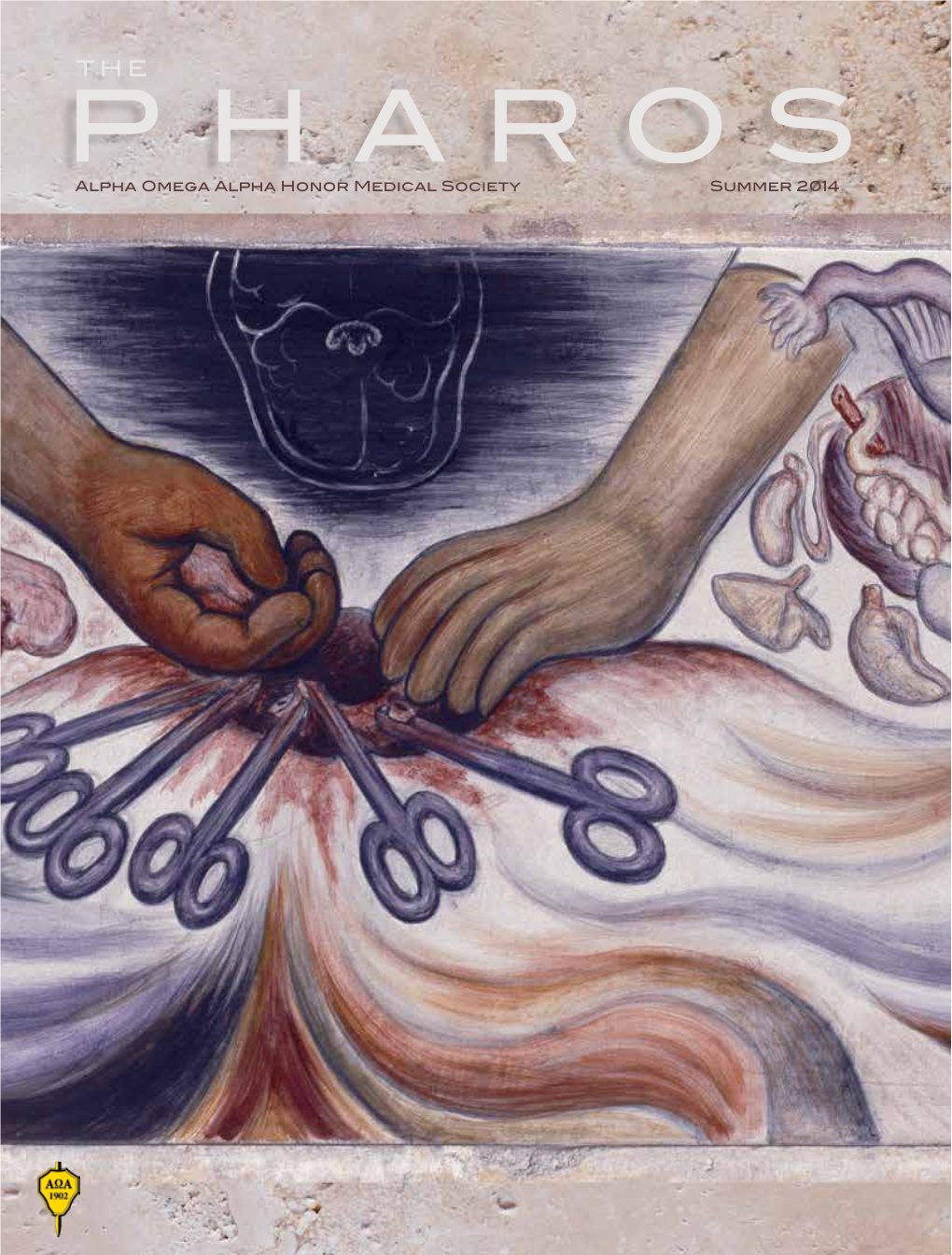
Alpha Omega Alpha Honor Medical Society Summer 2014
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Kingdom of the Monarchs Mexico Tour
For More Information Contact See More Tours at Cynthia Marion - 214.497.4074 www.travelphiletours.com KINGDOM OF THE MONARCHS MEXICO TOUR Benefiting Wimberley’s EmilyAnn Theatre & Gardens Friday February 9-Thursday February 15, 2018 7 Days / 6 Nights LEAVING FROM WIMBERLEY Enjoy our exciting ecological and cultural adventure. Fall in love with the Monarchs as you spend 2 days including Valentines day with tens of millions of Monarch butterflies! Experience one of the world’s most astounding natural events featuring the delicate Monarch at two different sanc- tuaries in Mexico where they “winterize” prior to making a remarkable springtime 3,000 mile journey to the northeastern US and Canada. Along the way we’ll take a boat ride with a local birding expert through floating gardens and canals of Xochimilco and explore Coyoacán, one of the most well preserved colonial areas of Mexico City to experience the art and culture of artists Frida Kahlo and Diego Rivera. Day 1 Texas to Mexico City Friday February 9 Depart Texas for Mexico City and the wonders that await. Upon arrival, we’ll transfer to our 4 ½ Star Tripadvisor rated hotel where you’ll have free time to get settled in your hotel room. We gather this evening for a welcome dinner at the award-winning Taberna del Leon. (D) Hotel: Paraiso See More Tours at For More Information Contact www.travelphiletours.com Cynthia Marion - 214.497.4074 Day 2 Mexico City Saturday February 10 Breakfast. Leave for one of the best handicrafts market in all of Mexico, Bazaar Del Sabado in San Angel. -

Sistema De Memoria Colectiva En El Metro Imagotipos En La Ciudad De México*
INVESTIGACIÓN 9 Sistema de memoria colectiva en el Metro Imagotipos en la Ciudad de México* Francisco López Ruiz Resumen El Sistema de Transporte Metropolitano (Metro) de la Ciudad de México ofrece un valor simbólico único en el mundo. Desde hace cuatro décadas las estaciones del Metro son representadas mediante íconos o imagotipos. El objetivo de este artículo es contrastar las características gráficas de dos imagotipos y la vinculación con su contexto urbano e histórico: los ideogramas de las estaciones La Noria (tren ligero) y Cuatro Caminos (línea 2 del Metro). El argumento central establece que los imagotipos del Metro y otros sistemas de transporte capitalino forman parte de la riqueza patri- monial y la identidad de la Ciudad de México, ya que simbolizan de manera creativa diversos elementos culturales y urbanos. Abstract Mexico City’s subway icons are unique examples of urban graphic design. The purpose of this essay is to compare two icons –La Noria (urban train) and Cuatro Caminos (subway)– and analyze their historical and cultural meaning or significance. The main argument is that such subway icons stand as symbols of Mexico City’s cultural heritage insofar they represent diverse cultural and urban elements. * Esta investigación pertenece al proyecto Energía y arquitectura sustentable, financiado por la Dirección de Investigación de la, Universidad Iberoamericana, Ciudad de México y el Patronato Económico de la misma universidad (FICSAC). 10 Francisco López Ruiz arquitectos, con lo cual se evita la fealdad El ingeniero Bernardo -
Focus on Art: the Spirit of Frida
focus on art: the spirit of frida Experience the sights, sounds, tastes and art that influenced a woman who challenged the world of art and polite society, Frida Kahlo. April 18 – 25 2017 or April 18-28, 2017 extension option trip details Travel with Hank & Laura Hine to Mexico to explore the world of Frida Kahlo, her art, and her tumultuous life with husband, partner and obsession Diego Rivera. Mexico City San Miguel de Highlights Allende Highlights Welcome dinner at Trolley touring Restaurant Café Tacuba Walking tour of galleries National Folkloric and shopping at Ballet performance Fábrica La Aurora Frida’s Casa Azul Guided visit to ‘the Sistine Chapel of the Americas’ The House Museum of Dolores Olmedo Folk art museum Soumaya Museum Special farewell dinner Guided visits to Rivera’s works Fine dining throughout Xilitla and Guanajuato Optional Extension Highlights Tour through spectacular Sierra Gorda; 2 nights in the El Castillo and La Posada de James; Edward James’ jungle sculpture garden; bath, waterfall and natural pools of Las Pozas; Diego Rivera’s house and museum; soiree with troubadours. Cost: $4,694* per person, double occupancy; single travelers add $1,069 Optional 4-day/3-night Extension add $1,259 per person double occupancy, single travelers add $350 more *Your price includes a $500 per person tax-deductible honorarium to The Dalí Museum. Details to follow. A deposit of $500 per person, a and membership with The Dalí Museum, are required to hold your space. Final payment is due January 18, 2017 price includes Main program: -

Mexico City and San Miguel De Allende SCHEDULE BY
An Art Lover’s Mexico: Mexico City and San Miguel de Allende October 19-26, 2018 Immerse yourself in the art, architecture, and cuisine of Mexico on this tour of Mexico City and San Miguel de Allende. Begin in Mexico City’s colonial center, touring the city's spectacular murals and dramatic architecture. Enjoy traditional home cooking at the Casa Pedregal, designed by notable Mexican architect Luis Barragán. See the Torres de Ciudad Satélite, an iconic piece of modern sculpture and architecture. In San Miguel de Allende, meander along narrow cobblestone streets, and view colorful arcades and courtyards, rustic houses, and elegant mansions. Conclude with a visit to El Charco del Ingenio botanical gardens to see migrating birds, serene waterfalls, and lush landscapes. GROUP SIZE: From 16 to 30 travelers PRICING: $4,995 per person double occupancy / Single supplement: $1,295 STUDY LEADER: JEFFREY QUILTER is the William and Muriel Seabury Howells Director of the Peabody Museum of Archaeology and Ethnology and senior lecturer in anthropology at Harvard. Trained as an anthropological archaeologist, Jeffrey has focused much of his career on the early societies of Peru. Recently, his interest in issues of the origins and nature of complex societies has shifted to a focus on viewing social and environmental changes over long periods of time. ____________________________________________________________________________________________ luxurious hotel, located near Chapultepec SCHEDULE BY DAY Park. B=Breakfast, L=Lunch, D=Dinner, R=Reception After checking into your hotel, drive to the National Museum of Anthropology to see FRIDAY, OCTOBER 19 exquisite sculptures and artifacts from ARRIVE MEXICO CITY Mexico’s pre-Columbian civilizations. -

Rediseño Del Manual De Capacitación Para Guías Temporales Del Museo Dolores Olmedo
UNIVERSIDAD PEDAGÓGICA NACIONAL Unidad Ajusco Licenciatura en Psicología Educativa Informe de intervención profesional Rediseño del manual de capacitación para guías temporales del Museo Dolores Olmedo Tesis Que para obtener el título de Licenciado en Psicología Educativa Presenta: Luis Antonio Jimenez Velazquez Asesora Dra. Mónica García Hernández Ciudad de México 2017 Agradecimientos A mis padres Teresa Velazquez y Luis Jimenez: Por todo el esfuerzo, paciencia y apoyo que me han brindado, sé que no he sido un hijo ejemplar pero gracias a sus consejos pude concluir esta etapa de mi vida. A Evelin y Leonardo: Hermana, sé que no siempre nos llevamos bien, pero te agradezco todo lo que haces por mí, es divertido compartir la vida contigo. Leo, espero siempre tengas una vida interesante en todo aspecto, goza, disfruta y se feliz creciendo. Los amo. A Jacinta López y Antonio Badillo y a sus hijos Karina, Celene, Gloria, Ivonne y Marcos: Porque son parte de mi familia nuclear y siempre han estado al pendiente de mí en todo aspecto de la vida. Gracias, pocas personas tienen la dicha de rodearse de tan buenas personas. A mi familia de Guanajuato: Son el perfecto escape de la rutina de esta ciudad. Los quiero. A Karen: ¿Quién pensaría que una obra de mi infancia, que comprendí años después, resultaría un punto de encuentro para ambos? (Le Petit Prince). A lo largo de estos años te has convertido en una pieza esencial de mi vida, te has vuelto parte de mi familia y más, gracias por estar a mi lado. A la Doctora Mónica García Hernández: Por apoyarme y guiarme en la elaboración de este proyecto. -

An Art Lover's
A custom-designed tour by International Seminar Design, Inc. © for Smith College An Art Lover’s MEXICO Art, Archaeological & Architectural Treasures of Mexico City & Oaxaca NOVEMBER 9–16, 2018 INTERNATIONAL SEMINAR DESIGN, INC. | 4115 Wisconsin Avenue, NW, Suite 101, Washington, DC 20016 | (202) 244-1448 | [email protected] Recommended Tour Dates: November 9–16, 2018 DAY ACTIVITY ACCOMMODATION MEALS 1 USA to Mexico City Four Seasons D.F. D 2 Mexico City Four Seasons D.F. B, L 3 Mexico City Four Seasons D.F. B, L, R 4 Mexico City to Oaxaca Quinta Real B, L, D 5 Oaxaca Quinta Real B, L, R 6 Oaxaca Quinta Real B, L 7 Oaxaca Quinta Real B, L, D 8 Departure to USA — B B = Breakfast, L = Lunch, D = Dinner, R = Reception Suggested Custom Itinerary Friday, November 9 USA / Mexico City • Fly to Mexico City. • Transfer independently to the Four Seasons D.F., Mexico City’s most luxurious five-star hotel, ideally situated by the entrance of Chapultepec Park. • In the late afternoon, gather in the hotel’s lobby and walk to the incomparable National Anthropology Museum, probably the crown jewel of all Latin American cultural institutions. Our guide will provide a whirlwind tour of the very best relics and artworks from the many civilizations that thrived in various parts of Mexico, including the Olmecs, Aztecs, Maya, and Zapotecs. • Enjoy an elegant welcome dinner in the Four Season’s superb Zanaya restaurant on the private outdoor terrace. The food is mostly seafood from the state of Nayarit. The seasonings and the local “zarandeado” cooking style place this restaurant at the top of Mexico City’s list of best places to dine. -

Mexico City: Art, Culture & Cuisine!
Mexico City: Art, Culture & Cuisine! Art History of Mexico Available Anytime! Cultural Journeys Mexico | Colombia | Guatemala www.tiastephanietours.com | (734) 769 7839 Mexico City: Art, Culture & Cuisine! Art History of Mexico On this journey of learning and discovery, we explore the history and expressions of Art in Mexico. In order to understand the vision and temperament of Diego and Frida, we will learn of History and Politics of Mexico, that is the only way to contextualize their art and lives. While Diego’s Art was overtly political, Frida’s was more personal, as we will see. The Mexican Muralism Movement will also be explored. If you are interested in Art, His- tory, Culture, Muralism, Diego and Frida, this trip is for you! Join us to explore art in Mexico City! Program Highlights • Explore the Zocalo • Visit Templo Mayor, Ceremonial Center of the Aztecs • Learn of Mexican History & Indigenous LOCATION Past at the National Palace Murals, painted by Diego Rivera • Ocotlan and the Southern Craft Route. • Visit the Palacio de Bellas Artes • Museum of Modern Art • Rufino Tamayo Museum • Frida Kahlo Museum • Dolores Olmedo Museum • UNAM Campus Itinerary Day 1: and the Cathedral of the Assumption of mural iconography and techniques of the Arrive Mexico City, Transfer to our Mary, constructed in a medley of Ba- ancient civilizations of Mexico. Diego Rivera Centrally Located Hotel and explore the roque, Neoclassical, and Mexican chur- studied the Prehispanic fresco technique to Historic Center! rigueresque architectural styles. Then we apply to his own work. (B, L) Enjoy a Light Lunch move to the National Palace to view Diego Explore the Zocalo, the Largest Square in Rivera’s mural masterpiece The Epic of the Day 3: the Americas! Mexican People, where he depicted major Today we explore the Antiguo Colegio San Visit Templo Mayor, Ceremonial Center of events in Mexico’s history, and the indig- Idelfonso, home to the first mural painted the Aztecs enous cultures of Mexico. -

Re-Thinking the Language of Pain in the Works of Marguerite Duras and Frida Kahlo
Re-thinking the Language of Pain in the Works of Marguerite Duras and Frida Kahlo Regina F. Bartolone A dissertation submitted to the faculty of the University of North Carolina at Chapel Hill in partial fulfillment of the requirement for the degree of Doctor of Philosophy in the Department of English and Comparative Literature. Chapel Hill 2006 Approved by: Dr. Martine Antle (advisor) Dr. Marsha Collins (reader) Dr. Maria DeGuzmán (reader) Dr. Dominque Fisher (reader) Dr. Diane Leonard (reader) Abstract Regina F.Bartolone Re-Thinking the Language of Pain in the Works of Marguerite Duras and Frida Kahlo (Under the direction of Dr. Martine Antle) This dissertation is a cross-cultural examination of the creation and the socio- cultural implications of the languages of pain in the works of French author, Marguerite Duras and Mexican painter, Frida Kahlo. Recent studies have determined that discursive communication is insufficient in expressing one’s pain. In particular, Elaine Scarry maintains that pain destroys language and that its victims must rely on the vocabulary of other cultural spheres in order to express their pain. The problem is that neither Scarry nor any other Western pain scholar can provide an alternative to discursive language to express pain. This study claims that both artists must work beyond their own cultural registers in order to give their pain a language. In the process of expressing their suffering, Duras and Kahlo subvert traditional literary and artistic conventions. Through challenging literary and artistic forms, they begin to re-think and ultimately re-define the way their readers and viewers understand feminine subjectivity, colonial and wartime occupation, personal tragedy, the female body, Christianity and Western hegemony. -

P20-21.Qxp Layout 1
Established 1961 21 Lifestyle Features Wednesday, December 11, 2019 t a stately museum in Mexico City, great-grandpuppies reside. tion and model to Mexican artists, it has also of Kahlo and Rivera paintings. There is a statue priceless paintings by Frida Kahlo and “Xolos,” as they are known for short, are a joined the list of icons that represent Mexican in the dogs’ honor on the museum grounds, and ADiego Rivera share pride of place with quintessentially Mexican dog. The ancient identity, such as Day of the Dead skeletons, a professional caretaker just for them. “To us, an unruly pack of hairless black dogs: Mexico’s species goes back 7,000 years and was first Frida Kahlo and the Aztec calendar,” said these dogs are living works of art, just like prized xoloitzcuintle. The 13 dogs who reside domesticated around 5,500 years ago. The Maria Olvido Moreno, an art historian at Rivera’s and Kahlo’s paintings,” said curator on the leafy grounds of the Museo Dolores Aztecs named the dog for the god of death, Mexico’s largest university, UNAM. Josefina Garcia. Olmedo are the direct descendants of ones that Xolotl, combined with “itzcuintli,” or dog. They belonged to Kahlo and Rivera, whose searingly had themselves buried with xolos so the dogs Doggy survivors ‘Coco’ and rock stars intimate portraits (her) and sprawling murals could guide them to Mictlan, the underworld Xolos lack hair - though some do have a Xolos have become cool once again in the (him) made them the towering power couple of where they believed life continued after death. -
México Mágico: Magical Mexico City Exploring the Colors of Mexican Folk Art with Marina Aguirre and Dr. Khristaan Villela
México Mágico: Magical Mexico City Exploring the Colors of Mexican Folk Art With Marina Aguirre and Dr. Khristaan Villela For the Friends of Folk Art - Santa Fe, NM September 4 – 12, 2017 Join the Friends of Folk Art and MOIFA’s Director for a special journey to Mexico Day 1 – Monday, September 4 Arrive México City in the afternoon. Transfer to our centrally located accommodations at the Best Western Majestic Hotel. Dinner on your own Day 2 – Tuesday, September 5 Breakfast at hotel is included daily Visit and tour of Museo de Arte Popular (Folk Art Museum) Lunch at Casa de los Azulejos, “House of Tiles, an 18th century palace (included) Afternoon visit to National Museum of Anthropology, one of the most important museums in the world, and home to Mexico’s national collection of Precolumbian art. Our tour will focus on Mexico’s rich indigenous arts and its connection and historic roots in Mexican folk art. There will not be time to see the entire museum. Dinner at Bonito Restaurant in the Condesa neighborhood (included) 1 Day 3 – Wednesday, September 6 Breakfast at hotel Visit to Diego Rivera’s mural “Dream of a Sunday Afternoon in Alameda Central Park” at the Museo Mural Diego Rivera. The mural provides an introduction to Mexico’s history and is an important point of reference for the work of Diego Rivera. The museum is a 30-minute walk from the hotel so you can walk or ride in the van. Visit the private collection of Ruth Lechuga at the Franz Mayer Museum. This collection is only available to scholars, and we have a rare opportunity to enjoy one of the most important folk art collections in Mexico. -
Annual Report 2004
mma BOARD OF TRUSTEES Richard C. Hedreen (as of 30 September 2004) Eric H. Holder Jr. Victoria P. Sant Raymond J. Horowitz Chairman Robert J. Hurst Earl A. Powell III Alberto Ibarguen Robert F. Erburu Betsy K. Karel Julian Ganz, Jr. Lmda H. Kaufman David 0. Maxwell James V. Kimsey John C. Fontaine Mark J. Kington Robert L. Kirk Leonard A. Lauder & Alexander M. Laughlin Robert F. Erburu Victoria P. Sant Victoria P. Sant Joyce Menschel Chairman President Chairman Harvey S. Shipley Miller John W. Snow Secretary of the Treasury John G. Pappajohn Robert F. Erburu Sally Engelhard Pingree Julian Ganz, Jr. Diana Prince David 0. Maxwell Mitchell P. Rales John C. Fontaine Catherine B. Reynolds KW,< Sharon Percy Rockefeller Robert M. Rosenthal B. Francis Saul II if Robert F. Erburu Thomas A. Saunders III Julian Ganz, Jr. David 0. Maxwell Chairman I Albert H. Small John W. Snow Secretary of the Treasury James S. Smith Julian Ganz, Jr. Michelle Smith Ruth Carter Stevenson David 0. Maxwell Roselyne C. Swig Victoria P. Sant Luther M. Stovall John C. Fontaine Joseph G. Tompkins Ladislaus von Hoffmann John C. Whitehead Ruth Carter Stevenson IJohn Wilmerding John C. Fontaine J William H. Rehnquist Alexander M. Laughlin Dian Woodner ,id Chief Justice of the Robert H. Smith ,w United States Victoria P. Sant John C. Fontaine President Chair Earl A. Powell III Frederick W. Beinecke Director Heidi L. Berry Alan Shestack W. Russell G. Byers Jr. Deputy Director Elizabeth Cropper Melvin S. Cohen Dean, Center for Advanced Edwin L. Cox Colin L. Powell John W. -

Acknowledgments
Acknowledgments The following institutions graciously granted permission to reproduce the images found in this book: the Amherst Special Collection at Amherst Col- lege, the collection of Andres Blaisten, the Archivo General del Estado de Nuevo León, the Archivo General de la Nación in Mexico City, the Biblio- teca Lerdo de Tejada, the Art Archive, the Colección Museo Dolores Olmedo, the Davis Museum at Wellesley College, the Dirección General de Activida- des Cinematográficas de la Universidad Nacional Autónoma de México, the Jacques and Natasha Gehman Collection of Mexican Art, and the Instituto Tlaxcalteca de Cultura. We also wish to thank the following institutions and individuals for permis- sion to reproduce the paintings of Diego Rivera, José Clemente Orozco, David Alfaro Siqueiros, Frida Kahlo, and María Izquierdo: the Instituto Nacional de Bellas Artes, the Banco de México, © Clemente Orozco V., Art © Estate of David Alfaro Siqueiros (somapp/vaga), Aurora Posadas Izquierdo, and Darlene Lutz. Thanks also to Sarah M. Lowe for permission to reproduce ma- terial from her book Frida Kahlo, Universe Series on Women (New York: Uni- verse, 1991) and to Natalie Hanemann for preparing the maps. Funds for the publication of this volume were provided by the Department of History and the General Research Board at the University of Maryland and by the Office of the Provost and the College of the Humanities and Fine Arts at California State University, Chico. Finally, we thank our contributors for their work and patience, and Valerie Millholland, Miriam Angress, and the editorial staff and art production staff at Duke University Press for patiently guiding this volume to publication.