to the think also of the families so deeply affected by their traumatic ‘medicine man’, and that for him the others could not and sad loss, and we offer a prayer for the grace, strength, provide?’ The answer, it was suggested in this case, is release support, and comfort they need in their pain and grief. -

The Parishes of Mary Immaculate; St Michael's, Inchicore and Our Lady
The Parishes of Mary Immaculate; St Michael’s, Inchicore and Our Lady of the Wayside, Bluebell. Oblate Pastoral Area Newsletter Tenth Sunday in Ordinary Time 10th June 2018 The Blessed Sacrament The Pastoral Area Masses & Confessions On Sunday 3rd May 2018 we celebrated Mary Immaculate the wonderful Feast of Corpus Christi or the Body of Christ. This feast was Sundays: (Vigil) Sat 7pm, introduced by the Church to help us to 8am, 11am, 7pm reflect on and to thank Christ for this Weekdays Mon – Fri 7am great gift. The Eucharist was instituted 10am, 7pm, Sat 11am by Jesus Christ during the Last Supper Holy Days 7pm (Vigil), 7am, when He gathered with His disciples the 10am, 7pm night before He died on Calvary. During Holy Days that fall on a Saturday this meal Jesus prayed for His disciples (and us) and stressed the importance of 7pm (Vigil), 11am, 7pm them being united and supportive of Confessions Sat 10.30 - 11am & each other. He gave us the Eucharist as 6.30 - 7pm a sign of our unity with Him and with each other. However the Eucharist must St Michael’s never be seen as just a relationship between Jesus and me. It binds us into the Sundays (Vigil) Sat 6.30pm community of disciples as St Paul tells us in his letter to the 1 Corinthians Sunday 9am & 11am (Family) 10:17 “ …. we are one body, for we all share the one bread.” It is meant to Weekdays (Mon – Fri) 10am strengthen us for the journey of life and to enable us to give witness to Him by Liturgy of the Word & Communion on our daily living and active concern for others. -

Report Master
To the Lord Mayor and Report No. 275/2019 Members of Dublin City Council Report of the Chief Executive ________________________________________________________________________ DRAFT PARK WEST – CHERRY ORCHARD LOCAL AREA PLAN 2019 CHIEF EXECUTIVE’S REPORT ON SUBMISSIONS FROM PUBLIC DISPLAY OF DRAFT PLAN The report of the Chief Executive was issued to the members of the City Council on the 30th August 2019. An addendum was issued on the 5th September 2019, included below as Section 6. Owen Keegan Chief Executive, Dublin City Council 30th August 2019 1 INTRODUCTION .......................................................................................................................... 3 1.1 FORMAT OF CHIEF EXECUTIVE’S REPORT ................................................................................ 3 1.2 CONTEXT ............................................................................................................................... 3 2 PROCESS TO DATE AND NEXT STEPS .................................................................................. 4 2.1 PRE-DRAFT CONSULTATION PROCESS (ISSUES PAPER) ........................................................... 4 2.2 DRAFT PARK WEST – CHERRY ORCHARD LOCAL AREA PLAN 2019 PUBLIC CONSULTATION PROCESS .......................................................................................................................................... 4 2.3 NEXT STEPS: ADOPTION / AMENDMENT OF PLAN ..................................................................... 5 3 SUBMISSION RECEIVED .......................................................................................................... -

614 Greenogue Business Park.Qxd
International Property Consultants Savills 33 Molesworth Street t: +353 1 618 1300 Dublin 2 e: [email protected] savills.ie For Sale by Private Treaty Prime "Ready To Go" industrial site with superb access to the N7 Site 614, Greenogue Business Park, Co. Dublin Industrial Division • Approx. 1.21 hectares (3 acres) within • Excellent location within minutes of the Contact a well established business location Naas Road (N7), the M50 and the new Gavin Butler, Niall Woods & Stephen Mellon Outer Ring Road (connecting the N4 and the N7) Dublin N7 Naas Baldonnell Aerodrome R120 Aerodrome Business Park Greenogue Business Park For Sale by Private Treaty Site 614 Greenogue Business Park, Co. Dublin M alahide Location Services M50 Sw o rds Railway Portmarnock DART LU A S National Primary Roads Greenogue Business Park is a well- We understand that all mains services M1 Regional Roads N2 Balgriffin Santry Baldoyle Ballym un Sut ton established development located approx. are available and connected to the site. Coolock Beaum ont Howth N3 Blanchardstown Finglas Whitehall Artane Raheny Clonsilla Killester Ashtown Glasnevin 1.1 km from the Rathcoole Interchange on Drum condra M50 Castleknock Marino Clontarf Cabra Phibsborough Fairview Lucan the Naas Road (N7). This interchange is Zoning Palmerstown Chapelizo d N4 Liffey Ringsend Valley Ballyfermot Inchico r e Sandym ount Drimnagh Ballsbridge 8.5 km from the N7 / M50 motorway Under the South Dublin County Council Crum lin Harold's Ranelagh Rathmines Cross Donnybrook Clondalkin Walkinstown Rathgar Kimm age Milltown Blackr ock Te r enure Booterstown Greenhills Rathfarnham junction and is also within close proximity of Development Plan 2004 - 2010 the site is Mount Merrion Monkstown Dun Laoghaire Kilnam anagh Dundrum N7 Te m p leogue Tallaght Stillorgan Sandyford Dalkey Firhouse Deasgrange Ballinteer Saggart Oldbaw n Salynoggi l n the Outer Ring Road which connects the N4 Zoned under Objective EP3 ie."to provide Foxr ock Le opar dstown N81 N11 Edm onstown Cabinteely Killiney to the N7. -

6 Tyrconnell Road, Inchicore, Dublin 8
FOR SALE BY PRIVATE TREATY 6 TYRCONNELL ROAD, INCHICORE, DUBLIN 8 MIXED USE RESIDENTIAL LED INVESTMENT (TENANTS NOT AFFECTED) 6 TYRCONNELL ROAD, INCHICORE, DUBLIN 8 ‘Fully Let Residential Led Investment’ EXECUTIVE SUMMARY Recently completed multi-unit development Consisting of 3 x apartments and an own door ground floor office unit Situated in vibrant Inchicore Village in Dublin 8 Ground floor office let to Dublin City Council (lease expiry June 2025) Total contracted rent of €115,200 per annum Guide price €1,650,000 Attractive initial yield of 6.98%. 6 TYRCONNELL ROAD, INCHICORE, DUBLIN 8 LOCATION DESCRIPTION The subject property occupies a prominent location on The subject property comprises a recently completed mixed-use Tyrconnell Road, adjacent to many local amenities and building incorporating office use at ground floor level with established businesses as well as being in an established residential accommodation on both the first and second floors. residential area. Inchicore village is situated 1 km away with The ground floor which is currently occupied by Dublin City Heuston Station, St. James Hospital and the National Children’s Council provides for a recently completed own door office suite. Hospital all within close proximity. Access to the residential accommodation is via an own door The Luas Red Line serves the Inchicore area with stops at entrance situated to the left-hand side of the office Drimnagh and Blackhorse, both situated approximately 850 accommodation. Access to the first floor is via a passenger lift meters from the subject property. Various Dublin Bus routes and stair-well servicing each floor. The first-floor layout provides also serve the area and pass through Tyrconnell Road providing for a one-bedroom apartment and a two-bedroom apartment access to Dublin City Centre within 20 minutes. -
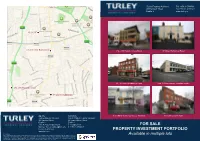
FOR SALE PROPERTY INVESTMENT PORTFOLIO Available in Multiple Lots
near Ranelagh — Dublin Turley Property Advisors Tel +353 1 4791500 89 Harcourt Street Fax +353 1 4791501 Dublin 2 www.turley.ie 13 S.C.R 23-25 Lower Rathmines 294 - 298 Harold’s Cross Road 97 Upper Rathmines Road 23 - 25 Lower Rathmines Road Unit 13 Goldenbridge Industrial Estate 294-298 Harolds Cross 97 Upper Rathmines 0 250 500 750 m Agents Solicitors 8 & 9 Main Street, Gorey, Co. Wexford 13 South Circular Road Turley Property Advisors Smyth O’Brien Hegarty Solicitors 89 Harcourt Street 24 Lower Abbey Street 1 of 1 Dublin 2 Dublin 1 Jack Brady [email protected] e: [email protected] FOR SALE Michael Turley [email protected] t: + 353 1 874 6627 t: +353 1 479 1500 PROPERTY INVESTMENT PORTFOLIO www.turley.ie DISCLAIMER Available in multiple lots These particulars are issued strictly on the understanding that they do not form part of any contract. Maps and Plans are not drawn to scale and measurements are approximate. Intending purchasers must satisfy themselves as to the accuracy of details given to them either verbally or part of this brochure. Such information is given in good faith and is believed to be correct, however the vendors or their agents shall not be liable for inaccuracies. All maps produced by permission of Ordnance Survey Ireland licence No. 00440044 Government of Ireland. 294 – 298 Harold’s Cross Road, Harold’s Cross, Dublin 6W 97 Upper Rathmines Road, Dublin 6 DESCRIPTION DESCRIPTION Constructed in 2008, this property comprises a throughout. To the rear of the property there is Number 97 comprises a pre-63, double fronted; two The property itself is situated on the corner of the purpose built mixed-use investment property, which parking for 4 cars. -

Electoral (Amendment) Act (2009)
———————— Number 4 of 2009 ———————— ELECTORAL (AMENDMENT) ACT 2009 ———————— ARRANGEMENT OF SECTIONS PART 1 Preliminary and General Section 1. Short title, collective citations and construction. 2. Interpretation. PART 2 Da´ il Constituencies and Number of Members 3. Number of members of Da´il E´ ireann. 4. Constituencies. 5. Number of members to be returned for constituency. 6. Repeal. PART 3 European Parliament Constituencies and Number of Members 7. Amendment of section 15 of European Parliament Elections Act 1997. 8. Substitution of Third Schedule to European Parliament Elec- tions Act 1997. PART 4 Constituency Commission 9. Substitution of Part II of Electoral Act 1997. 1 [No. 4.]Electoral (Amendment) Act 2009. [2009.] PART 5 European Parliament Elections 10. Substitution of sections 12 and 13 of European Parliament Elections Act 1997. 11. Substitution of rules 2 to 5 of Second Schedule to European Parliament Elections Act 1997. 12. Substitution of rule 13 of Second Schedule to European Par- liament Elections Act 1997. 13. Amendment of rules 17 and 88 of Second Schedule to Euro- pean Parliament Elections Act 1997. 14. Amendment of Schedule to Electoral Act 1997. PART 6 Local Elections 15. Substitution of articles 11 to 20 of Local Elections Regulations. 16. Amendment of article 83 of Local Elections Regulations. 17. Amendment of article 84 of Local Elections Regulations. 18. Amendment of article 86 of Local Elections Regulations. 19. Amendment of Local Elections (Disclosure of Donations and Expenditure) Act 1999. 20. Confirmation of Local Elections Regulations. SCHEDULE ———————— Acts Referred to Civil Service Regulation Acts 1956 to 2005 Electoral (Amendment) Act 2005 2005, No. -

KILMAINHAM-INCHICORE DEVELOPMENT STRATEGY Contents
KILMAINHAM-INCHICORE DEVELOPMENT STRATEGY Contents 1. INTRODUCTION 4 2. THEMES 6 3. STAKEHOLDER ENGAGEMENT 16 4. VISION 24 5. REGENERATION FRAMEWORK 28 6. URBAN REGENERATION & 40 DEVELOPMENT FUND 7. DELIVERY & PARTNERSHIPS 50 APPENDIX I - SPATIAL ANALYSIS APPENDIX II - MOVEMENT ANALYSIS APPENDIX III - LINKAGE ANALYSIS APPENDIX IV - NIAH SITES / PROTECTED STRUCTURES 1. INTRODUCTION KILMAINHAM-INCHICORE DEVELOPMENT STRATEGY Dublin City Council’s Kilmainham-Inchicore funding as Category “A” Projects under the Development Strategy is a non-statutory next round of the URDF later in 2021. high level study funded as a Category “B” This section sets out the basis for the Study under Call 1 of the (then) Department If Dublin City Council is successfully awarded of Housing, Planning and Local Government’s financing under the URDF it will be enabled Development Strategy, its purpose and (DHPLG) Urban Regeneration Development to undertake further detailed studies and Fund (URDF) to address opportunities for assessments of the projects before advancing what it attempts to achieve. urban regeneration and placemaking in to the planning consent process, detailed the Kilmainham-Inchicore area. The URDF design, and construction. application process is local authority led, prepared by the Executive. and determined The projects identified in the Development by the Minister for Housing and Local Strategy will be subject to a statutory Government (the Minister). The Development planning consent under the Planning and Strategy provides a framework for integrated, Development Act 2000 (as amended). All plan-led solutions, but does not authorise projects will be assessed concerning their specific projects. environmental impacts as part of a planning application. This includes compliance with The Development Strategy has been the Environmental Impact Assessment, Flood informed by the compilation of a Baseline Risk, and Habitats Directives. -

St. Michael's Parish Inchicore
St. Michael’s Parish Parish Priest: Fr. Louis McDermott OMI, Parish Secretary: Mrs. Pat Whelan St. Michael’s Parish Youth Worker: Padraig Corcoran Child Safeguarding Reps: Walter Balfe & Philomena McSorley 52a & 52b Bulfin Rd, Inchicore, Dublin 8. Tel 453 1660 Inchicore Parish Office: Mon-Fri: 9.30-12.30 Email: [email protected] www.stmichaelsinchicore.ie Weekday Mass: (Mon-Fri) 10am 18th November 2018 Liturgy of the Word & Communion Service on Wednesdays 10am 33rd Sunday of the Year Sunday Mass: 6.30pm (Vigil), 9am & 11am (Family Mass) We are in the final Sundays of the year with this Sunday being the second The church is open from 9am-12.00pm: Monday—Friday. last of the church liturgical year. It could be said that the church year re- flects the circle of life that we all experience, the ordinary and the extraor- Inchicore Environmental Group invite you to join them this Saturday dinary, births, deaths, joys and sorrow. The Gospel readings throughout morning, 17th for a canal clean up. Meeting B.E.R.A. hall 10am. the year are reminders of God’s presence in all our various living experience as we come together as church to encourage & support each other. Our Lady’s Hospice Partners in Faith Harold’s Cross CIRCLES OF HOPE Light up a Life 25th November: Feast of Christ the King Winter Reflection Day Sunday, 2nd December 2nd December: 1st Sunday of Advent Saturday, 8th December, This year the Hospice are delighted to wel- 10am-4pm. come a very special guest, Dublin’s own Sophia Centre, Cork St. -

History the History of Our School Is Very
History The history of our school is very much linked with the history of the locality and particularly with that of the Inchicore Railway. The establishment of the school was a direct response to the needs of the area at the time. It was built on the site of what was the Cow and Calf Inn. Let’s journey back a little in time! The year is 1729. An Act of Parliament in this year established Ireland’s first turnpike or toll road. It went from James’ Street through Kilmainham and Inchicore, past the Cow and Calf Inn to Kilcullen, County Kildare. The Kilcullen Road Company – a Turnpike Trust – maintained this road. In turn the Trust charged toll fees at various gates along this road. Sample fees for 1787 were as follows: A coach with 4 horses was charged 1 shilling (5 pence) per horse A horse and cart was charged 1 old penny A horse only was charged 1 old penny Droves of domestic animals were charged various amounts per score (20) In fact the Cow and Calf Inn was situated at a very important road junction. A second Turnpike road, operated by The Mullingar Road Company between 1786 and 1854, went along Inchicore Road, also passing by the Cow and Calf Inn, through lower Ballyfermot and Palmerstown. In the early 1800’s Inchicore was an area of fields and pastures. The Cow and Calf Inn was on land owned by Lord Cloncurry. Nearby was the Cow and Calf farm, which stretched along Grattan Crescent and lower Tyrconnell Road.