A Network Meta-Analysis Comparing Exenatide Once Weekly with Other GLP-1 Receptor Agonists for the Treatment of Type 2 Diabetes Mellitus
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Exenatide QW: a New Treatment Option for Type 2 Diabetes Offering Ease of Use, Improved Efficacy, and Reduced Side Effects
FEATURE ARTICLE Commentary: Exenatide QW: A New Treatment Option for Type 2 Diabetes Offering Ease of Use, Improved Efficacy, and Reduced Side Effects Charles F. Shaefer, Jr., MD Editor’s note: Once-weekly exenatide, (also called incretin mimetics) cur- with GLP-1 receptor agonists is the which has recently been approved for rently in use.3,4 only form of anti-diabetes therapy patients with type 2 diabetes, has great Validation of the acceptance offering proven weight loss. Finally, potential as a new diabetes therapy in clinical practice of GLP-1 GLP-1 receptor agonist therapy is in the primary care setting. This receptor agonists can be found in one of the recommended treatment commentary and the feature article that the recently released American strategies offering a low incidence of follows it (p. 95) offer an overview of Diabetes Association (ADA)/ hypoglycemia, an important aspect this new therapeutic tool and important European Association for the Study of diabetes therapy learned from the insights about its clinical utility. In the of Diabetes (EASD) position state- Action to Control Cardiovascular interest of transparency, however, we ment on the management of type 2 Risk in Diabetes trial.6 want to point out that the authors of diabetes, which placed these drugs As clinicians consider what to do both articles are affiliated with Amylin alongside older, well-accepted agents when metformin and lifestyle change Pharmaceuticals, which manufactures such as sulfonylureas (SUs) and do not adequately control a patient’s exenatide QW and markets it under the thiozolidinediones (TZDs) as a sec- A1C, they frequently ask, “incretin 5 trade name Bydureon. -

GLP-1 Receptor Agonists
Cognitive Vitality Reports® are reports written by neuroscientists at the Alzheimer’s Drug Discovery Foundation (ADDF). These scientific reports include analysis of drugs, drugs-in- development, drug targets, supplements, nutraceuticals, food/drink, non-pharmacologic interventions, and risk factors. Neuroscientists evaluate the potential benefit (or harm) for brain health, as well as for age-related health concerns that can affect brain health (e.g., cardiovascular diseases, cancers, diabetes/metabolic syndrome). In addition, these reports include evaluation of safety data, from clinical trials if available, and from preclinical models. GLP-1 Receptor Agonists Evidence Summary GLP-1 agonists are beneficial for patients with type 2 diabetes and obesity. Some evidence suggests benefits for Alzheimer’s disease. It is unclear whether it is beneficial for individuals without underlying metabolic disease. Semaglutide seems to be most effective for metabolic dysfunction, though liraglutide has more preclinical data for Alzheimer’s disease. Neuroprotective Benefit: Evidence from many preclinical studies and a pilot biomarker study suggest some neuroprotective benefits with GLP-1 agonists. However, whether they may be beneficial for everyone or only a subset of individuals (e.g. diabetics) is unclear. Aging and related health concerns: GLP-1 agonists are beneficial for treating diabetes and cardiovascular complications relating to diabetes. It is not clear whether they have beneficial effects in otherwise healthy individuals. Safety: GLP-1 agonists are generally safe for most people with minor side effects. However, long-term side effects are not known. 1 Availability: Available Dose: Varies - see Chemical formula: C172H265N43O51 (Liraglutide) as a prescription chart at the end of MW: 3751.262 g/mol medicine. -

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -

Combining a Glucagon-Like Peptide-1 Receptor Agonist with Basal Insulin: the Why and How
Combining a Glucagon-like Peptide-1 Receptor Agonist with Basal Insulin: The Why and How Case Study Mary is a 61 year-old female diagnosed with type 2 diabetes mellitus (T2DM) 8 years ago. She was initially managed with the combination of lifestyle modification and metformin. Since that time she was treated with a sulfonylurea, but it was discontinued due to symptomatic hypoglycemia. She was also treated with pioglitazone, but significant fluid retention led to it discontinuation. A year-and-a- half ago, basal insulin was added to her lifestyle and metformin management. She now administers 52 units (0.62 units/kg) once daily at bedtime. Since starting basal insulin, she has experienced 3 episodes of mild hypoglycemia. Since her diagnosis, Mary’s HbA1c has never been <7.0%; her current HbA1c is 7.9%. Over the past month, her fasting plasma glucose (FPG) has ranged from 103 mg/dL to 136 mg/dL and her postprandial glucose (PPG) from 164 mg/dL to 213 mg/dL. She has gained 2.6 kg since starting basal insulin and her body mass index is now 31 kg/m2. Her blood pressure is 134/82 mmHg. She experiences occasional tingling in her feet. Eye examination reveals grade 1 retinopathy. Current medications are: metformin 1000mg twice daily, basal insulin 52 units once daily at bedtime, and hydrochlorothiazide 25 mg once daily. Her family physician notes that Mary’s FPG is reasonably well-controlled, yet her HbA1c and PPG remain elevated. He is also concerned about her episodes of hypoglycemia and weight gain and the evidence indicating microvascular damage. -

Predicting Immunogenicity of Peptide Drugs and Their Impurities
Predicting Immunogenicity of Peptide Drugs and their Impurities using in Silico tools: Taspoglutide Case Study Aimee Mattei MS1, Frances Terry MPH1, Brian J Roberts PhD1, William Martin1, and Anne S De Groot MD1,2 1EpiVax, Inc.; 2Professor (Research) and Director, Institute for Immunology and Informatics, University of Rhode Island, USA Abstract What-if-Machine (WhIM) 15 Example Risk Profile for RLD A : . The peptide drug market is expected to generate $50B in revenue by 2024 but the FDA is Random Mimics the process of synthesizing High H ig h concerned about the number of impurities that may be introduced in the synthetic process. polypeptides and records theoretical Low 10 product impurities created through known . The peptide manufacturing process can result in synthesis-related impurities that can introduce Example Risk Profile for failures in the synthesis process. Random Peptides immunogenic epitopes within the amino acid sequence of the peptide, resulting in an unexpected 5 and undesired immune response against the drug. Each identified impurity is scored for Example Risk Profile for RLD B : putative T cell epitope content (EpiMatrix) Low 0 . EpiMatrix can be used to screen both the drug API sequence and its known peptide-related and cross conservation with the human Impurity Risk Score Risk Impurity impurities for the presence of putative T cell epitope content. proteome (JanusMatrix). -5 . When peptide-related impurities are unknown, the “What if Machine” (WhIM) can perform Impurities are weighted based on assumed probability of occurrence. Graphic for illustrative purposes only theoretical changes to the natural amino acid sequence of the drug substance and measure their -1 0 impact on the putative epitope content of the peptide. -

Exenatide: Role in Management of Type 2 Diabetes and Associated Cardiovascular Risk Factors
Therapy in Practice Exenatide: role in management of Type 2 diabetes and associated cardiovascular risk factors Zin Z Htike1, Kamlesh Khunti2 & Melanie Davies* Practice Points Obesity in Type 2 diabetes poses a challenge in choosing the right combination of glucose-lowering agents, particularly due to the potential side effect of weight gain with many of the existing glucose-lowering medications. One of the incretin-based therapies, the glucagon-like peptide-1 analog, exenatide, is found to be a promising new agent that not only provides glucoregulatory effect in improving glycemic control without increase risk of hypoglycemia but also often results in weight loss. Treatment with exenatide results in reduction in HbA1c comparable to many of the existing glucose-lowering agents including basal insulin analog, galrgine or biphasic insulin aspart. Exenatide is of particular benefit in obese patients with Type 2 diabetes whose control in inadequate on a combination of oral glucose-lowering agents. To date, exenatide is not licensed for use in combination with insulin. SUMMARY Management of Type 2 diabetes, particularly in obese patients, is rather challenging as treatment with the majority of the available glucose-lowering t herapies is often associated with side effects of weight gain and hypoglycemia, in addition to failure to maintain durable glycemic control. The first available glucagon-like peptide-1 analog, exenatide, adds a new t herapeutic option to the currently available glucose-lowering agents for obese patients with Type 2 d iabetes. Both randomized controlled trials and retrospective observational s tudies have shown that treatment with exenatide not only improves glycemic control with a low risk of h ypoglycemia, but also results in concurrent weight loss with the additional benefit of i mprovement in cardiovascular risk factors of hypertension and hyperlipidemia. -

Membrane-Tethered Ligands Are Effective Probes for Exploring Class B1 G Protein-Coupled Receptor Function
Membrane-tethered ligands are effective probes for exploring class B1 G protein-coupled receptor function Jean-Philippe Fortina, Yuantee Zhua, Charles Choib, Martin Beinborna, Michael N. Nitabachb, and Alan S. Kopina,1 aMolecular Pharmacology Research Center, Molecular Cardiology Research Institute, Tufts Medical Center, Tufts University School of Medicine, Boston, MA 02111; and bDepartment of Cellular and Molecular Physiology, Yale School of Medicine, New Haven, CT 06520 Edited by Solomon H. Snyder, Johns Hopkins University School of Medicine, Baltimore, MD, and approved March 6, 2009 (received for review January 6, 2009) Class B1 (secretin family) G protein-coupled receptors (GPCRs) peptide hormone complexes, providing important insight into modulate a wide range of physiological functions, including glu- the molecular mechanisms underlying PTH (3), corticotropin- cose homeostasis, feeding behavior, fat deposition, bone remod- releasing factor (CRF) (4), GIP (5), and exendin-4 (EXE4) (6) eling, and vascular contractility. Endogenous peptide ligands for interaction with their corresponding GPCRs. Notably, these these GPCRs are of intermediate length (27–44 aa) and include reports highlight that each of the peptides docks as an amphipathic receptor affinity (C-terminal) as well as receptor activation (N- ␣-helix in a hydrophobic groove present in the receptor ECD. terminal) domains. We have developed a technology in which a Peptide ligands that modulate class B1 GPCR function hold peptide ligand tethered to the cell membrane selectively modu- considerable promise as therapeutics. The peptidic GLP-1 mi- lates corresponding class B1 GPCR-mediated signaling. The engi- metic EXE4 (also known as exenatide or BYETTA) activates the neered cDNA constructs encode a single protein composed of (i)a GLP-1 receptor (GLP-1R) and represents the first incretin- transmembrane domain (TMD) with an intracellular C terminus, (ii) based pharmaceutical for the treatment of type 2 diabetes (7). -
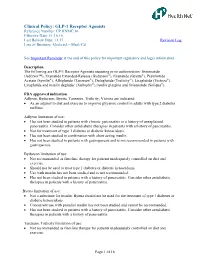
GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal
Clinical Policy: GLP-1 Receptor Agonists Reference Number: CP.HNMC.16 Effective Date: 11.16.16 Last Review Date: 11.17 Revision Log Line of Business: Medicaid – Medi-Cal See Important Reminder at the end of this policy for important regulatory and legal information. Description The following are GLP-1 Receptor Agonists requiring prior authorization: lixisenatide (Adlyxin™), Exenatide Extended-Release (Bydureon®), Exenatide (Byetta®), Pramlintide Acetate (Symlin®), Albiglutide (Tanzeum®), Dulaglutide (Trulicity®), Liraglutide (Victoza®), Liraglutide and insulin degludec (Xultophy®),Insulin glargine and lixisenatide (Soliqua®). FDA approved indication Adlyxin, Bydureon, Byetta, Tanzeum, Trulicity, Victoza are indicated: As an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Adlyxin limitation of use: Has not been studied in patients with chronic pancreatitis or a history of unexplained pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Not for treatment of type 1 diabetes or diabetic ketoacidosis. Has not been studied in combination with short acting insulin. Has not been studied in patients with gastroparesis and is not recommended in patients with gastroparesis. Bydureon limitation of use: Not recommended as first-line therapy for patients inadequately controlled on diet and exercise. Should not be used to treat type 1 diabetes or diabetic ketoacidosis. Use with insulin has not been studied and is not recommended. Has not been studied in patients with a history of pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis. Byetta limitation of use: Not a substitute for insulin. Byetta should not be used for the treatment of type 1 diabetes or diabetic ketoacidosis. -

Glucagon-Like Peptide-1 and Its Class BG Protein–Coupled Receptors
1521-0081/68/4/954–1013$25.00 http://dx.doi.org/10.1124/pr.115.011395 PHARMACOLOGICAL REVIEWS Pharmacol Rev 68:954–1013, October 2016 Copyright © 2016 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: RICHARD DEQUAN YE Glucagon-Like Peptide-1 and Its Class B G Protein–Coupled Receptors: A Long March to Therapeutic Successes Chris de Graaf, Dan Donnelly, Denise Wootten, Jesper Lau, Patrick M. Sexton, Laurence J. Miller, Jung-Mo Ahn, Jiayu Liao, Madeleine M. Fletcher, Dehua Yang, Alastair J. H. Brown, Caihong Zhou, Jiejie Deng, and Ming-Wei Wang Division of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands (C.d.G.); School of Biomedical Sciences, University of Leeds, Leeds, United Kingdom (D.D.); Drug Discovery Biology Theme and Department of Pharmacology, Monash Institute of Pharmaceutical Sciences, Parkville, Victoria, Australia (D.W., P.M.S., M.M.F.); Protein and Peptide Chemistry, Global Research, Novo Nordisk A/S, Måløv, Denmark (J.La.); Department of Molecular Pharmacology and Experimental Therapeutics, Mayo Clinic, Scottsdale, Arizona (L.J.M.); Department of Chemistry and Biochemistry, University of Texas at Dallas, Richardson, Texas (J.-M.A.); Department of Bioengineering, Bourns College of Engineering, University of California at Riverside, Riverside, California (J.Li.); National Center for Drug Screening and CAS Key Laboratory of Receptor Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai, China (D.Y., C.Z., J.D., M.-W.W.); Heptares Therapeutics, BioPark, Welwyn Garden City, United Kingdom (A.J.H.B.); and School of Pharmacy, Fudan University, Zhangjiang High-Tech Park, Shanghai, China (M.-W.W.) Downloaded from Abstract. -

(Hmmc) Dulaglutide (Trulicity
HERTFORDSHIRE MEDICINES MANAGEMENT COMMITTEE (HMMC) DULAGLUTIDE (TRULICITY®) FOR TYPE 2 DIABETES MELLITUS RECOMMENDED FOR RESTRICTED USE Name: What it is Indication Date Decision Decision NICE / SMC generic last revised Status Guidance (trade) dulaglutide glucagon‑like Type 2 diabetes June 2016 Final NICE - none ® (Trulicity ) peptide‑1 mellitus (T2DM) SMC – approved (GLP‑1) receptor for restricted use agonist Dulaglutide (Trulicity®) is RECOMMENDED FOR RESTRICTED USE as a GLP-1 receptor agonist option when a GLP-1 receptor agonist is indicated as add-on therapy in line with NICE guidelines for type 2 diabetes (see Policy Drivers overleaf) if a specialist service switches a patient from an alternative GLP-1 receptor agonist to dulaglutide clear information should be supplied on rationale and switch process to primary care colleagues. EFFICACY SAFETY From AWARD studies for change in HbA1c from According to SPC most common adverse events baseline, weekly dulaglutide was demonstrated to be: (≥1/10) are hypoglycaemia, particularly in o (1.5mg or 0.75mg) superior to placebo and exenatide combination with a sulfonylurea or insulin, and twice daily at 26 weeks gastrointestinal (GI) disorders. o (1.5mg or 0.75mg) superior to sitagliptin at 52 weeks According to the EPAR: o 1.5mg non-inferior to liraglutide 1.8mg daily at o across the phase II and III integrated safety 26 weeks population, incidence of common events are o (1.5mg or 0.75mg) non-inferior to insulin glargine at consistent with other GLP‑1 receptor agonists. 52 weeks. Superiority demonstrated for 1.5mg dose. o long‑term safety concerns of pancreatitis and Open label design of some of the AWARD studies pancreatic and thyroid cancers are consistent may have biased results with other GLP‑1 receptor agonists. -

Changing Lives with Next Generation Peptide Therapeutics
Changing lives with next generation peptide therapeutics Zealand Pharma Corporate Presentation May 2019 Forward-looking statements This presentation contains information pertaining to Zealand Pharma A/S (“Zealand"). Neither Zealand nor its management, directors, employees or representatives make any representation or warranty, express or implied, as to the accuracy or completeness of any of the information contained in this presentation or any other information transmitted or made available to the viewer or recipient hereof, whether communicated in written or oral form. This presentation does not constitute or form part of, and should not be construed as, an offer to sell or issue or the solicitation of an offer to buy or acquire Zealand securities, in any jurisdiction, or an inducement to enter into investment activity, nor shall there be any sale of Zealand securities in any state or jurisdiction in which such offer, solicitation or sale would be unlawful prior to registration or qualification under the securities laws of any such state or jurisdiction. No part of this presentation, nor the fact of its distribution, should form the basis of, or be relied on in connection with, any contract or commitment or investment decision whatsoever. This presentation contains forward-looking statements that reflect management's current views with respect to Zealand's product candidates' development, clinical and regulatory timelines and anticipated results, market opportunity, potential financial performance and other statements of future events or conditions. Although Zealand believes that the expectations reflected in such forward-looking statements are reasonable, no assurance can be given that such expectations will prove to have been correct. -

Effects of Sustained Treatment with Lixisenatide On
EMERGING THERAPIES: DRUGS AND REGIMENS Diabetes Care 1 Christopher K. Rayner,1,2 Linda E. Watson,1 Effects of Sustained Treatment Liza K. Phillips,1,3 Kylie Lange,1 Michelle J. Bound,1 Jacqueline Grivell,1 With Lixisenatide on Gastric Tongzhi Wu,1,3 Karen L. Jones,1,3 Michael Horowitz,1,3 Ele Ferrannini,4 Emptying and Postprandial Domenico Trico,` 5 Silvia Frascerra,6 Glucose Metabolism in Type 2 Andrea Mari,7 and Andrea Natali6 Diabetes: A Randomized Controlled Trial https://doi.org/10.2337/dc20-0190 OBJECTIVE Tachyphylaxis for slowing of gastric emptying is seen with continuous exposure to glucagon-like peptide 1 (GLP-1). We therefore aimed to establish whether prolonged use of a “short-acting” GLP-1 receptor agonist, lixisenatide, achieves sustained slowing of gastric emptying and reduction in postprandial glycemia. RESEARCH DESIGN AND METHODS 1Centre of Research Excellence for Translating A total of 30 patients with metformin-treated type 2 diabetes underwent assessment Nutritional Science to Good Health, University of Adelaide, Adelaide, Australia of gastric emptying (scintigraphy) and glucose metabolism (dual tracer technique) 2Department of Gastroenterology and Hepatol- aftera75-gglucosedrink,beforeandafter8weeks’treatmentwithlixisenatide(20mg ogy, Royal Adelaide Hospital, Adelaide, Australia subcutaneously daily) or placebo, in a double-blind randomized parallel design. 3Endocrine and Metabolic Unit, Royal Adelaide Hospital, Adelaide, Australia RESULTS 4CNR Institute of Clinical Physiology, Pisa, Italy 5Department of Surgical,