Dental Abnormalities After Pediatric Bone Marrow Transplantation
Total Page:16
File Type:pdf, Size:1020Kb

Load more
Recommended publications
-

Glossary for Narrative Writing
Periodontal Assessment and Treatment Planning Gingival description Color: o pink o erythematous o cyanotic o racial pigmentation o metallic pigmentation o uniformity Contour: o recession o clefts o enlarged papillae o cratered papillae o blunted papillae o highly rolled o bulbous o knife-edged o scalloped o stippled Consistency: o firm o edematous o hyperplastic o fibrotic Band of gingiva: o amount o quality o location o treatability Bleeding tendency: o sulcus base, lining o gingival margins Suppuration Sinus tract formation Pocket depths Pseudopockets Frena Pain Other pathology Dental Description Defective restorations: o overhangs o open contacts o poor contours Fractured cusps 1 ww.links2success.biz [email protected] 914-303-6464 Caries Deposits: o Type . plaque . calculus . stain . matera alba o Location . supragingival . subgingival o Severity . mild . moderate . severe Wear facets Percussion sensitivity Tooth vitality Attrition, erosion, abrasion Occlusal plane level Occlusion findings Furcations Mobility Fremitus Radiographic findings Film dates Crown:root ratio Amount of bone loss o horizontal; vertical o localized; generalized Root length and shape Overhangs Bulbous crowns Fenestrations Dehiscences Tooth resorption Retained root tips Impacted teeth Root proximities Tilted teeth Radiolucencies/opacities Etiologic factors Local: o plaque o calculus o overhangs 2 ww.links2success.biz [email protected] 914-303-6464 o orthodontic apparatus o open margins o open contacts o improper -

Non-Syndromic Occurrence of True Generalized Microdontia with Mandibular Mesiodens - a Rare Case Seema D Bargale* and Shital DP Kiran
Bargale and Kiran Head & Face Medicine 2011, 7:19 http://www.head-face-med.com/content/7/1/19 HEAD & FACE MEDICINE CASEREPORT Open Access Non-syndromic occurrence of true generalized microdontia with mandibular mesiodens - a rare case Seema D Bargale* and Shital DP Kiran Abstract Abnormalities in size of teeth and number of teeth are occasionally recorded in clinical cases. True generalized microdontia is rare case in which all the teeth are smaller than normal. Mesiodens is commonly located in maxilary central incisor region and uncommon in the mandible. In the present case a 12 year-old boy was healthy; normal in appearance and the medical history was noncontributory. The patient was examined and found to have permanent teeth that were smaller than those of the average adult teeth. The true generalized microdontia was accompanied by mandibular mesiodens. This is a unique case report of non-syndromic association of mandibular hyperdontia with true generalized microdontia. Keywords: Generalised microdontia, Hyperdontia, Permanent dentition, Mandibular supernumerary tooth Introduction [Ullrich-Turner syndrome], Chromosome 13[trisomy 13], Microdontia is a rare phenomenon. The term microdontia Rothmund-Thomson syndrome, Hallermann-Streiff, Oro- (microdentism, microdontism) is defined as the condition faciodigital syndrome (type 3), Oculo-mandibulo-facial of having abnormally small teeth [1]. According to Boyle, syndrome, Tricho-Rhino-Phalangeal, type1 Branchio- “in general microdontia, the teeth are small, the crowns oculo-facial syndrome. short, and normal contact areas between the teeth are fre- Supernumerary teeth are defined as any supplementary quently missing” [2] Shafer, Hine, and Levy [3] divided tooth or tooth substance in addition to usual configuration microdontia into three types: (1) Microdontia involving of twenty deciduous and thirty two permanent teeth [7]. -

Free PDF Download
Eur opean Rev iew for Med ical and Pharmacol ogical Sci ences 2014; 18: 440-444 Radiographic evaluation of the prevalence of enamel pearls in a sample adult dental population H. ÇOLAK, M.M. HAMIDI, R. UZGUR 1, E. ERCAN, M. TURKAL 1 Department of Restorative Dentistry, Kirikkale University School of Dentistry, Kirikkale, Turkey 1Department of Prosthodontics, Kirikkale University School of Dentistry, Kirikkale, Turkey Abstract. – AIM: Enamel pearls are a tooth One theory of the enamel pearl etiology is that anomaly that can act as contributing factors in the enamel pearls develop as a result of a localized development of periodontal disease. Studies that developmental activity of a remnant of Hertwig’s have addressed the prevalence of enamel pearls in epithelial root sheath which has remained adher - populations were scarce. The purpose of this study 5 was to evaluate the prevalence of enamel pearls in ent to the root surface during root development . the permanent dentition of Turkish dental patients It is believed that cells differentiate into function - by means of panoramic radiographs. ing ameloblasts and produce enamel deposits on PATIENTS AND METHODS: Panoramic radi - the root. The conditions needed for local differ - ographs of 6912 patients were examined for the entiation and functioning of ameloblasts in this presence of enamel pearls. All data (age, sex and ectopic position are not fully understood 6,7 . systemic disease or syndrome) were obtained from the patient files and analyzed for enamel The most common site for enamel pearls is at pearls. Descriptive characteristics of sexes, the cementoenamel junction of multirooted jaws, and dental localization were recorded. -
Developmental Disturbances Affecting Teeth
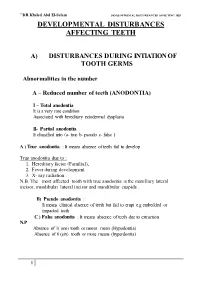
``DR.Khaled Abd El-Salam DEVELO PMENTAL DISTURBANCES AFFECTING TEET DEVELOPMENTAL DISTURBANCES AFFECTING TEETH A) DISTURBANCES DURING INTIATION OF TOOTH GERMS Abnormalities in the number A – Reduced number of teeth (ANODONTIA) I – Total anodontia It is a very rare condition Associated with hereditary ectodermal dysplasia II- Partial anodontia It classified into (a- true b- pseudo c- false ) A ) True anodontia : It means absence of teeth fail to develop True anodontia due to : 1. Hereditary factor (Familial), 2. Fever during development. 3. X- ray radiation . N.B. The most affected tooth with true anodontia is the maxillary lateral incisor, mandibular lateral incisor and mandibular cuspids . B) Pseudo anodontia : It means clinical absence of teeth but fail to erupt e.g embedded or impacted teeth C ) False anodontia : It means absence of teeth due to extraction N.P Absence of 1( one) tooth or mores mean (Hypodontia) Absence of 6 (six) tooth or more means (hyperdontia) 1 ``DR.Khaled Abd El-Salam DEVELO PMENTAL DISTURBANCES AFFECTING TEET ECTODERMAL DYSPLASIA • It is a hereditary disease which involves all structures which are derived from the ectoderm . • It is characterized by (general manifestation) : 1- Skin ( thin, smooth, Dry skin) 2- Hair (Absence or reduction (hypotrichosis). 3- Sweat-gland (Absence anhydrosis). 4- sebaceous gland ( absent lead to dry skin) 5-Temperature elevation (because of anhydrosis) 6- Depressed bridge of the nose 7- Defective mental development 8- Defective of finger nail Oral manifestation include teeth and -

On the Genetics of Hypodontia and Microdontia: Synergism Or Allelism of Major Genes in a Family with Six Affected Members
JMed Genet 1996;33:137-142 137 On the genetics of hypodontia and microdontia: synergism or allelism of major genes in a family J Med Genet: first published as 10.1136/jmg.33.2.137 on 1 February 1996. Downloaded from with six affected members S P Lyngstadaas, H Nordbo, T Gedde-Dahl Jr, P S Thrane Abstract and epigenetic factors.7 In a large study oftooth Familial severe hypodontia of the per- number and size in British schoolchildren, ex- manent dentition is a rare condition. The cluding patients with more widespread ab- genetics ofthis entity remains unclear and normalities, Brook3 favoured a multifactorial several modes of inheritance have been model with a continuous spectrum, related to suggested. We report here an increase in tooth number and size, with thresholds, and the number of congenitally missing teeth where position on the scale depends upon the after the mating of affected subjects from combination of numerous genetic and en- two unrelated Norwegian families. This vironmental factors, each with a small effect. condition may be the result of allelic mut- In this study the proportion ofaffected relatives ations at a single gene locus. Alternatively, varied with the severity of the condition in the incompletely penetrant non-allelic genes probands and an association between hy- may show a synergistic effect as expected podontia and microdontia was noted. for a multifactorial trait with interacting Other causes of hypodontia have been sug- gene products. This and similar kindreds gested and include an evolutionary trend to- may allow identification of genes involved wards fewer teeth,28 infections during in growth and differentiation of dental tis- pregnancy and early childhood, hormonal dys- sues by linkage and haplotype association function, which itself may be inherited, and analysis. -

A Global Compendium of Oral Health
A Global Compendium of Oral Health A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan A Global Compendium of Oral Health: Tooth Eruption and Hard Dental Tissue Anomalies Edited by Morenike Oluwatoyin Folayan This book first published 2019 Cambridge Scholars Publishing Lady Stephenson Library, Newcastle upon Tyne, NE6 2PA, UK British Library Cataloguing in Publication Data A catalogue record for this book is available from the British Library Copyright © 2019 by Morenike Oluwatoyin Folayan and contributors All rights for this book reserved. No part of this book may be reproduced, stored in a retrieval system, or transmitted, in any form or by any means, electronic, mechanical, photocopying, recording or otherwise, without the prior permission of the copyright owner. ISBN (10): 1-5275-3691-2 ISBN (13): 978-1-5275-3691-3 TABLE OF CONTENTS Foreword .................................................................................................. viii Introduction ................................................................................................. 1 Dental Development: Anthropological Perspectives ................................. 31 Temitope A. Esan and Lynne A. Schepartz Belarus ....................................................................................................... 48 Natallia Shakavets, Alexander Yatzuk, Klavdia Gorbacheva and Nadezhda Chernyavskaya Bangladesh ............................................................................................... -

Oral Manifestations in Patients with Glycogen Storage Disease: a Systematic Review of the Literature
applied sciences Review Oral Manifestations in Patients with Glycogen Storage Disease: A Systematic Review of the Literature 1, 1, 1 2 Antonio Romano y, Diana Russo y , Maria Contaldo , Dorina Lauritano , Fedora della Vella 3 , Rosario Serpico 1, Alberta Lucchese 1,* and Dario Di Stasio 1 1 Multidisciplinary Department of Medical-Surgical and Dental Specialties, University of Campania “L. Vanvitelli”, Via Luigi De Crecchio 6, 80138 Naples, Italy; [email protected] (A.R.); [email protected] (D.R.); [email protected] (M.C.); [email protected] (R.S.); [email protected] (D.D.S.) 2 Department of Medicine and Surgery, Centre of Neuroscience of Milan, University of Milano-Bicocca, 20126 Milan, Italy; [email protected] 3 Interdisciplinary Department of Medicine, University of Bari “A. Moro”, 70124 Bari, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-0815667670 Contributed equally to this article, so they are co-first authors. y Received: 28 August 2020; Accepted: 21 September 2020; Published: 25 September 2020 Abstract: (1) Background: Glycogen storage disease (GSD) represents a group of twenty-three types of metabolic disorders which damage the capacity of body to store glucose classified basing on the enzyme deficiency involved. Affected patients could present some oro-facial alterations: the purpose of this review is to catalog and characterize oral manifestations in these patients. (2) Methods: a systematic review of the literature among different search engines using PICOS criteria has been performed. The studies were included with the following criteria: tissues and anatomical structures of the oral cavity in humans, published in English, and available full text. -

Esthetic Treatment of Anterior Spacings in a Patient with Localized
pISSN, eISSN 0125-5614 Case Report M Dent J 2019; 39 (2) : 53-63 Esthetic treatment of anterior spacings in a patient with localized microdontia using no-prep veneers combined with periodontal surgery: A clinical report Pajaree Limothai, Chalermpol Leevailoj Esthetic Restorative and Implant Dentistry, Faculty of Dentistry, Chulalongkorn University Objectives: This case report describes the treatment of a patient with maxillary anterior spacings, resulting from microdontia, using a multidisciplinary approach to improve her esthetic appearance. Materials and Methods: A 23-year-old Thai female patient had multiple spaces between her maxillary anterior teeth with a high smile line and an unsymmetrical gingival level. The Recurring Esthetic Dental (RED) proportion was used to determine the widths of maxillary teeth and Bolton’s analysis was used to confirm the RED results, after that a diagnostic wax-up model was fabricated. Esthetic crown lengthening was performed from the right maxillary canine to the left maxillary canine to reduce excess gingival exposure and increase the length of the teeth according to the proportion acquired from the calculation. After complete gingival healing, no-prep ceramic veneers were placed on the maxillary anterior teeth using the IPS Empress® Esthetic ceramic system. Results: The no-prep veneers preserved all tooth structures and gave a satisfactory esthetic result. The patient was satisfied with the outcome. The final restorations closed the spaces with the natural appearance the patient desired. The function and occlusion of the restorations were good. The veneers and the periodontal tissues were in good condition at the 1-year recall. Conclusion: The multidisciplinary approach and no-prep ceramic veneers used in this case restored the maxillary anterior spacing and provided an excellent esthetic outcome. -

Oral Manifestations of Red Blood C Research Article
z Available online at http://www.journalcra.com INTERNATIONAL JOURNAL OF CURRENT RESEARCH International Journal of Current Research Vol. 10, Issue, 11, pp.75681-75686, November, 2018 DOI: https://doi.org/10.24941/ijcr.33312.11.2018 ISSN: 0975-833X RESEARCH ARTICLE ORAL MANIFESTATIONS OF RED BLOOD CELL DISORDERS: A RECENT ANATOMIZATION 1Swatantra Shrivastava, 2Sourabh Sahu, 3Pavan Kumar Singh, 4Rajeev Kumar Shrivastava, 5, *Soumendu Bikash Maiti and 6Stuti Shukla 1Department of Oral Medicine and Radiology, New Horizon Dental College and Research Institute, Bilaspur, India 2MGM Medical College and Hospital, Aurangabad, India 3Department of Public Health Dentistry, Vyas Dental College and Hospital, India 4Master of Dental Surgery , Department of Prosthodontics and Crown and Bridge, New Horizon Dental College and Research Institute, Bilaspur, Udaipur, India 5Senior Lecturer, Department of Oral Medicine and Radiology, Pacific Dental College and Research Center, India 6Post Graduate, Department of Oral Medicine and Radiology, New horizon Dental College and Research center, Bilaspur India ARTICLE INFO ABSTRACT Article History: Primary objective of the literature is recognize and evaluate the wide array of oral manifestations Received 17th August, 2018 associated with red blood cell disorders which would eventually aid in diagnosis of the lesions Received in revised form associated with the disorders for the practitioners. It starts with petechiae, spontaneous gingival 03rd September, 2018 bleeding, herpetic infection in aplastic anaemia to hunter’s glossitis in pernicious anaemia. Literature Accepted 26th October, 2018 also includes enamel hypoplasia associated with erythroblastis fetalis, atrophic glossitis in iron th Published online 30 November, 2018 deficiency anemia with symptom of glossodynia in megaloblastic anemia. Marked manifestations of pharyngo-esophageal ulcerations and esophageal webs seen in plummer Vinson syndrome and Key Words: periodontitis, taurodontism, agenesia, supernumerary teeth to be seen in fanconi’s anemia. -

Prevalence and Treatment Approaches of Impacted
RESEARCH PREVALENCE AND TREATMENT APPROACHES OF IMPACTED TEETH IN OLDER ADULTS Turkish Journal of Geriatrics DOI: ....10.31086/tjgeri.2020.191 2020; 23(3):23(4): ...-...524-533 ABSTRACT 1 Hasan Onur ŞİMŞEK Introduction: The primary aim of our study was to identify the problems 2 caused by impacted teeth and to discuss treatment alternatives in older adults. The Gökhan ÖZKAN 1 secondary aim of the study was to investigate the presence, frequency, and position Umut DEMETOĞLU of impacted teeth in older adults and to investigate the reasons for impaction. Materials and Methods: The study included 79,733 patients who were admitted to the Aydın Adnan Menderes University, Faculty of Dentistry since December 2013. From these patients, 8,670 panoramic radiographs of patients aged 60 years and older were evaluated retrospectively. Results: The most common impacted teeth were the third molar (453, 77.3%), canine (109, 18.6%), and premolar (13, 2.2%). There was a statistically significant difference between the presence of an impacted tooth and the outcome of treatment (p<0.001). Of the (216, 51.8%) patients for whom surgical tooth extraction was prescribed, (159, 38.1%) underwent extraction, while (57, 13.7%) patients refused treatment. CORRESPONDANCE Conclusions: Routine follow-up should be recommended for asymptomatic 1 Hasan Onur Şimşek teeth that do not cause significant problems in the adjacent teeth and surrounding tissues instead of prophylactic extraction in all age groups, especially in older adults. Aydın Adnan Menderes University, -

Associated Dental Anomalies: the Orthodontist Decoding the Genetics Which Regulates the Dental Development Disturbances
T ÓPICO E SP E CIAL Anomalias dentárias associadas: o ortodontista decodificando a genética que rege os distúrbios de desenvolvimento dentário Daniela Gamba Garib*, Bárbara Maria Alencar**, Flávio Vellini Ferreira***, Terumi Okada Ozawa**** Resumo O presente trabalho versa sobre o diagnóstico e a abordagem ortodôntica das anomalias dentárias, enfatizando os aspectos etiológicos que definem tais irregularidades de desenvolvimento. Parece existir uma inter-relação genética na determinação de algumas dessas anomalias, considerando-se a alta frequência de associações. Um mesmo defeito genético pode originar diferentes manifestações fenotípicas, incluindo agenesias, microdontias, ectopias e atraso no desenvolvimento dentário. As implicações clínicas das anomalias dentárias associadas são muito relevantes, uma vez que o diag- nóstico precoce de uma determinada anomalia dentária pode alertar o clínico sobre a possibilidade de desenvolvimento de outras anomalias associadas no mesmo paciente ou em outros membros da família, permitindo a intervenção ortodôntica em época oportuna. Palavras-chave: Genética. Anomalias dentárias. Agenesia. Etiologia. Ortodontia. INTRODUÇÃO anomalias dentárias. As anomalias expressam-se Caracterizada por complexos e precisos pro- com distintos graus de severidade. Da manifesta- cessos biológicos de substituição de dentes decí- ção mais branda para a mais severa – representa- duos por dentes permanentes, a dentadura mista das, respectivamente, desde o atraso cronológico representa uma das manifestações de perfeição na -

Journal of Science / Vol 8 / Issue 1 / 2018 / 19-25
Monika Rohilla. / Journal of Science / Vol 8 / Issue 1 / 2018 / 19-25. e ISSN 2277 - 3290 Print ISSN 2277 - 3282 Journal of Science Microbiology www.journalofscience.net Research article DISTURBANCES DURING APPOSITION OF DENTAL HARD TISSUES Monika Rohilla* PG Demonstrator in the Department of Pedodontics, PGIDS, Rohtak, Haryana 124514, India. ABSTRACT A series of factors influence the normal development of the occlusion, interfering in correct alignment of the teeth and harmonic relationship with the adjacent and antagonistic elements. Developmental disturbances of the teeth may manifest by variations in number, position, size, shape, eruption, structure. Such disturbances may occur in association with some more generalised disorder or may occur independently. The present study is undertaken to review the etiopathogenesis of various developmental disturbances during apposition of dental hard tissues. Keywords: Development, Hypoplasia, Apposition. Access this article online mutations in the AMEL-X gene which codes for Home page: Quick Response ameloblastin, enamelin, or tuftelin. In the case of http://journalofscience.net// code autosomal dominant type, the locus of defective gene is on chromosome 4q21 to which enamelin maps. The most DOI: common X-linked types are caused by a variety of defects http://dx.doi.org/10.21276/jos.2018.8.1.5 in the amelogenin genes and confusingly, it seems the same mutation can sometimes cause hypoplastic, Received:16.11.17 Revised:28.11.17 Accepted:06.12.17 hypomineralisation, or hypomaturation forms in different patients [2]. If there is disturbance of the first phase in which the Corresponding Author matrix is being formed the result is enamel hypoplasia Monika Rohilla and if it occurs during the second phase then the quality is PG demonstrator in the department of pedodontics, PGIDS, Rohtak, affected resulting in enamel hypomineralisation.