Pediatric Spinal Deformities
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Spinal Deformity Study Group
Spinal Deformity Study Group Editors in Chief Radiographic Michael F. O’Brien, MD Timothy R. Kuklo, MD Kathy M. Blanke, RN Measurement Lawrence G. Lenke, MD Manual B T2 T5 T2–T12 CSVL T5–T12 +X° -X +X° C7PL T12 L2 A S1 ©2008 Medtronic Sofamor Danek USA, Inc. – 0 + Radiographic Measurement Manual Editors in Chief Michael F. O’Brien, MD Timothy R. Kuklo, MD Kathy M. Blanke, RN Lawrence G. Lenke, MD Section Editors Keith H. Bridwell, MD Kathy M. Blanke, RN Christopher L. Hamill, MD William C. Horton, MD Timothy R. Kuklo, MD Hubert B. Labelle, MD Lawrence G. Lenke, MD Michael F. O’Brien, MD David W. Polly Jr, MD B. Stephens Richards III, MD Pierre Roussouly, MD James O. Sanders, MD ©2008 Medtronic Sofamor Danek USA, Inc. Acknowledgements Radiographic Measurement Manual The radiographic measurement manual has been developed to present standardized techniques for radiographic measurement. In addition, this manual will serve as a complimentary guide for the Spinal Deformity Study Group’s radiographic measurement software. Special thanks to the following members of the Spinal Deformity Study Group in the development of this manual. Sigurd Berven, MD Hubert B. Labelle, MD Randal Betz, MD Lawrence G. Lenke, MD Fabien D. Bitan, MD Thomas G. Lowe, MD John T. Braun, MD John P. Lubicky, MD Keith H. Bridwell, MD Steven M. Mardjetko, MD Courtney W. Brown, MD Richard E. McCarthy, MD Daniel H. Chopin, MD Andrew A. Merola, MD Edgar G. Dawson, MD Michael Neuwirth, MD Christopher DeWald, MD Peter O. Newton, MD Mohammad Diab, MD Michael F. -

Lordosis, Kyphosis, and Scoliosis
SPINAL CURVATURES: LORDOSIS, KYPHOSIS, AND SCOLIOSIS The human spine normally curves to aid in stability or balance and to assist in absorbing shock during movement. These gentle curves can be seen from the side or lateral view of the spine. When viewed from the back, the spine should run straight down the middle of the back. When there are abnormalities or changes in the natural spinal curvature, these abnormalities are named with the following conditions and include the following symptoms. LORDOSIS Some lordosis is normal in the lower portion or, lumbar section, of the human spine. A decreased or exaggerated amount of lordosis that is causing spinal instability is a condition that may affect some patients. Symptoms of Lordosis include: ● Appearance of sway back where the lower back region has a pronounced curve and looks hollow with a pronounced buttock area ● Difficulty with movement in certain directions ● Low back pain KYPHOSIS This condition is diagnosed when the patient has a rounded upper back and the spine is bent over or curved more than 50 degrees. Symptoms of Kyphosis include: ● Curved or hunched upper back ● Patient’s head that leans forward ● May have upper back pain ● Experiences upper back discomfort after movement or exercise SCOLIOSIS The most common of the three curvatures. This condition is diagnosed when the spine looks like a “s” or “c” from the back. The spine is not straight up and down but has a curve or two running side-to-side. Sagittal Balance Definition • Sagittal= front-to-back direction (sagittal plane) • Imbalance= Lack of harmony or balance Etiology • Excessive lordosis (backwards lean) or kyphosis (forward lean) • Traumatic injury • Previous spinal fusion that disrupted sagittal balance Effects • Low back pain • Difficulty walking • Inability to look straight ahead when upright The most ergonomic and natural posture is to maintain neutral balance, with the head positioned over the shoulders and pelvis. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -

The Genetic Heterogeneity of Brachydactyly Type A1: Identifying the Molecular Pathways
The genetic heterogeneity of brachydactyly type A1: Identifying the molecular pathways Lemuel Jean Racacho Thesis submitted to the Faculty of Graduate Studies and Postdoctoral Studies in partial fulfillment of the requirements for the Doctorate in Philosophy degree in Biochemistry Specialization in Human and Molecular Genetics Department of Biochemistry, Microbiology and Immunology Faculty of Medicine University of Ottawa © Lemuel Jean Racacho, Ottawa, Canada, 2015 Abstract Brachydactyly type A1 (BDA1) is a rare autosomal dominant trait characterized by the shortening of the middle phalanges of digits 2-5 and of the proximal phalange of digit 1 in both hands and feet. Many of the brachymesophalangies including BDA1 have been associated with genetic perturbations along the BMP-SMAD signaling pathway. The goal of this thesis is to identify the molecular pathways that are associated with the BDA1 phenotype through the genetic assessment of BDA1-affected families. We identified four missense mutations that are clustered with other reported BDA1 mutations in the central region of the N-terminal signaling peptide of IHH. We also identified a missense mutation in GDF5 cosegregating with a semi-dominant form of BDA1. In two families we reported two novel BDA1-associated sequence variants in BMPR1B, the gene which codes for the receptor of GDF5. In 2002, we reported a BDA1 trait linked to chromosome 5p13.3 in a Canadian kindred (BDA1B; MIM %607004) but we did not discover a BDA1-causal variant in any of the protein coding genes within the 2.8 Mb critical region. To provide a higher sensitivity of detection, we performed a targeted enrichment of the BDA1B locus followed by high-throughput sequencing. -

SCOLIOSIS: What Is New and True? Natural History, Screening/Evaluation and Treatment
SCOLIOSIS: what is new and true? Natural history, screening/evaluation and treatment Kathleen Moen MD Swedish Pediatric Specialty Update January 24, 2020 OBJECTIVES • 1) review of entity adolescent idiopathic scoliosis • 2) review the natural history of treated and untreated disease • 3) review screening recommendations and delineating patients who warrant referral • 4) review of treatment modalities Scoliosis • Definition: a lateral spinal curvature measuring at least 10 degrees on xray • Complex 3dimensional spinal deformity Adolescent Idiopathic Scoliosis • AIS: Scoliosis most often develops and progresses during the most rapid times of growth, typically between ages 10 ‐15 years. • NOT infantile or juvenile scoliosis which have different natural history profiles • NOT congenital spinal deformities, neuromuscular scoliosis or spinal dysraphism Adolescent Idiopathic Scoliosis • Classic Teaching – Small curves are common – Progression occurs during most rapid times of growth – Female predominance – Big curves get bigger – Etiology unclear: familial predisposition, and? – Idiopathic scoliosis not typically painful Adolescent Idiopathic Scoliosis • Mild scoliosis curves are common, affecting 2‐3% of the adolescent population, males and females equally • Less than 0.1% of adolescents have curves greater than 40 degrees. • Ratio of females to males 10:1 Cobb Angle Female:Male Prevalence >10 1.4‐2 :1 2 ‐ 3 % >20 5:1 .3 ‐ .5 % >30 10:1 .1 ‐ .3 % >40 10:1 <0.1% Weinstein, SL Adolescent Idiopathic Scoliosis, Prevalence and Natural History. Instructional -

Osteodystrophy-Like Syndrome Localized to 2Q37
Am. J. Hum. Genet. 56:400-407, 1995 Brachydactyly and Mental Retardation: An Albright Hereditary Osteodystrophy-like Syndrome Localized to 2q37 L. C. Wilson,"7 K. Leverton,3 M. E. M. Oude Luttikhuis,' C. A. Oley,4 J. Flint,5 J. Wolstenholme,4 D. P. Duckett,2 M. A. Barrow,2 J. V. Leonard,6 A. P. Read,3 and R. C. Trembath' 'Departments of Genetics and Medicine, University of Leicester, and 2Leicestershire Genetics Centre, Leicester Royal Infirmary, Leicester, 3Department of Medical Genetics, St Mary's Hospital, Manchester. 4Department of Human Genetics, University of Newcastle upon Tyne, Newcastle upon Tyne; 5MRC Molecular Haematology Unit, Institute of Molecular Medicine, Oxford; and 6Medical Unit and 7Mothercare Unit for Clinical Genetics and Fetal Medicine, Institute of Child Health, London Summary The physical feature brachymetaphalangia refers to shortening of either the metacarpals and phalanges of the We report five patients with a combination ofbrachymeta- hands or of the equivalent bones in the feet. The combina- phalangia and mental retardation, similar to that observed tion of brachymetaphalangia and mental retardation occurs in Albright hereditary osteodystrophy (AHO). Four pa- in Albright hereditary osteodystrophy (AHO) (Albright et tients had cytogenetically visible de novo deletions of chro- al. 1942), a dysmorphic syndrome that is also associated mosome 2q37. The fifth patient was cytogenetically nor- with cutaneous ossification (in si60% of cases [reviewed by mal and had normal bioactivity of the a subunit of Gs Fitch 1982]); round face; and short, stocky build. Affected (Gsa), the protein that is defective in AHO. In this patient, individuals with AHO may have either pseudohypopara- we have used a combination of highly polymorphic molec- thyroidism (PHP), with end organ resistance to parathyroid ular markers and FISH to demonstrate a microdeletion at hormone (PTH) and certain other cAMP-dependent hor- 2q37. -
Macrocephaly Information Sheet 6-13-19
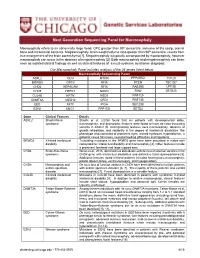
Next Generation Sequencing Panel for Macrocephaly Clinical Features: Macrocephaly refers to an abnormally large head, OFC greater than 98th percentile, inclusive of the scalp, cranial bone and intracranial contents. Megalencephaly, brain weight/volume ratio greater than 98th percentile, results from true enlargement of the brain parenchyma [1]. Megalencephaly is typically accompanied by macrocephaly, however macrocephaly can occur in the absence of megalencephaly [2]. Both macrocephaly and megalencephaly can been seen as isolated clinical findings as well as clinical features of a mutli-systemic syndromic diagnosis. Our Macrocephaly Panel includes analysis of the 36 genes listed below. Macrocephaly Sequencing Panel ASXL2 GLI3 MTOR PPP2R5D TCF20 BRWD3 GPC3 NFIA PTEN TBC1D7 CHD4 HEPACAM NFIX RAB39B UPF3B CHD8 HERC1 NONO RIN2 ZBTB20 CUL4B KPTN NSD1 RNF125 DNMT3A MED12 OFD1 RNF135 EED MITF PIGA SEC23B EZH2 MLC1 PPP1CB SETD2 Gene Clinical Features Details ASXL2 Shashi-Pena Shashi et al. (2016) found that six patients with developmental delay, syndrome macrocephaly, and dysmorphic features were found to have de novo truncating variants in ASXL2 [3]. Distinguishing features were macrocephaly, absence of growth retardation, and variability in the degree of intellectual disabilities The phenotype also consisted of prominent eyes, arched eyebrows, hypertelorism, a glabellar nevus flammeus, neonatal feeding difficulties and hypotonia. BRWD3 X-linked intellectual Truncating mutations in the BRWD3 gene have been described in males with disability nonsyndromic intellectual disability and macrocephaly [4]. Other features include a prominent forehead and large cupped ears. CHD4 Sifrim-Hitz-Weiss Weiss et al., 2016, identified five individuals with de novo missense variants in the syndrome CHD4 gene with intellectual disabilities and distinctive facial dysmorphisms [5]. -

Kyphectomy in Neonates with Meningomyelocele
Child's Nervous System (2019) 35:673–681 https://doi.org/10.1007/s00381-018-4006-4 ORIGINAL PAPER Kyphectomy in neonates with meningomyelocele Nail Özdemir1 & Senem Alkan Özdemir2 & Esra Arun Özer3 Received: 18 August 2018 /Accepted: 18 November 2018 /Published online: 11 December 2018 # Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract Purpose Kyphosis is the most severe spinal deformity associated with meningomyelocele (MMC) and is seen in approximately 15% of neonates. Our purpose is to present our clinical experience, to discuss the technique and deformity correction in kyphectomy in neonates with MMC, and to assess its long-term outcomes. Method In this prospective study, the authors reviewed eight cases submitted to surgery between 2013 and 2015. We evaluated clinical characteristics that were analyzed, as were the operative technique employed, and angle range of the kyphosis deformity postcorrection follow-up. Results Neonatal kyphectomy was performed of six females and two males. The mean birth weight was 2780 g, and the mean age at the time of surgery was 5.6 days. There were S-shaped type deformity in lumbar region in all neonates. In the correction of the kyphotic deformity, a total vertebrae were removed from four patient, whereas a partial vertebrectomy was done in four. The mean operative time was 116 min. No patients did not require the blood transfusion. There were no serious complications, and wound closure was successful in all patients. The mean follow-up period was 4 years and 3 months (range 36–61 months), except one patient who died 1 week after discharge. -

Failure to Maintain Segmental Lordosis During TLIF for One-Level
European Spine Journal (2019) 28:745–750 https://doi.org/10.1007/s00586-019-05890-w ORIGINAL ARTICLE Failure to maintain segmental lordosis during TLIF for one‑level degenerative spondylolisthesis negatively afects clinical outcome 5 years postoperatively: a prospective cohort of 57 patients Matevž Kuhta1 · Klemen Bošnjak2 · Rok Vengust2 Received: 14 June 2018 / Revised: 28 November 2018 / Accepted: 13 January 2019 / Published online: 24 January 2019 © Springer-Verlag GmbH Germany, part of Springer Nature 2019 Abstract Purpose The present study aimed to determine whether obtaining adequate lumbar (LL) or segmental (SL) lordosis during instrumented TLIF for one-level degenerative spondylolisthesis afects midterm clinical outcome. Methods The study was designed as a prospective one, including 57 patients who underwent single-level TLIF surgery for degenerative spondylolisthesis. Patients were analyzed globally with additional subgroup analysis according to pelvic incidence (PI). Radiographic analysis of spinopelvic sagittal parameters was conducted pre- and postoperatively. Clinical examination including ODI score was performed preoperatively, 1 and 5 years postoperatively. Results Signifcant improvement in ODI scores at 1 and 5 years postoperatively (p < 0.001) was demonstrated. There was a signifcant correlation between anterior shift of SVA and failure to improve SL (p = 0.046). Moreover, anterior SVA shift correlated with increased values of ODI score both 1 and 5 years postoperatively. In low-PI group, failure to correct LL correlated with high ODI scores 5 years postoperatively (r = − 0.499, p = 0.005). Conclusions Failure to correct segmental lordosis during surgery for one-level degenerative spondylolisthesis resulted in anterior displacement of the center of gravity, which in turn correlated with unfavorable clinical outcome 1 and 5 years postoperatively. -

Scoliosis in Paraplegia
Paraplegia (1974), II, 290-292 SCOLIOSIS IN PARAPLEGIA By JOHN A. ODOM, JR., M.D. and COURTN EY W. BROWN, M.D. Children's Hospital, Denver, Colorado in conjunction with ROBERT R. JACKSON, M.D., HARRY R. HA HN, M.D. and TERRY V. CARLE, M.D. Craig Rehabilitation Hospital, Englewood, Colorado WITH the increasing instance of excellent medical care, more children with traumatic paraplegia and myelomeningocele with paraplegia live to adulthood. In these two groups of patients there is a high instance of scoliosis, kyphosis and lordosis. Much attention in the past years has been placed on hips and feet but only in the last decade has there been much attention concentrated on the treatment of the spines of these patients. Most of this attention has been toward the patient with a traumatic paraplegia with development of scoliosis. Some attempts have been made at fusing the scoliotic spine of myelomeningo celes by Harrington Instrumentation but with a rather high instance of complica tions and failures. With the event of anterior instrumentation by Dr. Alan Dwyer of Sydney, Australia, the anterior approach to the spine is becoming widely accepted and very successfully used. This is especially valuable in the correction and fusion of the spine with no posterior elements from birth. MATERIAL FOR STUDY Between March of 1971 and June of 1973, there have been 26 paraplegics with scoliosis who have been cared for by the authors. All of these patients have either been myelomeningoceles with paraplegia or spinal cord injuries, all of whom have had scoliosis, kyphosis, or severe lordosis. -

An Unusual Cause of Back Pain in Osteoporosis: Lessons from a Spinal Lesion
Ann Rheum Dis 1999;58:327–331 327 MASTERCLASS Series editor: John Axford Ann Rheum Dis: first published as 10.1136/ard.58.6.327 on 1 June 1999. Downloaded from An unusual cause of back pain in osteoporosis: lessons from a spinal lesion S Venkatachalam, Elaine Dennison, Madeleine Sampson, Peter Hockey, MIDCawley, Cyrus Cooper Case report A 77 year old woman was admitted with a three month history of worsening back pain, malaise, and anorexia. On direct questioning, she reported that she had suVered from back pain for four years. The thoracolumbar radiograph four years earlier showed T6/7 vertebral collapse, mild scoliosis, and degenerative change of the lumbar spine (fig 1); but other investigations at that time including the eryth- rocyte sedimentation rate (ESR) and protein electophoresis were normal. Bone mineral density then was 0.914 g/cm2 (T score = −2.4) at the lumbar spine, 0.776 g/cm2 (T score = −1.8) at the right femoral neck and 0.738 g/cm2 (T score = −1.7) at the left femoral neck. She was given cyclical etidronate after this vertebral collapse as she had suVered a previous fragility fracture of the left wrist. On admission, she was afebrile, but general examination was remarkable for pallor, dental http://ard.bmj.com/ caries, and cellulitis of the left leg. A pansysto- lic murmur was heard at the cardiac apex on auscultation; there were no other signs of bac- terial endocarditis. She had kyphoscoliosis and there was diVuse tenderness of the thoraco- lumbar spine. Her neurological examination was unremarkable. on September 29, 2021 by guest. -
Differential Diagnosis Functional Vs Structural Scoliosis
Differential Diagnosis Functional vs Structural Scoliosis James J. Lehman, DC, MBA, FACO Associate Professor of Clinical Sciences University of Bridgeport College of Chiropractic Director Community Health Clinical Education University of Bridgeport Diagnosis is the key to successful treatment Scoliosis Classification Based upon the findings with this postural presentation, what physical examination procedures would you perform to determine your working diagnosis for the child with scoliosis? Classification of Scoliosis Structural or Nonstructural (functional) 1. Structural curves are fixed, nonflexible, and fail to correct with bending. 2. Nonstructural curves are not fixed but flexible and readily correct with bending. Postural Evaluation of Spine • Observation of standing posture • Right thoracic curve is most common with best prognosis Adam’s Position Differential Diagnosis Functional Scoliosis/Postural Imbalance Pelvic Obliquity and Postural Imbalance • You must determine whether the leg length discrepancy is anatomical or functional Actual Leg-Length Test • This is a tape measurement that tests for anatomical leg length discrepancy. • ASIS and medial malleolus are the landmarks identified Apparent Leg-Length Test • Reveals functional leg length discrepancy • Umbillicus and medial malleolus are landmarks • Evans Functional Leg-Length Measurement • Measure length of both lower extremities supine and seated • Inferior medial malloli are used as landmarks • Read the body language Functional Leg-Length Measurement • Usually the ipsilateral malleolus will measure short when supine if the superior iliac crest appears inferior when standing and long when seated Clinical Value of Long Sit Test • Pelvic Obliquity • Leg Length Discrepancy – Functional – Anatomical • SIJ Dysfunction • Spinal manipulation VIDEO: SUPINE TO LONG SIT TEST HTTP://WWW.THESTUDENTPHYSICALTHERAPIST.COM/SUPINE-TO-LONG- SIT-TEST.HTML LEVANGIE PK.