Board Paper Template
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Integration Joint Board 13Th September 2018 Mental Welfare Commission Themed Visit to People with Dementia in Community Hospital
Integration Joint Board 13th September 2018 Subject: Mental Welfare Commission Themed Visit to people with dementia in Community Hospitals Purpose: To provide an update as to the feedback from the Mental Welfare Commission (MWC) on their announced inspection visits to people with dementia in community hospitals, highlighting areas of good practice noted and recommendations made for areas of required improvement. Recommendation: Integrated Joint Board (IJB) members to please note the content of the report and consider the implementation of the supporting action plan which has been developed in response to the recommendations of the above noted report. Glossary of Terms AWI Adults with Incapacity IJB Integration Joint Board HSCP Health & Social Care Partnership MWC Mental Welfare Commission NHSAA NHS Ayrshire & Arran 1. EXECUTIVE SUMMARY 1.1 In May 2018 the MWC for Scotland published the “Visiting and monitoring report: Themed Visit to people with dementia in community hospitals” (Appendix 1). The report provides a picture of the experience of patients and carers in community hospitals across Scotland and contains twelve recommendations for IJB’s around improving the care provided within community hospitals, whilst also highlighting areas of good practice. 1.2 Community Hospital Ward Environments: Although ward environments visited were generally found to be clean and in good decorative order, the findings of the report were that more work could be done to make environments more dementia friendly. Furthermore, although there was a strong focus on physical rehabilitation within ward environments, the overall picture was of very limited meaningful and stimulating activity for people with dementia. Wards areas that had access to specialist dementia services and/or a dementia champion were found to display clear benefits in terms of supporting the development of good practice in dementia care. -

Discharges from NHS Hospitals to Care Homes Between 1 March and 31 May 2020
Discharges from NHS Hospitals to Care Homes between 1 March and 31 May 2020 Validated register of hospital discharges to care homes methodology Publication date: 28 October 2020 Revised 21 April 2021 A Management Information release for Scotland Public Health Scotland This is a Management Information publication Published management information are non-official statistics which may be in the process of being transitioned into official statistics. They may not comply with the UK Statistics Authority’s Code of Practice with regard to high data quality or high public value but there is a public interest or a specific interest by a specialist user group in accessing these statistics as there are no associated official statistics available. Users should therefore be aware of the aspects of data quality and caveats surrounding these data, all of which are listed in this document. Find out more about Management Information publications at: https://code.statisticsauthority.gov.uk/national-statisticians-guidance-management-information- and-official-statistics-3/ 1 Public Health Scotland Contents Revisions ................................................................................................................................. 4 Introduction .............................................................................................................................. 5 Identifying People Discharged to a Care Home ........................................................................... 5 Section 1 – Discharges from NHSScotland Hospitals -

Contract Between Scottish Ministers
CONTRACT BETWEEN SCOTTISH MINISTERS AND GEOAMEY PECS LTD FOR THE SCOTTISH COURT CUSTODY AND PRISONER ESCORT SERVICE (SCCPES) REFERENCE: 01500 MARCH 2018 Official No part of this document may be disclosed orally or in writing, including by reproduction, to any third party without the prior written consent of SPS. This document, its associated appendices and any attachments remain the property of SPS and will be returned upon request. 1 | P a g e 01500 Scottish Court Custody and Prisoner Escort Service (SCCPES) FORM OF CONTRACT CONTRACT No. 01500 This Contract is entered in to between: The Scottish Ministers, referred to in the Scotland Act 1998, represented by the Scottish Prison Service at the: Scottish Prison Service Calton House 5 Redheughs Rigg Edinburgh EH12 9HW (hereinafter called the “Purchaser”) OF THE FIRST PART And GEOAmey PECS Ltd (07556404) The Sherard Building, Edmund Halley Road Oxford OX4 4DQ (hereinafter called the “Service Provider”) OF THE SECOND PART The Purchaser hereby appoints the Service Provider and the Service Provider hereby agrees to provide for the Purchaser, the Services (as hereinafter defined) on the Conditions of Contract set out in this Contract. The Purchaser agrees to pay to the Service Provider the relevant sums specified in Schedule C and due in terms of the Contract, in consideration of the due and proper performance by the Service Provider of its obligations under the Contract. The Service Provider agrees to look only to the Purchaser for the due performance of the Contract and the Purchaser will be entitled to enforce this Contract on behalf of the Scottish Ministers. -

Accident and Emergency: Performance Update
Accident and Emergency Performance update Prepared by Audit Scotland May 2014 Auditor General for Scotland The Auditor General’s role is to: • appoint auditors to Scotland’s central government and NHS bodies • examine how public bodies spend public money • help them to manage their finances to the highest standards • check whether they achieve value for money. The Auditor General is independent and reports to the Scottish Parliament on the performance of: • directorates of the Scottish Government • government agencies, eg the Scottish Prison Service, Historic Scotland • NHS bodies • further education colleges • Scottish Water • NDPBs and others, eg Scottish Police Authority, Scottish Fire and Rescue Service. You can find out more about the work of the Auditor General on our website: www.audit-scotland.gov.uk/about/ags Audit Scotland is a statutory body set up in April 2000 under the Public Finance and Accountability (Scotland) Act 2000. We help the Auditor General for Scotland and the Accounts Commission check that organisations spending public money use it properly, efficiently and effectively. Accident and Emergency | 3 Contents Summary 4 Key messages 7 Part 1. A&E waiting times 9 Part 2. Reasons for delays in A&E 20 Part 3. Action by the Scottish Government 37 Endnotes 41 Appendix 1. NHS Scotland A&E departments and minor injury units 43 Appendix 2. National context for A&E and unscheduled care, 2004 to 2014 45 Exhibit data When viewing this report online, you can access background data by clicking on the graph icon. The data file will -

Candidate Information Pack Post Title: Consultant Physician in Gastroenterology
Our purpose Working together to achieve the healthiest life possible for everyone in Ayrshire and Arran Candidate information pack Post title: Consultant Physician in Gastroenterology University Hospital Ayr Follow us on Twitter @NHSaaa Find us on Facebook at www.facebook.com/nhsaaa Visit our website: www.nhsaaa.net All our publications are available in other formats Section one: About NHS Ayrshire & Arran NHS Ayrshire & Arran is one of 14 territorial NHS Boards within NHSScotland. Ayrshire and Arran NHS Board is responsible for the protection and improvement of the local population’s health and for the delivery of frontline healthcare services. The NHS Board membership consists of executive and non-executive members, and is accountable to the Cabinet Secretary for Health, Wellbeing and Sport. Our operational frontline services are provided through four distinct operational units – Acute Services and the Health and Social Care Partnerships in East, North and South Ayrshire. You can find further detail on the role of the NHS Board, and our organisational structure on our website – www.nhsaaa.net. NHS Ayrshire & Arran serves a mixed rural and urban population of 376,000. We have a full range of primary and secondary clinical services, covering the mainland of Ayrshire and the islands of Arran and Cumbrae. NHS Ayrshire & Arran covers three local authority areas: East, North and South Ayrshire. There are major areas of widespread deprivation and social exclusion in both rural and urban areas. The healthcare challenge within the area is considerable: our population suffers higher than average rates of coronary heart disease, lung cancer, respiratory illnesses and premature death among males. -

Strategic Plan 2016
Strategic Plan Let’s deliver 2018–21 care together North Ayrshire Health and Social Care Follow us on Twitter @NAHSCP For more information go to www.NAHSCP.org Foreword It is with great pleasure that I share our new The joining-up (integration) of community based health and social North Ayrshire health and social care strategic care services is still in its infancy and we have much to do in order to plan 2018–21. It is designed to build upon the create services that will best support the people of North Ayrshire. progress that has been made to date and lays out The last three years have, nevertheless, seen significant advances in many areas of health and social care: our key strategic priorities for the next three years. • We developed truly integrated Universal Early Years teams to The plan has been created in partnership with better support parents of children under the age of five third and independent sector colleagues, • We opened our new hospital, Woodland View, in Irvine, which – public health, community planning partners, as well as providing two community wards for older people – is local communities and, most importantly, people primarily a state-of-the-art mental health hospital who use our services. • We have continued to develop our care at home workforce, ensuring that we can recruit and retain staff and ultimately support people to live at home • To help support local carers, we have introduced a Carers Card that offers carers discounts at local businesses • Partnership working with community planning partners has resulted in reduction in the levels of domestic violence, and more general crime, across North Ayrshire Delivering care together All our achievements to date are far too lengthy to mention here, you can find out more about the progress being made in our annual performance reports at www.nahscp.org. -

Candidate Information Pack Post Title
Our purpose Working together to achieve the healthiest life possible for everyone in Ayrshire and Arran Candidate information pack Post title: Consultant in Oralmaxillofacial Surgery Job reference number: Closing date: MD/673/19 4 March 2020 Process for submitting application: CV with supporting documentary evidence of entry GMC Specialist Register/CCT or CESR date, together names and email addresses of 2 referees inc most recent Educational Supervisor or Clinical Director submitted to: [email protected] . Interviews have been scheduled for 30 March 2020 Follow us on Twitter @NHSaaa Find us on Facebook at www.facebook.com/nhsaaa Visit our website: www.nhsaaa.net All our publications are available in other formats Welcome from the Chief Executive Thank you for the interest you have shown in this post. I hope that the information in this pack will help you to decide and encourage you to apply for this post. In recent years we have re-defined the purpose and values that are the foundation for our approach to health and social care delivery. You will find more information on our purpose and values in this pack. As with other health and social care providers, we are delivering our services in challenging times. Demographic changes, increasing demand and wider socio-economic factors all impact on service delivery. We are committed to working together with our teams and communities to re-design services to meet these challenges and fulfil our purpose. Delivering high quality, safe, person-centred care to every person every time is our clear aim. This can only be achieved when our staff feel valued and fully engaged. -

March 2017 Contents ** Please Note That Some of the Links in This Document Are to Items on Athena, NHS Ayrshire & Arran's
March 2017 Contents • Staff awards and achievements • NHS Board update – 27 March 2017 • Ayrshire Achieves Chief Executive’s and Chairman’s reports • Quality improvement in action award Quality • Bowel cancer annual event Service • Green Gym Performance • MAST Decision / approval • Changes to salary from 1 April 2017 Minutes Next meeting Keep sending your news to [email protected] ** Please note that some of the links in this document are to items on AthenA, NHS Ayrshire & Arran’s intranet, and so may not work for external users. If you require a copy of any information, please email [email protected] ** Staff awards and achievements Queen’s Nurse title for local community nurse An Ayrshire community nurse has been selected to take part in a special professional development programme that will earn them the right to use the coveted Queen’s Nurse title. Barbara McFadzean, who works in East Ayrshire Health and Social Care Partnership, is one of 20 community nurses selected by The Queen’s Nursing Institute Scotland (QNIS) to join the first cohort of 21st century Queen’s Nurses. On completion of the programme, Barbara will be one of the first nurses to receive the title in Scotland for almost 50 years. Advancing Healthcare Award Fiona McMillan, Head of Clinical Physiology and Catrina MacGregor, Healthcare Science Lead have won a major UK award for their achievement in streamlining testing for heart failure and ensuring patients get more rapid diagnosis and treatment. They were presented with the Scottish Government’s award for driving improvement, delivering results for their approach to innovative service design to improve the patient experience and achieve earlier diagnosis. -
Scotland) Act 1973 (Copy Enclosed)
Cunninghame House Irvine 06 August 2015 Integration Joint Board You are requested to attend a meeting of the Integration Joint Board to be held on Thursday 13 August 2015 at 10.00 a.m. in the Council Chambers, Cunninghame House, Irvine, to consider the following business. Business 1. Apologies Invite intimation of apologies for absence. 2. Declaration of Interest 3. Minutes / Action Note (Page 5) The accuracy of the Minutes of the meeting held on 4 June 2015 will be confirmed and the Minutes signed in accordance with Paragraph 7 (1) of Schedule 7 of the Local Government (Scotland) Act 1973 (copy enclosed). 4. Matters Arising Reports for Approval 5. Performance and Audit Committee (Page 15) Submit report by Lesley Aird, Head of Finance, on the membership and meeting schedule for the Performance and Audit Committee of the IJB (copy enclosed). 6. Model Publication Scheme (Page 17) Submit report by Neil McLaughlin, Information Systems Manager, on the requirement to define how information is made publically accessible (copy enclosed). Reports to Note 7. Director's Report (Page 21) Submit report by Iona Colvin, Director, on developments within the North Ayrshire Health and Social Care Partnership (copy enclosed). 8. GP Strategy (Page 33) Submit report by Dr Paul Kerr, Clinical Director Health and Social Care Partnership on the document General Practice in Ayrshire and Arran: A Vision for Change (copy enclosed). 9. Care at Home Review Update (Page 65) Submit report by David Rowland, Head of Service Health & Community Care, on the progress that has been made by Main Street Consulting in conducting a review of Care at Home Services (copy enclosed). -
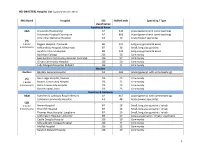
MASTER) Hospital List (Updated October 2015
HEI (MASTER) Hospital List (updated October 2015) NHS Board Hospital ISD Staffed beds Speciality / Type classification Ayrshire & Arran A&A University Hospital Ayr A2 343 Acute (general with some teaching) University Hospital Crosshouse A2 666 Acute (general with some teaching) Arran War Memorial Hospital A3 19 Acute (mixed speciality) (9) 3 acute Biggart Hospital, Prestwick B6 121 Long stay geriatric & acute 6 community Kirklandside Hospital, Kilmarnock B7 36 Small, long stay geriatric Ayrshire Central Hospital B8 142 Long stay geriatric & acute Davidson Cottage J26 26 Community East Ayrshire Community Hospital, Cumnock J26 57 Community Girvan Community Hospital J26 20 Community Lady Margaret Hospital, Millport J26 9 Community Borders Borders Borders General Hospital A2 265 Acute (general, with some teaching) (5) Hay Lodge Hospital, Peebles J26 23 Community 1 acute Hawick Community Hospital J26 22 Community 4 community Kelso Community Hospital J26 23 Community Knoll Hospital, Duns J26 23 Community Dumfries & Galloway D&G Dumfries & Galloway Royal Infirmary A2 367 Acute (general, with some teaching) Galloway Community Hospital A3 48 Acute (mixed speciality) (10) 2 acute Annan Hospital B7 18 Small, long stay geriatric / rehab 8 community Thornhill Hospital B7 13 Small, long stay geriatric / rehab Thomas Hope Hospital, Langholm B7 10 Small, long stay geriatric / rehab Lochmaben Hospital, Lockerbie B9 17 Long stay geriatric / rehab / psychiatry Castle Douglas Hospital J26 19 Community Kirkcudbright Cottage Hospital J26 9 Community Moffat Hospital J26 12 Community Newton Stewart Hospital J26 19 Community 1 HEI (MASTER) Hospital List (updated October 2015) Fife Fife Victoria Hospital, Kirkcaldy A2 621 Acute (general with some teaching) (7) Queen Margaret Hospital, Dunfermline A3 196 Acute (mixed speciality) 2 acute 5 community Cameron Hospital, Leven B7 95 Small, long stay geriatric Adamson Hospital, Cupar J26 19 Community Glenrothes Hospital J26 74 Community Randolph Wemyss Memorial Hospital J26 16 Community St. -

Site Code Site Name Address Address2 Town Post Code Tenure
Site Code Site Name Address Address2 Town Post Code Tenure Organisation A210H Ayr Hospital Dalmellington Road Ayr KA7 3UB Owned NHS Ayrshire & Arran A103H Ayrshire Central Hospital Ayrshire Central Hospital Kilwinning Road Irvine KA12 8TJ Owned NHS Ayrshire & Arran A111H Crosshouse Hospital 59A Kilmarnock Road Crosshouse Kilmarnock KA2 0BD Owned NHS Ayrshire & Arran A211B Drongan Resource Centre 21A Mill Of Shield Road Drongan KA6 7BA Owned NHS Ayrshire & Arran A204B Girvan Health Centre 109A Henrietta Street Girvan KA26 9AN Owned NHS Ayrshire & Arran A206H Holmhead Hospital Holmhead Cumnock KA18 1RR Owned NHS Ayrshire & Arran A110H Lady Margaret Hospital College Street Millport KA28 0HF Owned NHS Ayrshire & Arran A218C Muirkirk Clinic Glasgow Road Muirkirk KA18 3RQ Owned NHS Ayrshire & Arran A278B Patna Health Centre Doonside Avenue Patna KA6 7LX Owned NHS Ayrshire & Arran A201H Ailsa Hospital Dalmellington Road Ayr KA6 6AB Owned NHS Ayrshire & Arran A024B Dailly Surgery Owned NHS Ayrshire & Arran A026B Lochranza Newton Road Lochranza KA27 8HQ Owned NHS Ayrshire & Arran A101H Arran War Memorial Margnaheglish Road Lamlash KA27 8LF Owned NHS Ayrshire & Arran A104B Stewarton Health Centre 46 High Street Stewarton KA3 5BP Owned NHS Ayrshire & Arran A105B Townhead Surgery, Irvine Owned NHS Ayrshire & Arran A105H Kirklandside Hospital Kirklandside Kilmarnock KA1 5LH Owned NHS Ayrshire & Arran A106B Stevenston Health Centre Main Street Stevenston KA20 3AB Owned NHS Ayrshire & Arran A107B Saltcoats Health Centre 19 Raise Street Saltcoats KA21 -

Property and Asset Management Strategy (PAMS)
2015/16 Property and Asset Management Strategy (PAMS) Image 1 - Artist Impression of NACH Scheme (Source: Balfour Beatty) Working together to NHS Ayrshire & Arran achieve the healthiest life possible for everyone in DRAFT 9 Ayrshire and Arran 17/06/2015 Property and Asset Management Strategy (PAMS) Contents Contents .............................................................................................................................. 2 1. Executive Summary ....................................................................................... 5 2. Introduction .................................................................................................... 7 3. Where are we now? ...................................................................................... 10 3.1. NHS Ayrshire and Arran ................................................................................................. 10 3.1.1. Health and Social Care Partnerships .............................................................................. 11 3.2. Current Developments................................................................................................... 13 3.2.1. Building for Better Care ................................................................................................. 13 3.2.2. Woodland View (Formerly Adult Acute Mental Health Community Hospital, NACH) .. 15 3.2.3. Focus for Investment – Property ................................................................................... 18 3.2.4. Disinvestment and Sales ...............................................................................................