Dehydroepiandrosterone, Over-Studied but Under-Used in The
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-
Amplification of Oxidative Stress by a Dual Stimuli-Responsive Hybrid Drug
ARTICLE Received 11 Jul 2014 | Accepted 12 Mar 2015 | Published 20 Apr 2015 DOI: 10.1038/ncomms7907 Amplification of oxidative stress by a dual stimuli-responsive hybrid drug enhances cancer cell death Joungyoun Noh1, Byeongsu Kwon2, Eunji Han2, Minhyung Park2, Wonseok Yang2, Wooram Cho2, Wooyoung Yoo2, Gilson Khang1,2 & Dongwon Lee1,2 Cancer cells, compared with normal cells, are under oxidative stress associated with the increased generation of reactive oxygen species (ROS) including H2O2 and are also susceptible to further ROS insults. Cancer cells adapt to oxidative stress by upregulating antioxidant systems such as glutathione to counteract the damaging effects of ROS. Therefore, the elevation of oxidative stress preferentially in cancer cells by depleting glutathione or generating ROS is a logical therapeutic strategy for the development of anticancer drugs. Here we report a dual stimuli-responsive hybrid anticancer drug QCA, which can be activated by H2O2 and acidic pH to release glutathione-scavenging quinone methide and ROS-generating cinnamaldehyde, respectively, in cancer cells. Quinone methide and cinnamaldehyde act in a synergistic manner to amplify oxidative stress, leading to preferential killing of cancer cells in vitro and in vivo. We therefore anticipate that QCA has promising potential as an anticancer therapeutic agent. 1 Department of Polymer Á Nano Science and Technology, Polymer Fusion Research Center, Chonbuk National University, Backje-daero 567, Jeonju 561-756, Korea. 2 Department of BIN Convergence Technology, Chonbuk National University, Backje-daero 567, Jeonju 561-756, Korea. Correspondence and requests for materials should be addressed to D.L. (email: [email protected]). NATURE COMMUNICATIONS | 6:6907 | DOI: 10.1038/ncomms7907 | www.nature.com/naturecommunications 1 & 2015 Macmillan Publishers Limited. -

Cinnamaldehyde Induces Release of Cholecystokinin and Glucagon-Like
animals Article Cinnamaldehyde Induces Release of Cholecystokinin and Glucagon-Like Peptide 1 by Interacting with Transient Receptor Potential Ankyrin 1 in a Porcine Ex-Vivo Intestinal Segment Model Elout Van Liefferinge 1,* , Maximiliano Müller 2, Noémie Van Noten 1 , Jeroen Degroote 1 , Shahram Niknafs 2, Eugeni Roura 2 and Joris Michiels 1 1 Laboratory for Animal Nutrition and Animal Product Quality (LANUPRO), Department of Animal Sciences and Aquatic Ecology, Ghent University, 9000 Ghent, Belgium; [email protected] (N.V.N.); [email protected] (J.D.); [email protected] (J.M.) 2 Centre for Nutrition and Food Sciences, Queensland Alliance for Agriculture and Food Innovation, The University of Queensland, St. Lucia, QLD 4072, Australia; [email protected] (M.M.); [email protected] (S.N.); [email protected] (E.R.) * Correspondence: [email protected] Simple Summary: The gut is able to “sense” nutrients and release gut hormones to regulate diges- tive processes. Accordingly, various gastrointestinal cell types possess transient receptor potential channels, cation channels involved in somatosensation, thermoregulation and the sensing of pungent and spicy substances. Recent research shows that both channels are expressed in enteroendocrine Citation: Van Liefferinge, E.; Müller, M.; Van Noten, N.; Degroote, J.; cell types responsible for the release of gut peptide hormones such as Cholecystokinin (CCK) and Niknafs, S.; Roura, E.; Michiels, J. Glucagon-like Peptide-1 (GLP-1). A large array of herbal compounds, used in pig nutrition mostly for Cinnamaldehyde Induces Release of their antibacterial and antioxidant properties, are able to activate these channels. Cinnamaldehyde, Cholecystokinin and Glucagon-Like occurring in the bark of cinnamon trees, acts as an agonist of Transient Receptor Potential Ankyrin 1 Peptide 1 by Interacting with (TRPA1)-channel. -

Trpa1) Activity by Cdk5
MODULATION OF TRANSIENT RECEPTOR POTENTIAL CATION CHANNEL, SUBFAMILY A, MEMBER 1 (TRPA1) ACTIVITY BY CDK5 A dissertation submitted to Kent State University in partial fulfillment of the requirements for the degree of Doctor of Philosophy by Michael A. Sulak December 2011 Dissertation written by Michael A. Sulak B.S., Cleveland State University, 2002 Ph.D., Kent State University, 2011 Approved by _________________, Chair, Doctoral Dissertation Committee Dr. Derek S. Damron _________________, Member, Doctoral Dissertation Committee Dr. Robert V. Dorman _________________, Member, Doctoral Dissertation Committee Dr. Ernest J. Freeman _________________, Member, Doctoral Dissertation Committee Dr. Ian N. Bratz _________________, Graduate Faculty Representative Dr. Bansidhar Datta Accepted by _________________, Director, School of Biomedical Sciences Dr. Robert V. Dorman _________________, Dean, College of Arts and Sciences Dr. John R. D. Stalvey ii TABLE OF CONTENTS LIST OF FIGURES ............................................................................................... iv LIST OF TABLES ............................................................................................... vi DEDICATION ...................................................................................................... vii ACKNOWLEDGEMENTS .................................................................................. viii CHAPTER 1: Introduction .................................................................................. 1 Hypothesis and Project Rationale -

Chemical Tools for the Synthesis and Analysis of Glycans Thamrongsak Cheewawisuttichai [email protected]
The University of Maine DigitalCommons@UMaine Electronic Theses and Dissertations Fogler Library 8-2019 Chemical Tools for the Synthesis and Analysis of Glycans Thamrongsak Cheewawisuttichai [email protected] Follow this and additional works at: https://digitalcommons.library.umaine.edu/etd Recommended Citation Cheewawisuttichai, Thamrongsak, "Chemical Tools for the Synthesis and Analysis of Glycans" (2019). Electronic Theses and Dissertations. 3058. https://digitalcommons.library.umaine.edu/etd/3058 This Open-Access Thesis is brought to you for free and open access by DigitalCommons@UMaine. It has been accepted for inclusion in Electronic Theses and Dissertations by an authorized administrator of DigitalCommons@UMaine. For more information, please contact [email protected]. CHEMICAL TOOLS FOR THE SYNTHESIS AND ANALYSIS OF GLYCANS By Thamrongsak Cheewawisuttichai B.S. Chulalongkorn University, 2012 A DISSERTATION Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy (in Chemistry) The Graduate School The University of Maine August 2019 Advisory Committee: Matthew Brichacek, Assistant Professor of Chemistry, Advisor Alice E. Bruce, Professor of Chemistry Barbara J.W. Cole, Professor of Chemistry Raymond C. Fort, Jr., Professor of Chemistry William M. Gramlich, Associate Professor of Chemistry Copyright 2019 Thamrongsak Cheewawisuttichai ii CHEMICAL TOOLS FOR THE SYNTHESIS AND ANALYSIS OF GLYCANS By Thamrongsak Cheewawisuttichai Dissertation Advisor: Dr. Matthew Brichacek An Abstract of the Dissertation Presented in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy (in Chemistry) August 2019 Glycans can be found in every living organism from plants to bacteria and viruses to human. It has been known that glycans are involved in many biological processes such as structural roles, specific recognition with glycan-binding proteins, and host-pathogen recognitions. -

United States Patent Office Patented Dec
3,293,045 United States Patent Office Patented Dec. 20, 1966 2 vide wintergreen-flavored candies which contain as their 3,293,045 main flavoring ingredient wintergreen oil in lower mini INCREASING THE FLAVOR STRENGTH OF ANE THOLE, CENNAMALDEHYDE AND METHY mum effective levels than have previously been employed. SALICYLATE WITH MALTOL These and other objects are readily achieved through Joan M. Griffin, Forest Hills, N.Y., assignor to Chas. use of the compositions of the instant invention which are, Pfizer & Co., Inc., New York, N.Y., a corporation of in essence: A flavoring composition comprising an agent Delaware Selected from the group consisting of anethole, cinna No Drawing. Filed Oct. 18, 1963, Ser. No. 317,126 maldehyde and methyl salicylate and from about 15% 3 Claims. (C. 99-134) to about 100% by weight thereof of maltol. The instant invention contemplates the use of both This application relates to new and novel flavoring O natural and Synthetic anise, cinnamon and wintergreen compositions. More particularly, it concerns composi oils. It contemplates their use in the form of pure oils tions comprising aromatic flavoring ingredients together or blends of pure oils prepared either synthetically, being with maltol, a gamma-pyrone. There are also contem obtained by chemical reaction and distillation or, natural plated foods, beverages, candy and tablets, syrups, medi 5 ly, being obtained by extraction from the plant material cinal oils, pill and tablet coatings and troches containing from which the Subject oils have been classically isolated. these flavoring compositions. Generally speaking, the natural oils will, as described Among the most useful items of commerce are natural hereinafter, comprise predominantly one chemical entity and Synthetic flavors of the type represented by anise, together with isomers of this entity and minor amounts cinnamon and wintergreen. -

Method TO-11A
EPA/625/R-96/010b Compendium of Methods for the Determination of Toxic Organic Compounds in Ambient Air Second Edition Compendium Method TO-11A Determination of Formaldehyde in Ambient Air Using Adsorbent Cartridge Followed by High Performance Liquid Chromatography (HPLC) [Active Sampling Methodology] Center for Environmental Research Information Office of Research and Development U.S. Environmental Protection Agency Cincinnati, OH 45268 January 1999 Method TO-11A Acknowledgements This Method was prepared for publication in the Compendium of Methods for the Determination of Toxic Organic Compounds in Ambient Air, Second Edition (EPA/625/R-96/010b), which was prepared under Contract No. 68-C3-0315, WA No. 3-10, by Midwest Research Institute (MRI), as a subcontractor to Eastern Research Group, Inc. (ERG), and under the sponsorship of the U.S. Environmental Protection Agency (EPA). Justice A. Manning, John O. Burckle, and Scott Hedges, Center for Environmental Research Information (CERI), and Frank F. McElroy, National Exposure Research Laboratory (NERL), all in the EPA Office of Research and Development, were responsible for overseeing the preparation of this method. Additional support was provided by other members of the Compendia Workgroup, which include: • John O. Burckle, U.S. EPA, ORD, Cincinnati, OH • James L. Cheney, Corps of Engineers, Omaha, NB • Michael Davis, U.S. EPA, Region 7, KC, KS • Joseph B. Elkins Jr., U.S. EPA, OAQPS, RTP, NC • Robert G. Lewis, U.S. EPA, NERL, RTP, NC • Justice A. Manning, U.S. EPA, ORD, Cincinnati, OH • William A. McClenny, U.S. EPA, NERL, RTP, NC • Frank F. McElroy, U.S. EPA, NERL, RTP, NC • Heidi Schultz, ERG, Lexington, MA • William T. -

Multiple Dietary Supplements Do Not Affect Metabolic and Cardio-Vascular Health Andreea Soare Washington University School of Medicine in St
Washington University School of Medicine Digital Commons@Becker Open Access Publications 2014 Multiple dietary supplements do not affect metabolic and cardio-vascular health Andreea Soare Washington University School of Medicine in St. Louis Edward P. Weiss Washington University School of Medicine in St. Louis John O. Holloszy Washington University School of Medicine in St. Louis Luigi Fontana Washington University School of Medicine in St. Louis Follow this and additional works at: https://digitalcommons.wustl.edu/open_access_pubs Recommended Citation Soare, Andreea; Weiss, Edward P.; Holloszy, John O.; and Fontana, Luigi, ,"Multiple dietary supplements do not affect metabolic and cardio-vascular health." Aging.6,2. 149-157. (2014). https://digitalcommons.wustl.edu/open_access_pubs/2607 This Open Access Publication is brought to you for free and open access by Digital Commons@Becker. It has been accepted for inclusion in Open Access Publications by an authorized administrator of Digital Commons@Becker. For more information, please contact [email protected]. www.impactaging.com AGING, February 2014, Vol. 6, No 2 Research Paper Multiple dietary supplements do not affect metabolic and cardio‐ vascular health Andreea Soare1,2*, Edward P. Weiss1,3*, John O. Holloszy 1, and Luigi Fontana1,4,5 1 Division of Geriatrics and Nutritional Sciences, Department of Medicine, Washington University School of Medicine, St. Louis, MO 63130, USA 2 Department of Endocrinology and Diabetes, University Campus Bio‐Medico, Rome, Italy 3 Department of Nutrition and Dietetics, St. Louis University, St. Louis, MO 63130, USA 4 Department of Medicine, Salerno University School of Medicine, Salerno, Italy 5 CEINGE Biotecnologie Avanzate, Napoli, Italy * These authors contributed equally to this research Key words: supplements, endothelial function, arterial stiffness, inflammation, oxidative stress Received: 8/12/13; Accepted: 8/31/13; Published: 9/4/13 Correspondence to: Luigi Fontana, MD/PhD; E‐mail: [email protected] Copyright: © Soare et al. -
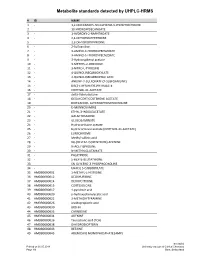
Metabolite Standards Detected by UHPLC-HRMS
Metabolite standards detected by UHPLC-HRMS #ID NAME 1 - 1,2-DIDECANOYL-SN-GLYCERO-3-PHOSPHOCHOLINE 2 - 10-HYDROXYDECANOATE 3 - 1-HYDROXY-2-NAPHTHOATE 4 - 2,4-DIHYDROXYPTERIDINE 5 - 2,6-DIHYDROXYPYRIDINE 6 - 2-Sulfoaniline 7 - 3-AMINO-4-HYDROXYBENZOATE 8 - 3-AMINO-5-HYDROXYBENZOATE 9 - 3-Hydroxyphenyl acetate 10 - 3-METHYL-2-OXINDOLE 11 - 3-NITRO-L-TYROSINE 12 - 4-QUINOLINECARBOXYLATE 13 - 4-QUINOLINECARBOXYLIC ACID 14 - ANILINE-2-SULFONATE (2-SULFOANILINE) 15 - BIS(2-ETHYLHEXYL)PHTHALATE 16 - CORTISOL 21-ACETATE 17 - delta-Valerolactone 18 - DEOXYCORTICOSTERONE ACETATE 19 - DIDECANOYL-GLYCEROPHOSPHOCHOLINE 20 - D-MANNOSAMINE 21 - ETHYL 3-INDOLEACETATE 22 - GALACTOSAMINE 23 - GLUCOSAMINATE 24 - Hydrocortisone acetate 25 - Hydrocortisone acetate (CORTISOL 21-ACETATE) 26- LUMICHROME 27 - Methyl vallinic acid 28 - N6-(DELTA2-ISOPENTENYL)-ADENINE 29 - N-ACETYLPROLINE 30 - N-METHYLGLUTAMATE 31- PALATINOSE 32 - S-HEXYL-GLUTATHIONE 33 - SN-GLYCERO-3-PHOSPHOCHOLINE 34 - URACIL 5-CARBOXYLATE 35 HMDB0000001 1-METHYL-L-HISTIDINE 36 HMDB0000012 DEOXYURIDINE 37 HMDB0000014 DEOXYCYTIDINE 38 HMDB0000015 CORTEXOLONE 39 HMDB0000017 4-pyridoxic acid 40 HMDB0000020 p-hydroxyphenylacetic acid 41 HMDB0000022 3-METHOXYTYRAMINE 42 HMDB0000026 ureidopropionic acid 43 HMDB0000030 BIOTIN 44 HMDB0000033 CARNOSINE 45 HMDB0000034 ADENINE 46 HMDB0000036 Taurocholic acid (TCA) 47 HMDB0000038 DIHYDROBIOPTERIN 48 HMDB0000043 BETAINE 49 HMDB0000045 ADENOSINE MONOPHOSPHATE (AMP) Inselspital Printed on 30.05.2018 University Institute of Clinical Chemistry Page 1/9 Bern, -

Cinnamaldehyde
DRAFT REPORT SUPPORT FOR CHEMICAL NOMINATION AND SELECTION PROCESS OF THE NATIONAL TOXICOLOGY PROGRAM EXECUTIVE SUMMARY OF DATA CINNAMALDEHYDE DECEMBER 14, 1989 Submitted to: NATIONAL TOXICOLOGY PROGRAM Submitted by: Arthur D. Little, Inc. Disclaimer The information contained herein is based on data from current published literature and is believed to be accurate. However, no warranty is expressed or implied regarding the accuracy ofthese data or the results to be obtainedfrom the use thereof TABLE OF CONTENTS ~ I. Introduction .........................................................................................................2 II. Chemical and Physical Properties ...........................................................................3 III. Production!Use........................................................................................................5 A. Production...................................................................................................5 B. Use .........................................................................................................6 IV. Exposure/Regulatory Status ....................................................................................7 A. Consumer Exposure ....................................................................................7 B. Occupational Exposure ...............................................................................7 C. Environmental Exposure .............................................................................8 D. Regulatory Status -

Safety Assessment of Food Flavor - Cinnamaldehyde Sivakumar J T Gowder* Qassim University, College of Applied Medical Sciences, Buraidah, Kingdom of Saudi Arabia
safe Bio ty Gowder, Biosafety 2014, 3:1 Biosafety DOI: 10.4172/2167-0331.1000e147 ISSN: 2167-0331 Editorial Open Access Safety Assessment of Food Flavor - Cinnamaldehyde Sivakumar J T Gowder* Qassim University, College of Applied Medical Sciences, Buraidah, Kingdom of Saudi Arabia A flavor is a substance which may be a single chemical entity It has been estimated that 95% of its consumption is as a flavoring or a blend of chemicals of natural or synthetic origin whose primary material and that its usage will grow by about 3% per year over the purpose is to provide all or part of the particular flavor or effect to any next 5 years [16,17]. Thus, cinnamaldehyde has a high potential for food or other product taken orally. Food flavorings are an essential human consumption in the world. FEMA (The Flavor and Extract element in foods. Flavoring substances can be divided into artificial Manufacturers’ Association of the USA) has given GRAS (Generally flavoring substances and nature-identical flavoring substances. Recognized as Safe) status for cinnamaldehyde. Cinnamaldehyde Artificial flavoring substances are those substances which have not is also approved for use by the Food and Drug Administration of yet been noticed in natural products whereas nature identical flavoring the United States. The Joint FAO/WHO Expert Committee on Food substances are present in natural products intended for human Additives at first set an Acceptable Daily Intake (ADI) of 1.25 mg/ consumption. Toxicological studies on flavoring compounds should be kg body weight. The World Health Organization has established a made according to necessity and adequacy. -

Duke Yale University University
Sven-Eric Jordt, PhD1 Duke Yale Associate Professor University University Sairam Jabba, PhD1 Senior Research Associate Hanno C. Erythropel, PhD2 Associate Research Scientist 1Duke University School of Medicine Department of Anesthesiology Durham NC 27710 2Center for Green Chemistry & Green Engineering at Yale University New Haven, CT 06511 To: Dockets Management Staff (HFA-305) Food and Drug Administration 5630 Fishers Lane, Rm. 1061 Rockville, MD 20852. RE: Docket No. FDA-2012-N-0143 - Harmful and Potentially Harmful Constituents in Tobacco Products - Formation of Flavorant–Solvent Adducts With Novel Toxicological Properties October 4th, 2019 Dear Commissioner Sharpless: With this letter we would like to provide new scientific data in support of the proposed rulemaking by the Food and Drug Administration for Harmful and Potentially Harmful Constituents (HPHC) in Tobacco Products, where FDA has proposed to add 19 new chemical toxicants that are present in tobacco products. We appreciate and agree with FDA that these 19 chemicals should be regarded as HPHC’s. In our opinion, this proposed HPHC list does not include several hundreds of other chemicals and classes of chemicals (especially respiratory irritants) that are present in the tobacco products or delivered through use of these products. In this document, we specifically wanted to inform FDA about flavor-solvent adducts, a class of chemical compounds not declared previously in tobacco products and that have unexpected toxicological effects. These adducts that are generally called as flavor aldehyde- PG/VG acetals are rapidly formed in e-cigarette liquids after mixing of their constituents and under storage conditions between popular flavor-aldehydes like vanillin (vanilla), cinnamaldehyde (cinnamon), benzaldehyde (cherry), citral (citrus), anisaldehyde (anise/spice) and solvents propylene glycol and vegetable glycerine. -

Selective Oxidation of Cinnamyl Alcohol to Cinnamaldehyde Over Functionalized Multi-Walled Carbon Nanotubes Supported Silver-Cobalt Nanoparticles
catalysts Article Selective Oxidation of Cinnamyl Alcohol to Cinnamaldehyde over Functionalized Multi-Walled Carbon Nanotubes Supported Silver-Cobalt Nanoparticles Zahoor Iqbal 1,* , Muhammad Sufaid Khan 1,*, Rozina Khattak 2, Tausif Iqbal 3, Ivar Zekker 4, Muhammad Zahoor 5 , Helal F. Hetta 6 , Gaber El-Saber Batiha 7 and Eida M. Alshammari 8 1 Department of Chemistry, University of Malakand, Chakdara 18800, Pakistan 2 Department of Chemistry, Shaheed Benazir Bhutto Women University, Peshawar 25000, Pakistan; [email protected] 3 Center for Computational Materials Science, University of Malakand, Chakdara 18800, Pakistan; [email protected] 4 Institute of Chemistry, University of Tartu, 14a Ravila St., 50411 Tartu, Estonia; [email protected] 5 Department of Biochemistry, University of Malakand, Chakdara 18800, Pakistan; [email protected] 6 Department of Internal Medicine, University of Cincinnati College of Medicine, Cincinnati, OH 45267-0595, USA; [email protected] 7 Department of Pharmacology and Therapeutics, Faculty of Veterinary Medicine, Damanhour University, Damanhour 22511, El-Beheira, Egypt; [email protected] 8 Department of Chemistry, College of Sciences, University of Ha’il, Ha’il 81451, Saudi Arabia; Citation: Iqbal, Z.; Khan, M.S.; [email protected] Khattak, R.; Iqbal, T.; Zekker, I.; * Correspondence: [email protected] (Z.I.); [email protected] (M.S.K.) Zahoor, M.; Hetta, H.F.; El-Saber Batiha, G.; Alshammari, E.M. Abstract: The selective oxidation of alcohols to aldehydes has attracted a lot of attention because of Selective Oxidation of Cinnamyl its potential use in agrochemicals, fragrances, and fine chemicals. However, due to homogenous Alcohol to Cinnamaldehyde over catalysis, low yield, low selectivity, and hazardous oxidants, traditional approaches have lost their Functionalized Multi-Walled Carbon efficiency.