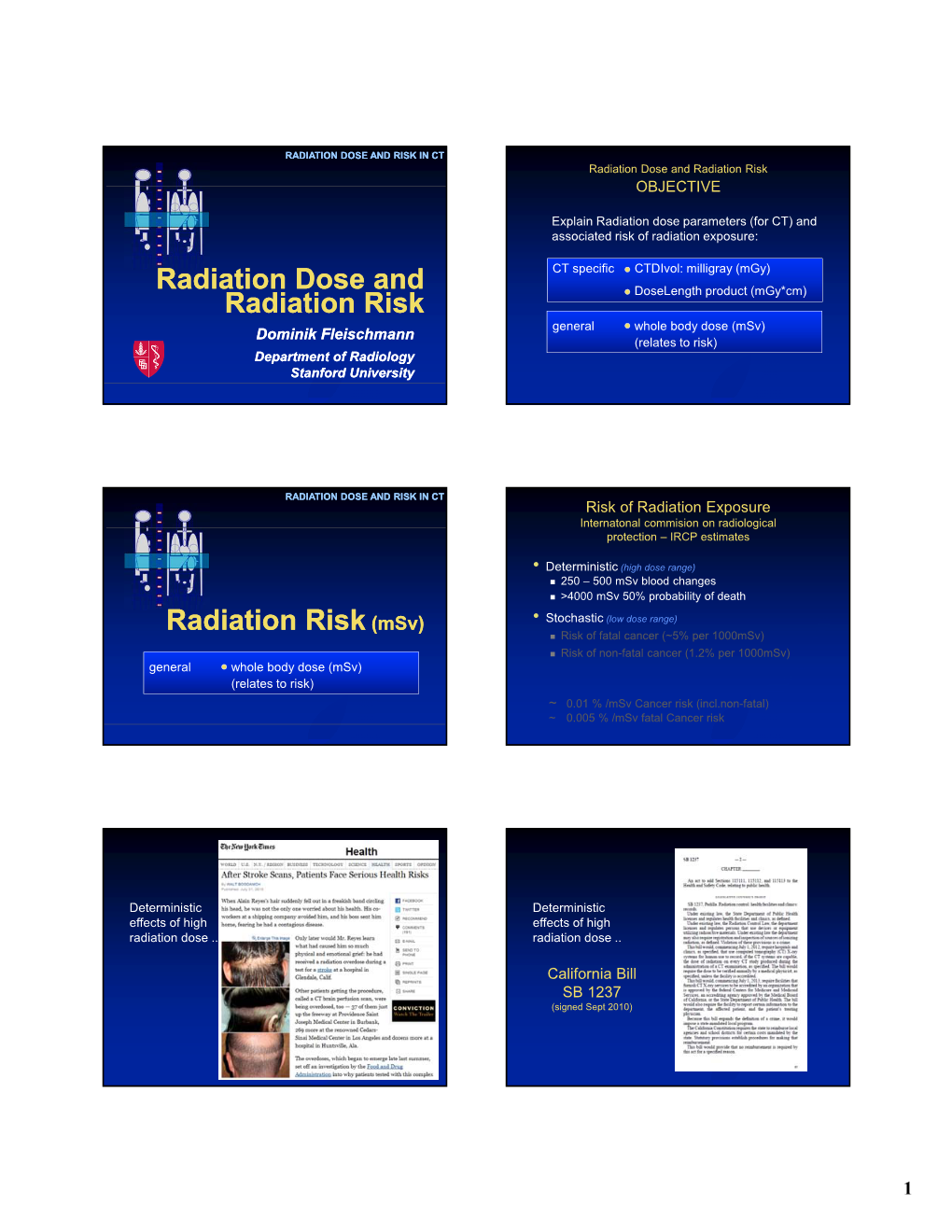
(Msv) Radiation Risk
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![小型飛翔体/海外 [Format 2] Technical Catalog Category](https://docslib.b-cdn.net/cover/2534/format-2-technical-catalog-category-112534.webp)
小型飛翔体/海外 [Format 2] Technical Catalog Category
小型飛翔体/海外 [Format 2] Technical Catalog Category Airborne contamination sensor Title Depth Evaluation of Entrained Products (DEEP) Proposed by Create Technologies Ltd & Costain Group PLC 1.DEEP is a sensor analysis software for analysing contamination. DEEP can distinguish between surface contamination and internal / absorbed contamination. The software measures contamination depth by analysing distortions in the gamma spectrum. The method can be applied to data gathered using any spectrometer. Because DEEP provides a means of discriminating surface contamination from other radiation sources, DEEP can be used to provide an estimate of surface contamination without physical sampling. DEEP is a real-time method which enables the user to generate a large number of rapid contamination assessments- this data is complementary to physical samples, providing a sound basis for extrapolation from point samples. It also helps identify anomalies enabling targeted sampling startegies. DEEP is compatible with small airborne spectrometer/ processor combinations, such as that proposed by the ARM-U project – please refer to the ARM-U proposal for more details of the air vehicle. Figure 1: DEEP system core components are small, light, low power and can be integrated via USB, serial or Ethernet interfaces. 小型飛翔体/海外 Figure 2: DEEP prototype software 2.Past experience (plants in Japan, overseas plant, applications in other industries, etc) Create technologies is a specialist R&D firm with a focus on imaging and sensing in the nuclear industry. Createc has developed and delivered several novel nuclear technologies, including the N-Visage gamma camera system. Costainis a leading UK construction and civil engineering firm with almost 150 years of history. -

Absorbed Dose in Radioactive Media Outline Introduction Radiation Equilibrium Charged-Particle Equilibrium Limiting Cases
Outline • General dose calculation considerations, Absorbed Dose in Radioactive absorbed fraction Media • Radioactive disintegration processes and associated dose deposition – Alpha disintegration Chapter 5 – Beta disintegration – Electron-capture transitions F.A. Attix, Introduction to Radiological – Internal conversion Physics and Radiation Dosimetry • Summary Introduction Radiation equilibrium • We are interested in calculating the absorbed dose in a. The atomic composition radioactive media, applicable to cases of of the medium is – Dose within a radioactive organ homogeneous – Dose in one organ due to radioactive source in another b. The density of the organ medium is • If conditions of CPE or RE are satisfied, dose homogeneous c. The radioactive source calculation is straightforward is uniformly distributed • Intermediate situation is more difficult but can be d. No external electric or handled at least in approximations magnetic fields are present Charged-particle equilibrium Limiting cases • Emitted radiation typically includes both • Each charged particle of a given type and photons (longer range) and charged energy leaving the volume is replaced by an particles (shorter range) identical particle of the same energy entering • Assume the conditions for RE are satisfied the volume • Consider two • Existence of RE is sufficient condition for CPE limited cases based • Even if RE does not exist CPE may still exist on the size of the (for a very large or a very small volume) radioactive object 1 Limiting cases: small object Limiting -

G20070354/G20070331 Fact Sheet, Biological Effects of Radiation
Fact Sheet 11 Ofice of Public Affairs Telephone: 301/415-8200 E-mail : opa @nrc.g ov I Biological Effects of Radiation Background Radiation is all around us. It is naturally present in our environment and has been since the birth of this planet. Consequently, life has evolved in an environment which has significant levels of ionizing radiation. It comes from outer space (cosmic), the ground (terrestrial), and even from within our own bodies. It is present in the air we breathe, the food we eat, the water we drink, and in the construction materials used to build our homes. Certain foods such as bananas and brazil nuts naturally contain higher levels of radiation than other foods. Brick and stone homes have higher natural radiation levels than homes made of other building materials such as wood. Our nation's Capitol, which is largely constructed of granite, contains higher levels of natural radiation than most homes. Levels of natural or background radiation can vary greatly from one location to the next. For example, people residing in Colorado are exposed to more natural radiation than residents of the east or west coast because Colorado has more cosmic radiation at a higher altitude and more terrestrial radiation from soils enriched in naturally occurring uranium. Furthermore, a lot of our natural exposure is due to radon, a gas from the earth's crust that is present in the air we breathe. The average annual radiation exposure from natural sources to an individual in the United States is about 300 millirem (3 millisieverts)*. Radon gas accounts for two-thirds of this exposure, while cosmic, terrestrial, and internal radiation account for the remainder. -

How Do Radioactive Materials Move Through the Environment to People?
5. How Do Radioactive Materials Move Through the Environment to People? aturally occurring radioactive materials Radionuclides can be removed from the air in Nare present in our environment and in several ways. Particles settle out of the our bodies. We are, therefore, continuously atmosphere if air currents cannot keep them exposed to radiation from radioactive atoms suspended. Rain or snow can also remove (radionuclides). Radionuclides released to them. the environment as a result of human When these particles are removed from the activities add to that exposure. atmosphere, they may land in water, on soil, or Radiation is energy emitted when a on the surfaces of living and non-living things. radionuclide decays. It can affect living tissue The particles may return to the atmosphere by only when the energy is absorbed in that resuspension, which occurs when wind or tissue. Radionuclides can be hazardous to some other natural or human activity living tissue when they are inside an organism generates clouds of dust containing radionu- where radiation released can be immediately clides. absorbed. They may also be hazardous when they are outside of the organism but close ➤ Water enough for some radiation to be absorbed by Radionuclides can come into contact with the tissue. water in several ways. They may be deposited Radionuclides move through the environ- from the air (as described above). They may ment and into the body through many also be released to the water from the ground different pathways. Understanding these through erosion, seepage, or human activities pathways makes it possible to take actions to such as mining or release of radioactive block or avoid exposure to radiation. -

Industrial Radiography
RADIATION PROTECTION OF WORKERS Industrial Radiography RADIATION AND RADIOGRAPHS RADIOACTIVE SOURCES PROCEDURES RADIOGRAPHERS DO follow the procedures. Ionizing radiation can pen- Materials of higher den Sealed sources are small þ Safe storage Precautions þ DO use the appropriate equipment, including collimators. in size and contain material etrate objects and create sity absorb more radiation. þ DO confi rm that there are no other people working in the images on photographic The metal components are which emits penetrating area of radiography. fi lm. The technique is revealed inside this tele radiation continuously. Radioactive sources should be kept in a secure, fi re þ DO use clear working signs and signals. called radiography and phone because they have Special containers made þ DO set up the controlled area and the necessary barriers. the processed fi lms are absorbed more radiation of dense metal shielding resistant and adequately shielded storage location þ DO confi rm the location of the source, or that X rays are called radiographs. than the surrounding plastic. are necessary to store, not being generated, by use of a survey meter. when not in use, and should move and manipulate these þ DO secure and store the source or X ray machine when sources. Due to their small be kept separate from other not in use. materials. The storage loca- size and manoeuvrability, Portable and mobile radiographic þ DO wear your personal dosimeter. sealed sources can be containers. ~ tion for X ray machines that used in confined spaces. are not in use is not required to be shielded. OTHER WORKERS Iridium-192 is a common radioactive source used þ DO observe the access restrictions, however remote it may in gamma radiography. -

Radiation Basics
Environmental Impact Statement for Remediation of Area IV \'- f Susana Field Laboratory .A . &at is radiation? Ra - -.. - -. - - . known as ionizing radiatios bScause it can produce charged.. particles (ions)..- in matter. .-- . 'I" . .. .. .. .- . - .- . -- . .-- - .. What is radioactivity? Radioactivity is produced by the process of radioactive atmi trying to become stable. Radiation is emitted in the process. In the United State! Radioactive radioactivity is measured in units of curies. Smaller fractions of the curie are the millicurie (111,000 curie), the microcurie (111,000,000 curie), and the picocurie (1/1,000,000 microcurie). Particle What is radioactive material? Radioactive material is any material containing unstable atoms that emit radiation. What are the four basic types of ionizing radiation? Aluminum Leadl Paper foil Concrete Adphaparticles-Alpha particles consist of two protons and two neutrons. They can travel only a few centimeters in air and can be stopped easily by a sheet of paper or by the skin's surface. Betaparticles-Beta articles are smaller and lighter than alpha particles and have the mass of a single electron. A high-energy beta particle can travel a few meters in the air. Beta particles can pass through a sheet of paper, but may be stopped by a thin sheet of aluminum foil or glass. Gamma rays-Gamma rays (and x-rays), unlike alpha or beta particles, are waves of pure energy. Gamma radiation is very penetrating and can travel several hundred feet in air. Gamma radiation requires a thick wall of concrete, lead, or steel to stop it. Neutrons-A neutron is an atomic particle that has about one-quarter the weight of an alpha particle. -

Radionuclides (Including Radon, Radium and Uranium)
Radionuclides (including Radon, Radium and Uranium) Hazard Summary Uranium, radium, and radon are naturally occurring radionuclides found in the environment. No information is available on the acute (short-term) noncancer effects of the radionuclides in humans. Animal studies have reported inflammatory reactions in the nasal passages and kidney damage from acute inhalation exposure to uranium. Chronic (long-term) inhalation exposure to uranium and radon in humans has been linked to respiratory effects, such as chronic lung disease, while radium exposure has resulted in acute leukopenia, anemia, necrosis of the jaw, and other effects. Cancer is the major effect of concern from the radionuclides. Radium, via oral exposure, is known to cause bone, head, and nasal passage tumors in humans, and radon, via inhalation exposure, causes lung cancer in humans. Uranium may cause lung cancer and tumors of the lymphatic and hematopoietic tissues. EPA has not classified uranium, radon or radium for carcinogenicity. Please Note: The main sources of information for this fact sheet are EPA's Integrated Risk Information System (IRIS) (5), which contains information on oral chronic toxicity and the RfD for uranium, and the Agency for Toxic Substances and Disease Registry's (ATSDR's) Toxicological Profiles for Uranium, Radium, and Radon. (1) Uses Uranium is used in nuclear power plants and nuclear weapons. Very small amounts are used in photography for toning, in the leather and wood industries for stains and dyes, and in the silk and wood industries. (2) Radium is used as a radiation source for treating neoplastic diseases, as a radon source, in radiography of metals, and as a neutron source for research. -
Development of Chemical Dosimeters Development Of
SUDANSUDAN ACADEMYAGADEMY OFOF SCIENCES(SAS)SGIENGES(SAS) ATOMICATOMIC ENERGYEhTERGYRESEARCHESRESEARCHES COORDINATIONCOORDII\rATI ON COUNCILCOUNCIL - Development of Chemical Dosimeters A dissertation Submitted in a partial Fulfillment of the Requirement forfbr Diploma Degree in Nuclear Science (Chemistry) By FareedFadl Alla MersaniMergani SupervisorDr K.S.Adam MurchMarch 2006 J - - - CONTENTS Subject Page -I - DedicationDedication........ ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... ... I Acknowledgement ... '" ... ... ... ... ... ... '" ... ... ... ... '" ... '" ....... .. 11II Abstract ... ... ... '" ... ... ... '" ... ... ... ... -..... ... ... ... ... ... ..... III -I Ch-lch-1 DosimetryDosimefry - 1-1t-l IntroductionLntroduction . 1I - 1-2t-2 Principle of Dosimetry '" '" . 2 1-3l-3 DosimetryDosimefiySystems . 3J 1-3-1l-3-l primary standard dosimeters '" . 4 - 1-3-2l-3-Z Reference standard dosimeters ... .. " . 4 1-3-3L-3-3 Transfer standard dosimeters ... ... '" . 4 1-3-4t-3-4 Routine dosimeters . 5 1-4I-4 Measurement of absorbed dose . 6 1-5l-5 Calibration of DosimetryDosimetrvsystemsvstem '" . 6 1-6l-6 Transit dose effects . 8 Ch-2ch-2 Requirements of chemical dosimeters 2-12-l Introduction ... ... ... .............................................. 111l 2-2 Developing of chemical dosimeters ... ... .. ....... ... .. ..... 12t2 2-3 Classification of Dosimetry methods.methods .......................... 14l4 2-4 RequirementsRequiremsnts of ideal chemical dosimeters ,. ... 15 2-5 Types of chemical system . -

6.2.43A Radiation-Dominated Model of the Universe
6 BIG BANG COSMOLOGY – THE EVOLVING UNIVERSE 6.2.43A radiation-dominated model of the Universe R We have just seen that in the early Universe, the dominant energy density is that due to the radiation within the Universe. The Friedmann equation that was described in Chapter 5 (Box 5.4) can be solved for such conditions and the way in which the scale factor varies with time for such a model is shown in Figure 6.7. One important feature of such a model is that the scale factor varies in the following way: R(t) ∝ t1/2 (6.17) 0 t −4 Because the energy density of radiation is dominant for times when R(t)/R(t0) < 10 , all cosmological models which start at t = 0 with R(0) = 0, will go through a phase Figure 6.73The evolution of the that is well described by this radiation-dominated model. Thus we are in the rather scale factor with time in a remarkable position that regardless of which type of cosmological model best cosmological model in which the dominant contribution to the describes the Universe at the present, we can be reasonably confident that we energy density arises from the know how the scale factor varied with time in the first few tens of thousands of radiation within the Universe years of the big bang. (i.e. during the radiation-dominated However, the temperature of the background radiation varies with scale factor era). according to T(t) ∝ 1/R(t) (Equation 6.6). It follows that during the radiation- dominated era the temperature of the background radiation varies with time according to T(t) ∝ t −1/2 (6.18) This describes how temperature changes with time in an expanding universe where the energy density of radiation is the dominant component. -

The International Commission on Radiological Protection: Historical Overview
Topical report The International Commission on Radiological Protection: Historical overview The ICRP is revising its basic recommendations by Dr H. Smith Within a few weeks of Roentgen's discovery of gamma rays; 1.5 roentgen per working week for radia- X-rays, the potential of the technique for diagnosing tion, affecting only superficial tissues; and 0.03 roentgen fractures became apparent, but acute adverse effects per working week for neutrons. (such as hair loss, erythema, and dermatitis) made hospital personnel aware of the need to avoid over- Recommendations in the 1950s exposure. Similar undesirable acute effects were By then, it was accepted that the roentgen was reported shortly after the discovery of radium and its inappropriate as a measure of exposure. In 1953, the medical applications. Notwithstanding these observa- ICRU recommended that limits of exposure should be tions, protection of staff exposed to X-rays and gamma based on consideration of the energy absorbed in tissues rays from radium was poorly co-ordinated. and introduced the rad (radiation absorbed dose) as a The British X-ray and Radium Protection Committee unit of absorbed dose (that is, energy imparted by radia- and the American Roentgen Ray Society proposed tion to a unit mass of tissue). In 1954, the ICRP general radiation protection recommendations in the introduced the rem (roentgen equivalent man) as a unit early 1920s. In 1925, at the First International Congress of absorbed dose weighted for the way different types of of Radiology, the need for quantifying exposure was radiation distribute energy in tissue (called the dose recognized. As a result, in 1928 the roentgen was equivalent in 1966). -

Radiation Safety in Fluoroscopy
Radiation Safety for New Medical Physics Graduate Students John Vetter, PhD Medical Physics Department UW School of Medicine & Public Health Background and Purpose of This Training . This is intended as a brief introduction to radiation safety from the perspective of a Medical Physicist. Have a healthy respect for radiation without an undue fear of it. The learning objectives are: . To point out the sources of ionizing radiation in everyday life and at work. To present an overview of the health effects of ionizing radiation. To show basic concepts and techniques used to protect against exposure to ionizing radiation. Further training in Radiation Safety can be found at: https://ehs.wisc.edu/radiation-safety-training/ Outline . Ionizing Radiation . Definition, Quantities & Units . Levels of Radiation Exposure . Background & Medical . Health Effects of Radiation Exposure . Stochastic & Deterministic . Limits on Radiation Exposure . Rationale for Exposure Limits . Minimizing Radiation Exposure . Time, Distance, Shielding, Containment Definition of Ionizing Radiation . Radiation can be thought of as energy in motion. Electromagnetic radiation is pure energy that moves at the speed of light in the form of photons and includes: radio waves; microwaves; infrared, visible and ultraviolet light; x-rays and γ-rays. A key difference between these forms of electromagnetic radiation is the amount of energy that each photon carries. Some ultraviolet light, and X-rays and Gamma-rays have enough energy to remove electrons from atoms as they are absorbed, forming positive and negatively charged ions. These forms of radiation are called ionizing radiation. Radio waves, microwaves, infrared and visible light do not have enough energy to ionize atoms. -

PE1128 Radiation Exposure in Medical Imaging
Radiation Exposure in Medical Imaging This handout answers questions about radiation exposure and what Seattle Children’s Hospital is doing to keep your child safe. Medical imaging uses machines and techniques to provide valuable information about your child’s health. It plays an important role in helping your doctor make the correct diagnosis. Some of these machines use radiation to get these images. We are all exposed to small amounts of radiation in normal daily life from soil, rocks, air, water and even some of the foods we eat. This is called background radiation. The amount of background radiation that you are exposed to depends on where you live and varies throughout the country. The average person in the United States receives about 3 milli-Sieverts (mSv) per year from background radiation. A mSv is a unit of measurement for radiation, like an inch is a unit of length. Which medical MRI and ultrasound do not use ionizing (high-energy) radiation to make imaging exams images. MRI uses magnets and radio waves, and ultrasound uses sound waves. use radiation? Diagnostic An X-ray is a form of energy that can pass through your child’s bones and Radiography tissues to create an image. The image created is called a radiograph, sometimes referred to as an “X-ray.” X-rays are used to detect and diagnose conditions in the body. CT scan A CT (computed tomography) scan, sometimes called a “CAT scan,” uses X-rays, special equipment, and computers to make pictures that provide a multidimensional view of a body part.