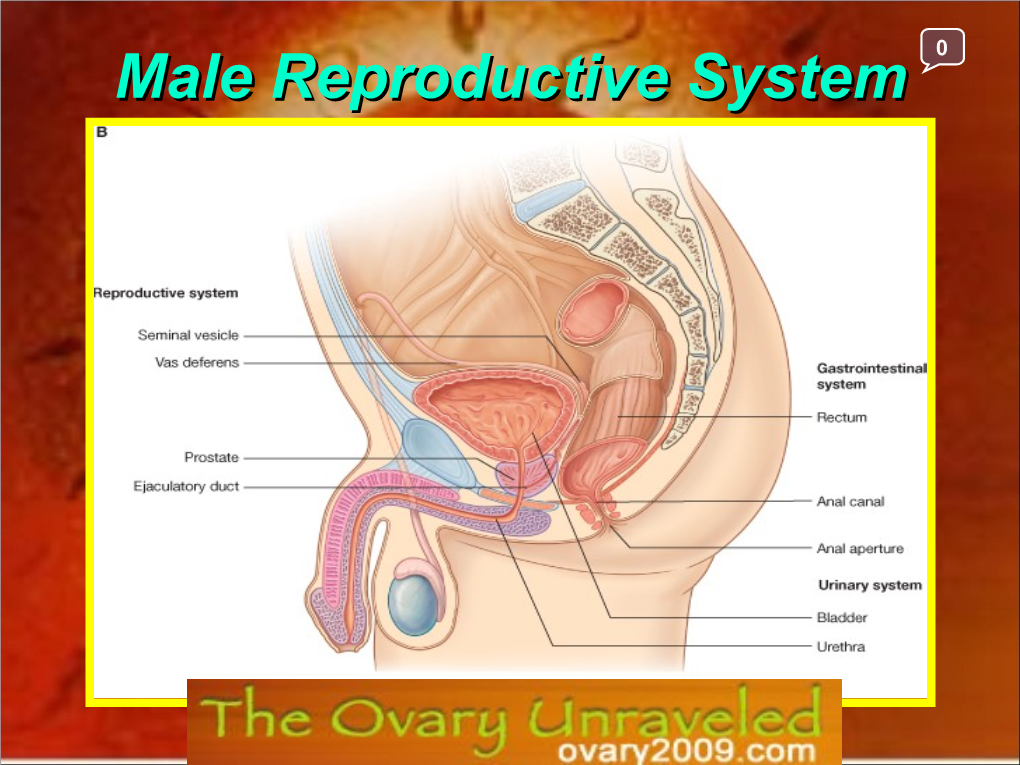
Male Reproductive System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Morphology of the Male Reproductive Tract in the Water Scavenger Beetle Tropisternus Collaris Fabricius, 1775 (Coleoptera: Hydrophilidae)
Revista Brasileira de Entomologia 65(2):e20210012, 2021 Morphology of the male reproductive tract in the water scavenger beetle Tropisternus collaris Fabricius, 1775 (Coleoptera: Hydrophilidae) Vinícius Albano Araújo1* , Igor Luiz Araújo Munhoz2, José Eduardo Serrão3 1Universidade Federal do Rio de Janeiro, Instituto de Biodiversidade e Sustentabilidade (NUPEM), Macaé, RJ, Brasil. 2Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brasil. 3Universidade Federal de Viçosa, Departamento de Biologia Geral, Viçosa, MG, Brasil. ARTICLE INFO ABSTRACT Article history: Members of the Hydrophilidae, one of the largest families of aquatic insects, are potential models for the Received 07 February 2021 biomonitoring of freshwater habitats and global climate change. In this study, we describe the morphology of Accepted 19 April 2021 the male reproductive tract in the water scavenger beetle Tropisternus collaris. The reproductive tract in sexually Available online 12 May 2021 mature males comprised a pair of testes, each with at least 30 follicles, vasa efferentia, vasa deferentia, seminal Associate Editor: Marcela Monné vesicles, two pairs of accessory glands (a bean-shaped pair and a tubular pair with a forked end), and an ejaculatory duct. Characters such as the number of testicular follicles and accessory glands, as well as their shape, origin, and type of secretion, differ between Coleoptera taxa and have potential to help elucidate reproductive strategies and Keywords: the evolutionary history of the group. Accessory glands Hydrophilid Polyphaga Reproductive system Introduction Coleoptera is the most diverse group of insects in the current fauna, The evolutionary history of Coleoptera diversity (Lawrence et al., with about 400,000 described species and still thousands of new species 1995; Lawrence, 2016) has been grounded in phylogenies with waiting to be discovered (Slipinski et al., 2011; Kundrata et al., 2019). -

The Male Body
Fact Sheet The Male Body What is the male What is the epididymis? reproductive system? The epididymis is a thin highly coiled tube (duct) A man’s fertility and sexual characteristics depend that lies at the back of each testis and connects on the normal functioning of the male reproductive the seminiferous tubules in the testis to another system. A number of individual organs act single tube called the vas deferens. together to make up the male reproductive 1 system; some are visible, such as the penis and the 6 scrotum, whereas some are hidden within the body. The brain also has an important role in controlling 7 12 reproductive function. 2 8 1 11 What are the testes? 3 6 The testes (testis: singular) are a pair of egg 9 7 12 shaped glands that sit in the scrotum next to the 2 8 base of the penis on the outside of the body. In 4 10 11 adult men, each testis is normally between 15 and 3 35 mL in volume. The testes are needed for the 5 male reproductive system to function normally. 9 The testes have two related but separate roles: 4 10 • to make sperm 5 1 Bladder • to make testosterone. 2 Vas deferens The testes develop inside the abdomen in the 3 Urethra male fetus and then move down (descend) into the scrotum before or just after birth. The descent 4 Penis of the testes is important for fertility as a cooler 5 Scrotum temperature is needed to make sperm and for 16 BladderSeminal vesicle normal testicular function. -

Anatomy and Physiology Male Reproductive System References
DEWI PUSPITA ANATOMY AND PHYSIOLOGY MALE REPRODUCTIVE SYSTEM REFERENCES . Tortora and Derrickson, 2006, Principles of Anatomy and Physiology, 11th edition, John Wiley and Sons Inc. Medical Embryology Langeman, pdf. Moore and Persaud, The Developing Human (clinically oriented Embryologi), 8th edition, Saunders, Elsevier, . Van de Graff, Human anatomy, 6th ed, Mcgraw Hill, 2001,pdf . Van de Graff& Rhees,Shaum_s outline of human anatomy and physiology, Mcgraw Hill, 2001, pdf. WHAT IS REPRODUCTION SYSTEM? . Unlike other body systems, the reproductive system is not essential for the survival of the individual; it is, however, required for the survival of the species. The RS does not become functional until it is “turned on” at puberty by the actions of sex hormones sets the reproductive system apart. The male and female reproductive systems complement each other in their common purpose of producing offspring. THE TOPIC : . 1. Gamet Formation . 2. Primary and Secondary sex organ . 3. Male Reproductive system . 4. Female Reproductive system . 5. Female Hormonal Cycle GAMET FORMATION . Gamet or sex cells are the functional reproductive cells . Contain of haploid (23 chromosomes-single) . Fertilizationdiploid (23 paired chromosomes) . One out of the 23 pairs chromosomes is the determine sex sex chromosome X or Y . XXfemale, XYmale Gametogenesis Oocytes Gameto Spermatozoa genesis XY XX XX/XY MALE OR FEMALE....? Male Reproductive system . Introduction to the Male Reproductive System . Scrotum . Testes . Spermatic Ducts, Accessory Reproductive Glands,and the Urethra . Penis . Mechanisms of Erection, Emission, and Ejaculation The urogenital system . Functionally the urogenital system can be divided into two entirely different components: the urinary system and the genital system. -

Diagnosis and Management of Infertility Due to Ejaculatory Duct Obstruction: Summary Evidence ______
Vol. 47 (4): 868-881, July - August, 2021 doi: 10.1590/S1677-5538.IBJU.2020.0536 EXPERT OPINION Diagnosis and management of infertility due to ejaculatory duct obstruction: summary evidence _______________________________________________ Arnold Peter Paul Achermann 1, 2, 3, Sandro C. Esteves 1, 2 1 Departmento de Cirurgia (Disciplina de Urologia), Universidade Estadual de Campinas - UNICAMP, Campinas, SP, Brasil; 2 ANDROFERT, Clínica de Andrologia e Reprodução Humana, Centro de Referência para Reprodução Masculina, Campinas, SP, Brasil; 3 Urocore - Centro de Urologia e Fisioterapia Pélvica, Londrina, PR, Brasil INTRODUCTION tion or perineal pain exacerbated by ejaculation and hematospermia (3). These observations highlight the Infertility, defined as the failure to conceive variability in clinical presentations, thus making a after one year of unprotected regular sexual inter- comprehensive workup paramount. course, affects approximately 15% of couples worl- EDO is of particular interest for reproduc- dwide (1). In about 50% of these couples, the male tive urologists as it is a potentially correctable factor, alone or combined with a female factor, is cause of male infertility. Spermatogenesis is well- contributory to the problem (2). Among the several -preserved in men with EDO owing to its obstruc- male infertility conditions, ejaculatory duct obstruc- tive nature, thus making it appealing to relieve the tion (EDO) stands as an uncommon causative factor. obstruction and allow these men the opportunity However, the correct diagnosis and treatment may to impregnate their partners naturally. This review help the affected men to impregnate their partners aims to update practicing urologists on the current naturally due to its treatable nature. methods for diagnosis and management of EDO. -

THE UNIVERSITY of EDINBURGH
THE UNIVERSITY of EDINBURGH Title Urethroscopy: an aid to diagnosis, treatment and prognosis of urethral conditions in the male due to gonorrhoea Author McFarlane, Wilfrid Qualification MD Year 1919 Thesis scanned from best copy available: may contain faint or blurred text, and/or cropped or missing pages. Digitisation Notes: • Page 8 of Supplement at back is missing Scanned as part of the PhD Thesis Digitisation project http://librarvblogs.is.ed.ac.uk/phddigitisation URETHROSCOPY an aid to Diagnosis, Treatment and Prognosis of Urethral Conditions in the Male due to GONORRHOEA. "by Wilfrid McFarlane, M.C., M.B., Ch.E. (Edin) L.R.C.P. & S.E. M.O. 9. Stationary Hospital, Havre. 1916 M.O. i/c Gonorrhoeal Division, Military Hospital, Hemel Hempstead. 1918 M.O. Venereal Hospital, Cambridge. Thesis for"the Degree of M.D. - f 1• THE ANATOMY AMD HISTOLOGY OF THE URETHRA AND THE PATHOLOGY OF GONORRHOEA. In order to make a correct diagnosis and to carry out a sound treatment of any disease it is essential to have an accurate knowledge of the anatomy of the l • organ affected and of the pathology of the disease affecting it. THE -ANATOMY OF THE MALE URETHRA. It is merely necessary to bring out those points which will enable one to understand the effect of Gonorrhoea on the urethra, especially in longstanding cases. The urethra is the channel by which urine passes from the bladder to the outside. Into this channel open the ejaculatory ducts and thus it acts also as a passage for the spermatic fluid. In its course from the neck of the bladder to the root of the penis the urethra describes a curve, the concavity of which looks upwards and forwards. -

Case Based Urology Learning Program
Case Based Urology Learning Program Resident’s Corner: UROLOGY Case Number 11 CBULP 2011‐038 Case Based Urology Learning Program Editor: Steven C. Campbell, MD PhD Cleveland Clinic Associate Editors: Jonathan H. Ross, MD Rainbow Babies & Children’s Hospital, UH David A. Goldfarb, MD Cleveland Clinic Howard B. Goldman, MD Cleveland Clinic Manager: Nikki Williams Cleveland Clinic Case Contributors: Edmund Y. Ko, MD and Edmund S. Sabanegh, Jr., MD Cleveland Clinic A 26‐year‐old‐male presents with a 1‐year history of infertility. His healthy wife is 26‐years‐old, has normal 28‐day menstrual cycles, and has never been pregnant. The patient states that his ejaculate volume has consisted of only a few drops of semen for as long as he can remember. He has a normal libido and denies erectile dysfunction. What other history is particularly relevant? What other history is particularly relevant? The patient denies any prior evaluation for this problem, which falls under the category of infertility associated with low volume ejaculate. He denies having any urinary difficulties. He denies STD or GU infection. His past medical/surgical/social/family history are completely negative. He does not take any medications and has never used steroids. What physical examination findings are particularly relevant? What physical examination findings are particularly relevant? General appearance: Well‐nourished and well developed male, appears healthy Chest: No gynecomastia Tanner stage: 5 Groin exam: No hernia, no incisions Testicular exam: Bilaterally descended testicles, 20cc bilaterally, no masses Vas deferens: Easily palpable bilaterally Epididymis: Fullness to tail of the epididymis bilaterally No varicocele DRE: Small gland 15cc. -

Spermatophore Structure and Anatomy of the Ejaculatory Duct in Penaeus Setiferus, P. Duorarum, and P. Aztecus (Crustacea: Decapo
Spermatophore Structure and Anatomy of the Ejaculatory Duct in Penaeus setiferus, P. duorarum, and P. aztecus (Crustacea: Decapoda): Homologies and Functional Significance1 RAYMOND T. BAUER AND CORA E. CASH Center for Crustacean Research. University of Southwestern Louisiana, Lafayette, Louisiana, 70504-2451. U.S.A Abstract, Spermatophore structure inside the male ejaculatory duct, immediately fol lowing ejaculation, and after exposure to seawater is described and compared for three species of Penaeus. P. setiferus (external attachment of the spermatophore to an "open" thelycum of the female) and P. duorarum and P. aztecus (spermatophore storage behind a "closed" thelycum). Detailed investigation of the origin and disposition of spermatophore materials in the ejaculatory duct permits hypotheses of homologies among the species of Penaeus investigated. The sperm sac of the spermatophore of P. setiferus is homologous to the main body of the spermatophore of P. duorarum and P. aztecus. The adhesive glands and material have been lost entirely in the latter two species, and the appendages of their spermatophores are homologous to the glutinous material of P. setiferus. Structures lot mechanical attachment found in the externally attached spermatophore of P. setiferus are lost or reduced in the phylogenetically advanced P. duorarum and P. aztecus. Reduction in complexity of the spermatophore in the species with closed thelycum is postulated to have evolved concomitantly with spermatophore enclosure and storage. In the species with closed thelycum, exposure of the spermatophore to seawater causes a striking reaction, consisting of an unfolding of its "appendage." Spreading of the appendage material throughout the aperture of the seminal receptacle to insure its complete seal after insem ination is suggested as the function of the spermatophore reaction. -

The “Road Map”
PRACTICAL ROADMAP MALE REPRODUCTIVE SYSTEM DR N GRAVETT THE TESTIS • Slide 7 Stain: Iron Haematoxylin NOTE: Iron haematoxylin, a blue-black stain demonstrates the chromosomes in the dividing cells of the testis THE TESTIS Connective Tissue Septum These incomplete septae Tunica Albuginea divide the testis into lobes Seminiferous Tubule Interstitial Tissue Loose connective tissue between the seminiferous tubules THE TESTIS Tunica Tunica Albuginea Vasculosa BV Seminiferous Tubule Leydig Cells Blood Vessel (BV) Interstitial Seminiferous Tubule Tissue LEYDIG CELLS Interstitial Tissue BV Seminiferous Tubule NOTE: Leydig cells are endocrine glands and as such are usually located close to blood vessels. These cells are located outside the seminiferous tubules within the loose connective tissue stroma. SEMINIFEROUS TUBULE • Seminiferous Epithelium – Complex Stratified Epithelium consisting of 2 basic cell populations: 1. Sertoli Cells 2. Cells of the Spermatogenic Series: • Spermatogonia • Primary Spermatocyte • Secondary Spermatocyte (Transitory phase: not seen in histological section) • Early Spermatid • Late Spematid SEMINIFEROUS TUBULE Myoid Cell Sertoli Cells Primary Spermatocyte Spermato- gonium Spermato- gonium Lumen Early Spermatids Late Spematids Leydig Cell Spermato- gonium TESTIS AND EPIDIDYMIS • Slide 11 Stain: H&E NOTE: This slide is for ANAT 2020 only Pathway of sperm from point of production to exterior: Seminiferous Tubule Tubuli recti Rete Testes Efferent Ductules Epididymis Vas Deferens Ejaculatory Duct Prostatic Urethra -

Lab Ex. 59 & 61 Male Reproductive System
scrotum testis interstitial (Leydig) cells Produce testosterone Located in the connective tissue between seminiferous tubules seminiferous tubules Where sperm is produced Cross section epididymis Allows sperm to mature and stores them before ejaculation spermatic cord Contains vas deferens, blood and lymph vessels and nerves vas (ductus) deferens Muscular tube where sperm travels from the epididymis to the ejaculatory duct seminal vesicle Contributes about 60% of the fluid in semen ejaculatory duct Where the vas deferens and the duct of the seminal vesicle meet and empty into the urethra prostate gland Secretes a thin, milky fluid that makes up about 30% of the semen prostatic urethra Membranous urethra bulbourethral (Cowper’s) gland Produces a clear slippery fluid that lubricates the head of the penis The fluid also neutralizes the acidity of residual urine in the urethra that can be harmful to sperm penis penile urethra corpus cavernosum 2 cylindrical erectile tissues located on the dorsal side of the penis crus Each corpus cavernosum diverges toward the inside of the body like the arms of a Y Each arm is called a crus corpus spongiosum A single erectile body that passes along the ventral side of the penis and encloses the penile urethra bulb The corpus spongiosum terminates internally as a dilated bulb glans penis prepuce Also called foreskin sperm head acrosome A lysosome in the form of a cap that contains enzymes used to penetrate the egg DNA – 23 chromosomes Located within the nucleus in the head of the sperm midpiece tail diploid vs. haploid Diploid: contain 2 sets of chromosomes (46) Haploid: contain 1 set (half of normal) 23 . -

Reproductive System Anatomy of Male Reproductive System
Reproductive System Function: producing offspring propagation of the species ‡in terms of evolution – the only reason all the other systems exist only major system that doesn’t work continuously ‡ only activated at puberty in 7th week of embryonic development genes are activated that trigger differentiation of gonads Anatomy of Male Reproductive System Major Organs External sexual organs: penis and scrotum Internal structures form continuous tube: Testes epididymus vas deferens ejaculatory duct urethra in penis Accessory organs seminal vesicles prostate gland bulbourethral glands 1. Penis and Scrotum transfer organ glans ‡ expanded head prepuce ‡ foreskin both have modified sebaceous glands that produce waxy secretion = smegma inside penis are three cylindrical bodies called erectile tissue ‡ fill with blood during sexual arousal scrotum keeps testes at cooler temperature for sperm development 2. Testes (=testicles) Introduction to Anatomy & Physiology: Reproductive System; Ziser Lecture Notes, 2005 1 primary reproductive organ of male has dual function a. hormone secretion: ‡testosterone 1. development and maintenance of secondary sexual characteristics 2. stimulates protein synthesis 3. promotes growth of skeletal muscles b. spermatogenesis: ‡formation and maturation of sperm cells a. seminiferous tubules in cross section: seminiferous tubules appear roughly circular where sperm cells are produced b. interstitial cells are scattered between the seminiferous tubules endocrine cells ‡ testosterone 3. Epididymis epididymis is highly coiled, 18’ tube that sits on outside of testes Once produced sperm move to epididymis where they mature and are stored until “duty calls” stored sperm remain fertile for 40-60 days older sperm disintegrate and are reabsorbed by epididymis 4. Vas Deferens (=ductus deferens) a long muscular tube leading from eipdidymis in scrotum, through the inguinal canal into the pelvic cavity and around the posterior side of the bladder where it unites with ducts from the seminal vesicles 5. -

The Reproductive System
The Reproductive System The Male Reproductive System Part 1 Introduction General system functions Production of gametes Method for transfer of spermatozoa to ovum Site for fertilization Stable environment for protection and development of zygote Reproductive System Primary sex organs Testes and ovaries Produce sex cells (gametes) Secrete steroid sex hormones Androgens (males) Estrogens and progesterone (females) Accessory reproductive organs Ducts Glands External genitalia Male Reproductive System Testes Ducts Accessory glands Penis Hormonal function of the testis Ureter Urinary bladder Prostatic urethra Peritoneum Seminal Membranous vesicle urethra Ampulla of Urogenital ductus deferens diaphragm Pubis Ejaculatory Corpus duct cavernosum Rectum Corpus Prostate spongiosum Bulbourethral Spongy urethra gland Epididymis Anus Glans penis Bulb of penis Prepuce Ductus (vas) Testis External deferens Scrotum urethral orifice Copyright © 2010 Pearson Education, Inc. Figure 27.1 Testes Reside in scrotum Paired, located outside of body Descend into scrotum through inguinal canal Cryptorchidism Urinary bladder Superficial inguinal ring (end of inguinal canal) Testicular artery Spermatic cord Ductus (vas) deferens Penis Autonomic Middle septum of scrotum nerve fibers Pampiniform Cremaster muscle venous plexus External spermatic Epididymis fascia Tunica vaginalis (from peritoneum) Superficial fascia Tunica albuginea containing dartos of testis Scrotum muscle Internal spermatic Skin fascia Copyright © 2010 Pearson Education, Inc. -

Pathology and Treatment of Gonorrhea
University of Nebraska Medical Center DigitalCommons@UNMC MD Theses Special Collections 5-1-1933 Pathology and treatment of gonorrhea Luppens Albert University of Nebraska Medical Center This manuscript is historical in nature and may not reflect current medical research and practice. Search PubMed for current research. Follow this and additional works at: https://digitalcommons.unmc.edu/mdtheses Part of the Medical Education Commons Recommended Citation Albert, Luppens, "Pathology and treatment of gonorrhea" (1933). MD Theses. 610. https://digitalcommons.unmc.edu/mdtheses/610 This Thesis is brought to you for free and open access by the Special Collections at DigitalCommons@UNMC. It has been accepted for inclusion in MD Theses by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. THE PAT~OLOGY AND TREATMENT OF GONORRHEA By Albert Luppena A Senior Taeeis presented to tae Univeraity of Nebraska waioll ia one of the requirements for.tae deil'ee of Doctor of Kedioine. r CONTENTS I. History 2. A Drawini of the Kale Oro-Genital System 3. Tke Normal Anatomy of the Kale Oro-Genital Tract. 4. Kale a. Tae Keohanism of tae Gonorraeal Infection b. Tae Course of Acute Gonorraea c. Patholoi1cal Alterations in the Kale Urethral Canal d. Aoute Gonorrhea e. Severe Aoute Urethritis f. Subaoute Anterior Urethritis i• Aoute Posterior Urethritis h. Complioation1 of Acute Gonorrhea (1) Case Report• Showini Possible EtiolOiY of Oomplioations (2) Follioulitis (3) Ohordee (4) The Vasa Deferentia and the Epididymis (5) Aoute Prostatitis (6) Aoute Seminal Vesioulitis (7) Cowper's Glands (8) Gonorrheal Ophthalmia (9) Gonorrheal Cystitis (10) Gonorrheal Nephritis (11) Gonococcal Arthritis 1.