Brand Name: Bydureon Generic Name: Exenatide Extended-Release
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Exenatide QW: a New Treatment Option for Type 2 Diabetes Offering Ease of Use, Improved Efficacy, and Reduced Side Effects
FEATURE ARTICLE Commentary: Exenatide QW: A New Treatment Option for Type 2 Diabetes Offering Ease of Use, Improved Efficacy, and Reduced Side Effects Charles F. Shaefer, Jr., MD Editor’s note: Once-weekly exenatide, (also called incretin mimetics) cur- with GLP-1 receptor agonists is the which has recently been approved for rently in use.3,4 only form of anti-diabetes therapy patients with type 2 diabetes, has great Validation of the acceptance offering proven weight loss. Finally, potential as a new diabetes therapy in clinical practice of GLP-1 GLP-1 receptor agonist therapy is in the primary care setting. This receptor agonists can be found in one of the recommended treatment commentary and the feature article that the recently released American strategies offering a low incidence of follows it (p. 95) offer an overview of Diabetes Association (ADA)/ hypoglycemia, an important aspect this new therapeutic tool and important European Association for the Study of diabetes therapy learned from the insights about its clinical utility. In the of Diabetes (EASD) position state- Action to Control Cardiovascular interest of transparency, however, we ment on the management of type 2 Risk in Diabetes trial.6 want to point out that the authors of diabetes, which placed these drugs As clinicians consider what to do both articles are affiliated with Amylin alongside older, well-accepted agents when metformin and lifestyle change Pharmaceuticals, which manufactures such as sulfonylureas (SUs) and do not adequately control a patient’s exenatide QW and markets it under the thiozolidinediones (TZDs) as a sec- A1C, they frequently ask, “incretin 5 trade name Bydureon. -

GLP-1 Receptor Agonists
Cognitive Vitality Reports® are reports written by neuroscientists at the Alzheimer’s Drug Discovery Foundation (ADDF). These scientific reports include analysis of drugs, drugs-in- development, drug targets, supplements, nutraceuticals, food/drink, non-pharmacologic interventions, and risk factors. Neuroscientists evaluate the potential benefit (or harm) for brain health, as well as for age-related health concerns that can affect brain health (e.g., cardiovascular diseases, cancers, diabetes/metabolic syndrome). In addition, these reports include evaluation of safety data, from clinical trials if available, and from preclinical models. GLP-1 Receptor Agonists Evidence Summary GLP-1 agonists are beneficial for patients with type 2 diabetes and obesity. Some evidence suggests benefits for Alzheimer’s disease. It is unclear whether it is beneficial for individuals without underlying metabolic disease. Semaglutide seems to be most effective for metabolic dysfunction, though liraglutide has more preclinical data for Alzheimer’s disease. Neuroprotective Benefit: Evidence from many preclinical studies and a pilot biomarker study suggest some neuroprotective benefits with GLP-1 agonists. However, whether they may be beneficial for everyone or only a subset of individuals (e.g. diabetics) is unclear. Aging and related health concerns: GLP-1 agonists are beneficial for treating diabetes and cardiovascular complications relating to diabetes. It is not clear whether they have beneficial effects in otherwise healthy individuals. Safety: GLP-1 agonists are generally safe for most people with minor side effects. However, long-term side effects are not known. 1 Availability: Available Dose: Varies - see Chemical formula: C172H265N43O51 (Liraglutide) as a prescription chart at the end of MW: 3751.262 g/mol medicine. -

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -
![LANTUS® (Insulin Glargine [Rdna Origin] Injection)](https://docslib.b-cdn.net/cover/0369/lantus%C2%AE-insulin-glargine-rdna-origin-injection-60369.webp)
LANTUS® (Insulin Glargine [Rdna Origin] Injection)
Rev. March 2007 Rx Only LANTUS® (insulin glargine [rDNA origin] injection) LANTUS® must NOT be diluted or mixed with any other insulin or solution. DESCRIPTION LANTUS® (insulin glargine [rDNA origin] injection) is a sterile solution of insulin glargine for use as an injection. Insulin glargine is a recombinant human insulin analog that is a long-acting (up to 24-hour duration of action), parenteral blood-glucose-lowering agent. (See CLINICAL PHARMACOLOGY). LANTUS is produced by recombinant DNA technology utilizing a non- pathogenic laboratory strain of Escherichia coli (K12) as the production organism. Insulin glargine differs from human insulin in that the amino acid asparagine at position A21 is replaced by glycine and two arginines are added to the C-terminus of the B-chain. Chemically, it is 21A- B B Gly-30 a-L-Arg-30 b-L-Arg-human insulin and has the empirical formula C267H404N72O78S6 and a molecular weight of 6063. It has the following structural formula: LANTUS consists of insulin glargine dissolved in a clear aqueous fluid. Each milliliter of LANTUS (insulin glargine injection) contains 100 IU (3.6378 mg) insulin glargine. Inactive ingredients for the 10 mL vial are 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, 20 mcg polysorbate 20, and water for injection. Inactive ingredients for the 3 mL cartridge are 30 mcg zinc, 2.7 mg m-cresol, 20 mg glycerol 85%, and water for injection. The pH is adjusted by addition of aqueous solutions of hydrochloric acid and sodium hydroxide. LANTUS has a pH of approximately 4. CLINICAL PHARMACOLOGY Mechanism of Action: The primary activity of insulin, including insulin glargine, is regulation of glucose metabolism. -

Insulin Aspart Sanofi, If It Is Coloured Or It Has Solid Pieces in It
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 This medicinal product is subject to additional monitoring. This will allow quick identification of new safety information. Healthcare professionals are asked to report any suspected adverse reactions. See section 4.8 for how to report adverse reactions. 1. NAME OF THE MEDICINAL PRODUCT Insulin aspart Sanofi 100 units/ml solution for injection in vial Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen 2. QUALITATIVE AND QUANTITATIVE COMPOSITION One ml solution contains 100 units insulin aspart* (equivalent to 3.5 mg). Insulin aspart Sanofi 100 units/ml solution for injection in vial Each vial contains 10 ml equivalent to 1,000 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in cartridge Each cartridge contains 3 ml equivalent to 300 units insulin aspart. Insulin aspart Sanofi 100 units/ml solution for injection in pre-filled pen Each pre-filled pen contains 3 ml equivalent to 300 units insulin aspart. Each pre-filled pen delivers 1-80 units in steps of 1 unit. *produced in Escherichia coli by recombinant DNA technology. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Solution for injection (injection). Clear, colourless, aqueous solution. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Insulin aspart Sanofi is indicated for the treatment of diabetes mellitus in adults, adolescents and children aged 1 year and above. 4.2 Posology and method of administration Posology The potency of insulin analogues, including insulin aspart, is expressed in units, whereas the potency of human insulin is expressed in international units. -

Combining a Glucagon-Like Peptide-1 Receptor Agonist with Basal Insulin: the Why and How
Combining a Glucagon-like Peptide-1 Receptor Agonist with Basal Insulin: The Why and How Case Study Mary is a 61 year-old female diagnosed with type 2 diabetes mellitus (T2DM) 8 years ago. She was initially managed with the combination of lifestyle modification and metformin. Since that time she was treated with a sulfonylurea, but it was discontinued due to symptomatic hypoglycemia. She was also treated with pioglitazone, but significant fluid retention led to it discontinuation. A year-and-a- half ago, basal insulin was added to her lifestyle and metformin management. She now administers 52 units (0.62 units/kg) once daily at bedtime. Since starting basal insulin, she has experienced 3 episodes of mild hypoglycemia. Since her diagnosis, Mary’s HbA1c has never been <7.0%; her current HbA1c is 7.9%. Over the past month, her fasting plasma glucose (FPG) has ranged from 103 mg/dL to 136 mg/dL and her postprandial glucose (PPG) from 164 mg/dL to 213 mg/dL. She has gained 2.6 kg since starting basal insulin and her body mass index is now 31 kg/m2. Her blood pressure is 134/82 mmHg. She experiences occasional tingling in her feet. Eye examination reveals grade 1 retinopathy. Current medications are: metformin 1000mg twice daily, basal insulin 52 units once daily at bedtime, and hydrochlorothiazide 25 mg once daily. Her family physician notes that Mary’s FPG is reasonably well-controlled, yet her HbA1c and PPG remain elevated. He is also concerned about her episodes of hypoglycemia and weight gain and the evidence indicating microvascular damage. -

Predicting Immunogenicity of Peptide Drugs and Their Impurities
Predicting Immunogenicity of Peptide Drugs and their Impurities using in Silico tools: Taspoglutide Case Study Aimee Mattei MS1, Frances Terry MPH1, Brian J Roberts PhD1, William Martin1, and Anne S De Groot MD1,2 1EpiVax, Inc.; 2Professor (Research) and Director, Institute for Immunology and Informatics, University of Rhode Island, USA Abstract What-if-Machine (WhIM) 15 Example Risk Profile for RLD A : . The peptide drug market is expected to generate $50B in revenue by 2024 but the FDA is Random Mimics the process of synthesizing High H ig h concerned about the number of impurities that may be introduced in the synthetic process. polypeptides and records theoretical Low 10 product impurities created through known . The peptide manufacturing process can result in synthesis-related impurities that can introduce Example Risk Profile for failures in the synthesis process. Random Peptides immunogenic epitopes within the amino acid sequence of the peptide, resulting in an unexpected 5 and undesired immune response against the drug. Each identified impurity is scored for Example Risk Profile for RLD B : putative T cell epitope content (EpiMatrix) Low 0 . EpiMatrix can be used to screen both the drug API sequence and its known peptide-related and cross conservation with the human Impurity Risk Score Risk Impurity impurities for the presence of putative T cell epitope content. proteome (JanusMatrix). -5 . When peptide-related impurities are unknown, the “What if Machine” (WhIM) can perform Impurities are weighted based on assumed probability of occurrence. Graphic for illustrative purposes only theoretical changes to the natural amino acid sequence of the drug substance and measure their -1 0 impact on the putative epitope content of the peptide. -

OZEMPIC (Semaglutide) Injection, for Subcutaneous Use Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙CONTRAINDICATIONS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ These highlights do not include all the information needed to use Personal or family history of medullary thyroid carcinoma or in patients OZEMPIC® safely and effectively. See full prescribing information with Multiple Endocrine Neoplasia syndrome type 2 (4). for OZEMPIC. Known hypersensitivity to OZEMPIC or any of the product components (4). OZEMPIC (semaglutide) injection, for subcutaneous use Initial U.S. Approval: 2017 ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙WARNINGS AND PRECAUTIONS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ Pancreatitis: Has been reported in clinical trials. Discontinue promptly if WARNING: RISK OF THYROID C-CELL TUMORS pancreatitis is suspected. Do not restart if pancreatitis is confirmed (5.2). See full prescribing information for complete boxed warning. Diabetic Retinopathy Complications: Has been reported in a clinical trial. Patients with a history of diabetic retinopathy should be monitored (5.3). In rodents, semaglutide causes thyroid C-cell tumors. It is Never share an OZEMPIC pen between patients, even if the needle is unknown whether OZEMPIC causes thyroid C-cell tumors, changed (5.4). including medullary thyroid carcinoma (MTC), in humans as Hypoglycemia: When OZEMPIC is used with an insulin secretagogue or the human relevance of semaglutide-induced rodent thyroid C- insulin, consider lowering the dose of the secretagogue or insulin to reduce cell tumors has not been determined (5.1, 13.1). the risk of hypoglycemia (5.5). OZEMPIC is contraindicated in patients with a personal or Acute Kidney Injury: Monitor renal function in patients with renal family history of MTC or in patients with Multiple Endocrine impairment reporting severe adverse gastrointestinal reactions (5.6). Neoplasia syndrome type 2 (MEN 2). -

Exenatide: Role in Management of Type 2 Diabetes and Associated Cardiovascular Risk Factors
Therapy in Practice Exenatide: role in management of Type 2 diabetes and associated cardiovascular risk factors Zin Z Htike1, Kamlesh Khunti2 & Melanie Davies* Practice Points Obesity in Type 2 diabetes poses a challenge in choosing the right combination of glucose-lowering agents, particularly due to the potential side effect of weight gain with many of the existing glucose-lowering medications. One of the incretin-based therapies, the glucagon-like peptide-1 analog, exenatide, is found to be a promising new agent that not only provides glucoregulatory effect in improving glycemic control without increase risk of hypoglycemia but also often results in weight loss. Treatment with exenatide results in reduction in HbA1c comparable to many of the existing glucose-lowering agents including basal insulin analog, galrgine or biphasic insulin aspart. Exenatide is of particular benefit in obese patients with Type 2 diabetes whose control in inadequate on a combination of oral glucose-lowering agents. To date, exenatide is not licensed for use in combination with insulin. SUMMARY Management of Type 2 diabetes, particularly in obese patients, is rather challenging as treatment with the majority of the available glucose-lowering t herapies is often associated with side effects of weight gain and hypoglycemia, in addition to failure to maintain durable glycemic control. The first available glucagon-like peptide-1 analog, exenatide, adds a new t herapeutic option to the currently available glucose-lowering agents for obese patients with Type 2 d iabetes. Both randomized controlled trials and retrospective observational s tudies have shown that treatment with exenatide not only improves glycemic control with a low risk of h ypoglycemia, but also results in concurrent weight loss with the additional benefit of i mprovement in cardiovascular risk factors of hypertension and hyperlipidemia. -

A Network Meta-Analysis Comparing Exenatide Once Weekly with Other GLP-1 Receptor Agonists for the Treatment of Type 2 Diabetes Mellitus
Diabetes Ther DOI 10.1007/s13300-016-0155-1 REVIEW A Network Meta-analysis Comparing Exenatide Once Weekly with Other GLP-1 Receptor Agonists for the Treatment of Type 2 Diabetes Mellitus Sheena Kayaniyil . Greta Lozano-Ortega . Heather A. Bennett . Kristina Johnsson . Alka Shaunik . Susan Grandy . Bernt Kartman To view enhanced content go to www.diabetestherapy-open.com Received: December 17, 2015 Ó The Author(s) 2016. This article is published with open access at Springerlink.com ABSTRACT treatment of adults with T2DM inadequately controlled on metformin monotherapy. Introduction: Exenatide is a glucagon-like Methods: A systematic literature review was peptide-1 receptor agonist (GLP-1 RA), conducted to identify randomized controlled approved for treatment of type 2 diabetes trials (RCTs) that investigated GLP-1 RAs mellitus (T2DM). There is limited direct (albiglutide, dulaglutide, exenatide, liraglutide, evidence comparing the efficacy and and lixisenatide) at approved doses in the tolerability of exenatide 2 mg once weekly United States/Europe, added on to metformin (QW) to other GLP-1 RAs. A network only and of 24 ± 6 weeks treatment duration. meta-analysis (NMA) was conducted to A Bayesian NMA was conducted. estimate the relative efficacy and tolerability of Results: Fourteen RCTs were included in the exenatide QW versus other GLP-1 RAs for the NMA. Exenatide QW obtained a statistically significant reduction in glycated hemoglobin (HbA1c) relative to lixisenatide 20 lg once daily. No other comparisons of exenatide QW Electronic supplementary material The online version of this article (doi:10.1007/s13300-016-0155-1) to other GLP-1 RAs were statistically significant contains supplementary material, which is available to for change in HbA1c. -
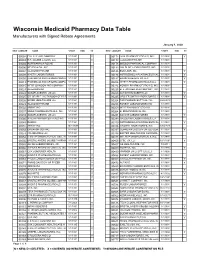
Numeric Listing of Manufacturers That Have Signed Rebate Agreements
Wisconsin Medicaid Pharmacy Data Table Manufacturers with Signed Rebate Agreements January 1, 2020 NEWLABELER NAME START END SC NEW LABELER NAME START END SC 00002 ELI LILLY AND COMPANY 1/1/1991 Y 00172 IVAX PHARMACEUTICALS, INC. 1/1/1991 Y 00003 E.R. SQUIBB & SONS, LLC. 1/1/1991 Y 00173 GLAXOSMITHKLINE 1/1/1991 00004 HOFFMANN-LA ROCHE 1/1/1991 00178 MISSION PHARMACAL COMPANY 1/1/1991 00006 MERCK & CO., INC. 1/1/1991 Y 00182 GOLDLINE LABORATORIES, INC. 1/1/1991 00007 GLAXOSMITHKLINE 1/1/1991 00185 EON LABS, INC. 1/1/1991 Y 00008 WYETH LABORATORIES 1/1/1991 Y 00186 ASTRAZENECA PHARMACEUTICAL 1/1/1991 Y 00009 PHARMACIA AND UPJOHN COMPA 1/1/1991 Y 00187 BAUSCH HEALTH US, LLC. 1/1/1991 Y 00013 PHARMACIA AND UPJOHN COMPA 1/1/1991 Y 00206 WYETH PHARMACEUTICALS LLC 1/1/1991 Y 00015 MEAD JOHNSON AND COMPANY 1/1/1991 Y 00224 KONSYL PHARMACEUTICALS, INC. 1/1/1992 00023 ALLERGAN INC 1/1/1991 00225 B. F. ASCHER AND COMPANY, INC. 1/1/1991 00024 SANOFI-AVENTIS, US LLC 1/1/1991 Y 00228 ACTAVIS ELIZABETH LLC 1/1/1991 Y 00025 GD. SEARLE LLC DIVISION OF PFIZ 1/1/1991 Y 00245 UPSHER-SMITH LABORATORIES, I 1/1/1991 Y 00026 BAYER HEALTHCARE LLC 1/1/1991 Y 00254 PAR PHARMACEUTTICAL INC. 9/28/2018 00029 GLAXOSMITHKLINE 1/1/1991 00258 FOREST LABORATORIES INC 1/1/1991 00032 ABBVIE INC. 1/1/1991 Y 00259 MERZ PHARMACEUTICALS 1/1/1991 00037 MEDA PHARMACEUTICALS, INC. -

Type 2 Diabetes Adult Outpatient Insulin Guidelines
Diabetes Coalition of California TYPE 2 DIABETES ADULT OUTPATIENT INSULIN GUIDELINES GENERAL RECOMMENDATIONS Start insulin if A1C and glucose levels are above goal despite optimal use of other diabetes 6,7,8 medications. (Consider insulin as initial therapy if A1C very high, such as > 10.0%) 6,7,8 Start with BASAL INSULIN for most patients 1,6 Consider the following goals ADA A1C Goals: A1C < 7.0 for most patients A1C > 7.0 (consider 7.0-7.9) for higher risk patients 1. History of severe hypoglycemia 2. Multiple co-morbid conditions 3. Long standing diabetes 4. Limited life expectancy 5. Advanced complications or 6. Difficult to control despite use of insulin ADA Glucose Goals*: Fasting and premeal glucose < 130 Peak post-meal glucose (1-2 hours after meal) < 180 Difference between premeal and post-meal glucose < 50 *for higher risk patients individualize glucose goals in order to avoid hypoglycemia BASAL INSULIN Intermediate-acting: NPH Note: NPH insulin has elevated risk of hypoglycemia so use with extra caution6,8,15,17,25,32 Long-acting: Glargine (Lantus®) Detemir (Levemir®) 6,7,8 Basal insulin is best starting insulin choice for most patients (if fasting glucose above goal). 6,7 8 Start one of the intermediate-acting or long-acting insulins listed above. Start insulin at night. When starting basal insulin: Continue secretagogues. Continue metformin. 7,8,20,29 Note: if NPH causes nocturnal hypoglycemia, consider switching NPH to long-acting insulin. 17,25,32 STARTING DOSE: Start dose: 10 units6,7,8,11,12,13,14,16,19,20,21,22,25 Consider using a lower starting dose (such as 0.1 units/kg/day32) especially if 17,19 patient is thin or has a fasting glucose only minimally above goal.