SCOLIOSIS: What Is New and True? Natural History, Screening/Evaluation and Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Lordosis, Kyphosis, and Scoliosis
SPINAL CURVATURES: LORDOSIS, KYPHOSIS, AND SCOLIOSIS The human spine normally curves to aid in stability or balance and to assist in absorbing shock during movement. These gentle curves can be seen from the side or lateral view of the spine. When viewed from the back, the spine should run straight down the middle of the back. When there are abnormalities or changes in the natural spinal curvature, these abnormalities are named with the following conditions and include the following symptoms. LORDOSIS Some lordosis is normal in the lower portion or, lumbar section, of the human spine. A decreased or exaggerated amount of lordosis that is causing spinal instability is a condition that may affect some patients. Symptoms of Lordosis include: ● Appearance of sway back where the lower back region has a pronounced curve and looks hollow with a pronounced buttock area ● Difficulty with movement in certain directions ● Low back pain KYPHOSIS This condition is diagnosed when the patient has a rounded upper back and the spine is bent over or curved more than 50 degrees. Symptoms of Kyphosis include: ● Curved or hunched upper back ● Patient’s head that leans forward ● May have upper back pain ● Experiences upper back discomfort after movement or exercise SCOLIOSIS The most common of the three curvatures. This condition is diagnosed when the spine looks like a “s” or “c” from the back. The spine is not straight up and down but has a curve or two running side-to-side. Sagittal Balance Definition • Sagittal= front-to-back direction (sagittal plane) • Imbalance= Lack of harmony or balance Etiology • Excessive lordosis (backwards lean) or kyphosis (forward lean) • Traumatic injury • Previous spinal fusion that disrupted sagittal balance Effects • Low back pain • Difficulty walking • Inability to look straight ahead when upright The most ergonomic and natural posture is to maintain neutral balance, with the head positioned over the shoulders and pelvis. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ► -
Macrocephaly Information Sheet 6-13-19
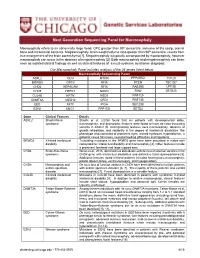
Next Generation Sequencing Panel for Macrocephaly Clinical Features: Macrocephaly refers to an abnormally large head, OFC greater than 98th percentile, inclusive of the scalp, cranial bone and intracranial contents. Megalencephaly, brain weight/volume ratio greater than 98th percentile, results from true enlargement of the brain parenchyma [1]. Megalencephaly is typically accompanied by macrocephaly, however macrocephaly can occur in the absence of megalencephaly [2]. Both macrocephaly and megalencephaly can been seen as isolated clinical findings as well as clinical features of a mutli-systemic syndromic diagnosis. Our Macrocephaly Panel includes analysis of the 36 genes listed below. Macrocephaly Sequencing Panel ASXL2 GLI3 MTOR PPP2R5D TCF20 BRWD3 GPC3 NFIA PTEN TBC1D7 CHD4 HEPACAM NFIX RAB39B UPF3B CHD8 HERC1 NONO RIN2 ZBTB20 CUL4B KPTN NSD1 RNF125 DNMT3A MED12 OFD1 RNF135 EED MITF PIGA SEC23B EZH2 MLC1 PPP1CB SETD2 Gene Clinical Features Details ASXL2 Shashi-Pena Shashi et al. (2016) found that six patients with developmental delay, syndrome macrocephaly, and dysmorphic features were found to have de novo truncating variants in ASXL2 [3]. Distinguishing features were macrocephaly, absence of growth retardation, and variability in the degree of intellectual disabilities The phenotype also consisted of prominent eyes, arched eyebrows, hypertelorism, a glabellar nevus flammeus, neonatal feeding difficulties and hypotonia. BRWD3 X-linked intellectual Truncating mutations in the BRWD3 gene have been described in males with disability nonsyndromic intellectual disability and macrocephaly [4]. Other features include a prominent forehead and large cupped ears. CHD4 Sifrim-Hitz-Weiss Weiss et al., 2016, identified five individuals with de novo missense variants in the syndrome CHD4 gene with intellectual disabilities and distinctive facial dysmorphisms [5]. -

Scoliosis in Paraplegia
Paraplegia (1974), II, 290-292 SCOLIOSIS IN PARAPLEGIA By JOHN A. ODOM, JR., M.D. and COURTN EY W. BROWN, M.D. Children's Hospital, Denver, Colorado in conjunction with ROBERT R. JACKSON, M.D., HARRY R. HA HN, M.D. and TERRY V. CARLE, M.D. Craig Rehabilitation Hospital, Englewood, Colorado WITH the increasing instance of excellent medical care, more children with traumatic paraplegia and myelomeningocele with paraplegia live to adulthood. In these two groups of patients there is a high instance of scoliosis, kyphosis and lordosis. Much attention in the past years has been placed on hips and feet but only in the last decade has there been much attention concentrated on the treatment of the spines of these patients. Most of this attention has been toward the patient with a traumatic paraplegia with development of scoliosis. Some attempts have been made at fusing the scoliotic spine of myelomeningo celes by Harrington Instrumentation but with a rather high instance of complica tions and failures. With the event of anterior instrumentation by Dr. Alan Dwyer of Sydney, Australia, the anterior approach to the spine is becoming widely accepted and very successfully used. This is especially valuable in the correction and fusion of the spine with no posterior elements from birth. MATERIAL FOR STUDY Between March of 1971 and June of 1973, there have been 26 paraplegics with scoliosis who have been cared for by the authors. All of these patients have either been myelomeningoceles with paraplegia or spinal cord injuries, all of whom have had scoliosis, kyphosis, or severe lordosis. -
Differential Diagnosis Functional Vs Structural Scoliosis
Differential Diagnosis Functional vs Structural Scoliosis James J. Lehman, DC, MBA, FACO Associate Professor of Clinical Sciences University of Bridgeport College of Chiropractic Director Community Health Clinical Education University of Bridgeport Diagnosis is the key to successful treatment Scoliosis Classification Based upon the findings with this postural presentation, what physical examination procedures would you perform to determine your working diagnosis for the child with scoliosis? Classification of Scoliosis Structural or Nonstructural (functional) 1. Structural curves are fixed, nonflexible, and fail to correct with bending. 2. Nonstructural curves are not fixed but flexible and readily correct with bending. Postural Evaluation of Spine • Observation of standing posture • Right thoracic curve is most common with best prognosis Adam’s Position Differential Diagnosis Functional Scoliosis/Postural Imbalance Pelvic Obliquity and Postural Imbalance • You must determine whether the leg length discrepancy is anatomical or functional Actual Leg-Length Test • This is a tape measurement that tests for anatomical leg length discrepancy. • ASIS and medial malleolus are the landmarks identified Apparent Leg-Length Test • Reveals functional leg length discrepancy • Umbillicus and medial malleolus are landmarks • Evans Functional Leg-Length Measurement • Measure length of both lower extremities supine and seated • Inferior medial malloli are used as landmarks • Read the body language Functional Leg-Length Measurement • Usually the ipsilateral malleolus will measure short when supine if the superior iliac crest appears inferior when standing and long when seated Clinical Value of Long Sit Test • Pelvic Obliquity • Leg Length Discrepancy – Functional – Anatomical • SIJ Dysfunction • Spinal manipulation VIDEO: SUPINE TO LONG SIT TEST HTTP://WWW.THESTUDENTPHYSICALTHERAPIST.COM/SUPINE-TO-LONG- SIT-TEST.HTML LEVANGIE PK. -

Complications and Radiographic Correction in Adult Scoliosis
Neurosurg Focus 28 (3):E7, 2010 Complications and radiographic correction in adult scoliosis following combined transpsoas extreme lateral interbody fusion and posterior pedicle screw instrumentation MATTHEW J. TOR M ENTI , M.D., MATTHEW B. MASERATI , M.D., CHRISTOPHER M. BONFIEL D , M.D., DAVI D O. OKONKWO , M.D., PH.D., AN D AD A M S. KANTER , M.D. Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, Pennsylvania Object. The authors recently used a combined approach of minimally invasive transpsoas extreme lateral in- terbody fusion (XLIF) and open posterior segmental pedicle screw instrumentation with transforaminal lumbar in- terbody fusion (TLIF) for the correction of coronal deformity. The complications and radiographic outcomes were compared with a posterior-only approach for scoliosis correction. Methods. The authors retrospectively reviewed all deformity cases that were surgically corrected at the Uni- versity of Pittsburgh Medical Center Presbyterian Hospital between June 2007 and August 2009. Eight patients underwent combined transpsoas and posterior approaches for adult degenerative thoracolumbar scoliosis. The com- parison group consisted of 4 adult patients who underwent a posterior-only scoliosis correction. Data on intra- and postoperative complications were collected. The pre- and postoperative posterior-anterior and lateral scoliosis series radiographic films were reviewed, and comparisons were made for coronal deformity, apical vertebral translation (AVT), and lumbar lordosis. Clinical outcomes were evaluated by comparing pre- and postoperative visual analog scale scores. Results. The median preoperative coronal Cobb angle in the combined approach was 38.5° (range 18–80°). Fol- lowing surgery, the median Cobb angle was 10° (p < 0.0001). The mean preoperative AVT was 3.6 cm, improving to 1.8 cm postoperatively (p = 0.031). -

Degenerative Spondylolisthesis
AN INTRODUCTION TO DEGENERATIVE SPONDYLOLISTHESIS This booklet is designed to inform you about lumbar degenerative spondylolisthesis. It is not meant to replace any personal conversations that you might wish to have with your physician or other member of your healthcare team. Not all the information here will apply to your individual treatment or its outcome. The information is intended to answer some of your questions and serve as a stimulus for you to ask appropriate questions about spinal alignment and spine surgery. About the Spine CERVICAL The human spine is comprised of the cervical (neck) spine, the thoracic (chest) spine, the lumbar (lower back) spine, and sacral THORACIC bones. The entire spine is made up of 24 bones, called vertebrae. These vertebrae are connected by several joints, which allow you to LUMBAR bend, twist, and carry loads. The main joint between two vertebrae is called an intervertebral disc. The disc is comprised of two parts, a tough and fibrous outer layer (annulus fibrosis) and a soft, gelatinous center (nucleus pulposus). These two parts work in conjunction to allow the spine to move, and also provide shock absorption. INTERVERTEBRAL ANNULUS DISC FIBROSIS SPINAL NERVES NUCLEUS PULPOSUS What is Degenerative Spondylolisthesis? Degenerative spondylolisthesis is a condition where the intervertebral disc degenerates resulting in a loss of disc height and instability, causing one vertebra to slip forward over another vertebra below it. The word spondylolisthesis is comprised of two parts: spondylo meaning spine, and listhesis meaning slippage. This condition can cause impingement of the spinal nerves and/or fatigue of the back muscles, and may result in lower back and/or leg pain. -

Saethre–Chotzen Syndrome Caused by TWIST 1 Gene Mutations: Functional Differentiation from Muenke Coronal Synostosis Syndrome
European Journal of Human Genetics (2006) 14, 39–48 & 2006 Nature Publishing Group All rights reserved 1018-4813/06 $30.00 www.nature.com/ejhg ARTICLE Saethre–Chotzen syndrome caused by TWIST 1 gene mutations: functional differentiation from Muenke coronal synostosis syndrome Wolfram Kress*,1, Christian Schropp2, Gabriele Lieb2, Birgit Petersen2, Maria Bu¨sse-Ratzka2, Ju¨rgen Kunz3, Edeltraut Reinhart4, Wolf-Dieter Scha¨fer5, Johanna Sold5, Florian Hoppe6, Jan Pahnke6, Andreas Trusen7, Niels So¨rensen8,Ju¨rgen Krauss8 and Hartmut Collmann8 1Institute of Human Genetics, University of Wu¨rzburg, Wu¨rzburg, Germany; 2Department of Pediatrics, University of Wu¨rzburg, Wu¨rzburg, Germany; 3Institute of Human Genetics, University of Marburg, Marburg, Germany; 4Department of Maxillo-facial Surgery, University of Wu¨rzburg, Wu¨rzburg, Germany; 5Department of Ophthalmology, University of Wu¨rzburg, Wu¨rzburg, Germany; 6Department of Otorhinolaryngology, University of Wu¨rzburg, Wu¨rzburg, Germany; 7Department of Diagnostic Radiology, University of Wu¨rzburg, Wu¨rzburg, Germany; 8Sect. Pediatric Neurosurgery, University of Wu¨rzburg, Wu¨rzburg, Germany The Saethre–Chotzen syndrome (SCS) is an autosomal dominant craniosynostosis syndrome with uni- or bilateral coronal synostosis and mild limb deformities. It is caused by loss-of-function mutations of the TWIST 1 gene. In an attempt to delineate functional features separating SCS from Muenke’s syndrome, we screened patients presenting with coronal suture synostosis for mutations in the TWIST 1 gene, and for the Pro250Arg mutation in FGFR3. Within a total of 124 independent pedigrees, 39 (71 patients) were identified to carry 25 different mutations of TWIST 1 including 14 novel mutations, to which six whole gene deletions were added. -

The Effect of Minimally Invasive Pectus Excavatum Repair on Thoracic Scoliosis
European Journal of Cardio-Thoracic Surgery 59 (2021) 375–381 ORIGINAL ARTICLE doi:10.1093/ejcts/ezaa328 Advance Access publication 30 October 2020 Cite this article as: Is¸can_ M, Kılıc¸ B, Turna A, Kaynak MK. The effect of minimally invasive pectus excavatum repair on thoracic scoliosis. Eur J Cardiothorac Surg 2021;59:375–81. The effect of minimally invasive pectus excavatum repair on thoracic scoliosis Mehlika Is¸can_ a,*, Burcu Kılıc¸b, Akif Turna b and Mehmet Kamil Kaynak b a Department of Thoracic Surgery, Gebze Fatih State Hospital, Kocaeli, Turkey b Department of Thoracic Surgery, Istanbul University-Cerrahpas¸a,Cerrahpas¸aSchool of Medicine, Istanbul, Turkey Downloaded from https://academic.oup.com/ejcts/article/59/2/375/5943430 by guest on 29 September 2021 * Corresponding author. Department of Thoracic Surgery, Gebze Fatih State Hospital, 41400 Gebze - Kocaeli, Turkey. Tel: +90-543-6609334; e-mail: [email protected] (M. Is¸can)._ Received 13 March 2020; received in revised form 17 July 2020; accepted 23 July 2020 THORACIC Abstract OBJECTIVES: The Nuss technique comprises the placement of an intrathoracic bar behind the sternum. However, besides improving the body posture through the correction of the pectus excavatum (PE), this procedure may cause or worsen thoracic scoliosis as a result of the considerable stress loaded on the chest wall and the thorax. Our goal was to investigate the impact of the Nuss procedure on the thoracic spinal curvature in patients with PE. METHODS: A total of 100 patients with PE who underwent the Nuss procedure were included in the study and evaluated retrospectively. -

RIN2 Deficiency Results in Macrocephaly, Alopecia, Cutis Laxa
REPORT RIN2 Deficiency Results in Macrocephaly, Alopecia, Cutis Laxa, and Scoliosis: MACS Syndrome Lina Basel-Vanagaite,1,2,14 Ofer Sarig,4,14 Dov Hershkovitz,6,7 Dana Fuchs-Telem,2,4 Debora Rapaport,3 Andrea Gat,5 Gila Isman,4 Idit Shirazi,4 Mordechai Shohat,1,2 Claes D. Enk,10 Efrat Birk,2 Ju¨rgen Kohlhase,11 Uta Matysiak-Scholze,11 Idit Maya,1 Carlos Knopf,9 Anette Peffekoven,12 Hans-Christian Hennies,12 Reuven Bergman,8 Mia Horowitz,3 Akemi Ishida-Yamamoto,13 and Eli Sprecher2,4,6,* Inherited disorders of elastic tissue represent a complex and heterogeneous group of diseases, characterized often by sagging skin and occasionally by life-threatening visceral complications. In the present study, we report on an autosomal-recessive disorder that we have termed MACS syndrome (macrocephaly, alopecia, cutis laxa, and scoliosis). The disorder was mapped to chromosome 20p11.21-p11.23, and a homozygous frameshift mutation in RIN2 was found to segregate with the disease phenotype in a large consan- guineous kindred. The mutation identified results in decreased expression of RIN2, a ubiquitously expressed protein that interacts with Rab5 and is involved in the regulation of endocytic trafficking. RIN2 deficiency was found to be associated with paucity of dermal micro- fibrils and deficiency of fibulin-5, which may underlie the abnormal skin phenotype displayed by the patients. Disorders of elastic tissue often share common phenotypic shown to result in decreased secretion of elastin.9,10 In features, including redundant skin, hyperlaxity of joints, addition, -

Reduction of High-Grade Isthmic and Dysplastic Spondylolisthesis in 5 Adolescents Baron S
A Case Series & Literature Review Reduction of High-Grade Isthmic and Dysplastic Spondylolisthesis in 5 Adolescents Baron S. Lonner, MD, Edward W. Song, MD, Carrie L. Scharf, BA, and Jeff Yao, MD translation of L5 on S1. Isthmic spondylolisthesis (type Abstract II) may be caused by stress fracture from repetitive Treatment of high-grade isthmic and dysplastic spondylo- listhesis in children and adolescents remains a challenge. microtrauma to the pars interarticularis or by acute pars Surgical treatment of spondylolisthesis has been recom- interarticularis fracture, most commonly of the fifth 1 mended in adolescents with pain refractory to nonopera- lumbar vertebra. tive modalities, slippage progression, or >50% slippage on Surgical treatment of spondylolisthesis has been rec- presentation. Controversy exists as to the optimal surgical ommended in adolescents with pain refractory to non- approach for high-grade spondylolisthesis. In this report, operative modalities, slippage progression, or slippage we describe 5 cases of high-grade isthmic and dysplastic of >50% on presentation (Meyerding grade 3 or 4).2 spondylolisthesis in adolescents and review the literature on High-grade slips can be treated with various surgical surgical treatment for this entity. Operative records, charts, procedures, including decompression and circumfer- x-rays, and Scoliosis Research Society outcome question- ential arthrodesis with interbody grafting or transver- naires (SRS-22) were retrospectively evaluated for 5 con- tebral fibular grafting.3-9 Gaines10 recommended L5 secutive patients diagnosed with and treated for high-grade spondylolisthesis. Each patient received treatment consist- vertebrectomy with circumferential fusion of L4 to the ing of decompression, reduction, and circumferential fusion sacrum for spondyloptosis. -
A Genomic Approach to Delineating the Occurrence of Scoliosis in Arthrogryposis Multiplex Congenita
G C A T T A C G G C A T genes Article A Genomic Approach to Delineating the Occurrence of Scoliosis in Arthrogryposis Multiplex Congenita Xenia Latypova 1, Stefan Giovanni Creadore 2, Noémi Dahan-Oliel 3,4, Anxhela Gjyshi Gustafson 2, Steven Wei-Hung Hwang 5, Tanya Bedard 6, Kamran Shazand 2, Harold J. P. van Bosse 5 , Philip F. Giampietro 7,* and Klaus Dieterich 8,* 1 Grenoble Institut Neurosciences, Université Grenoble Alpes, Inserm, U1216, CHU Grenoble Alpes, 38000 Grenoble, France; [email protected] 2 Shriners Hospitals for Children Headquarters, Tampa, FL 33607, USA; [email protected] (S.G.C.); [email protected] (A.G.G.); [email protected] (K.S.) 3 Shriners Hospitals for Children, Montreal, QC H4A 0A9, Canada; [email protected] 4 School of Physical & Occupational Therapy, Faculty of Medicine and Health Sciences, McGill University, Montreal, QC H3G 2M1, Canada 5 Shriners Hospitals for Children, Philadelphia, PA 19140, USA; [email protected] (S.W.-H.H.); [email protected] (H.J.P.v.B.) 6 Alberta Congenital Anomalies Surveillance System, Alberta Health Services, Edmonton, AB T5J 3E4, Canada; [email protected] 7 Department of Pediatrics, University of Illinois-Chicago, Chicago, IL 60607, USA 8 Institut of Advanced Biosciences, Université Grenoble Alpes, Inserm, U1209, CHU Grenoble Alpes, 38000 Grenoble, France * Correspondence: [email protected] (P.F.G.); [email protected] (K.D.) Citation: Latypova, X.; Creadore, S.G.; Dahan-Oliel, N.; Gustafson, Abstract: Arthrogryposis multiplex congenita (AMC) describes a group of conditions characterized A.G.; Wei-Hung Hwang, S.; Bedard, by the presence of non-progressive congenital contractures in multiple body areas.