Thrombin Time for Assessment of Dabigatran (Pradaxa®) Clearance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Severity of Anaemia Has Corresponding Effects on Coagulation Parameters of Sickle Cell Disease Patients
diseases Article Severity of Anaemia Has Corresponding Effects on Coagulation Parameters of Sickle Cell Disease Patients Samuel Antwi-Baffour 1,* , Ransford Kyeremeh 1 and Lawrence Annison 2 1 Department of Medical Laboratory Sciences, School of Allied Health Sciences, College of Health Sciences, University of Ghana, P.O. Box KB 143 Accra, Ghana; [email protected] 2 Department of Medical Laboratory Sciences, School of Allied Health Sciences, Narh-Bita College, P.O. Box Co1061 Tema, Ghana; [email protected] * Correspondence: s.antwi-baff[email protected] Received: 31 July 2019; Accepted: 18 October 2019; Published: 17 December 2019 Abstract: Sickle cell disease (SCD) is an inherited condition characterized by chronic haemolytic anaemia. SCD is associated with moderate to severe anaemia, hypercoagulable state and inconsistent platelet count and function. However, studies have yielded conflicting results with regards to the effect of anaemia on coagulation in SCD. The purpose of this study was to determine the effect of anaemia severity on selected coagulation parameters of SCD patients. Four millilitres of venous blood samples were taken from the participants (SCD and non-SCD patients) and used for analysis of full blood count and coagulation parameters. Data was analysed using SPSS version-16. From the results, it was seen that individuals with SCD had a prolonged mean PT, APTT and high platelet count compared to the controls. There was also significant difference in the mean PT (p = 0.039), APTT (p = 0.041) and platelet count (p = 0.010) in HbSS participants with severe anaemia. Mean APTT also showed significant difference (p = 0.044) with severe anaemia in HbSC participants. -

Blood and Immunity
Chapter Ten BLOOD AND IMMUNITY Chapter Contents 10 Pretest Clinical Aspects of Immunity Blood Chapter Review Immunity Case Studies Word Parts Pertaining to Blood and Immunity Crossword Puzzle Clinical Aspects of Blood Objectives After study of this chapter you should be able to: 1. Describe the composition of the blood plasma. 7. Identify and use roots pertaining to blood 2. Describe and give the functions of the three types of chemistry. blood cells. 8. List and describe the major disorders of the blood. 3. Label pictures of the blood cells. 9. List and describe the major disorders of the 4. Explain the basis of blood types. immune system. 5. Define immunity and list the possible sources of 10. Describe the major tests used to study blood. immunity. 11. Interpret abbreviations used in blood studies. 6. Identify and use roots and suffixes pertaining to the 12. Analyse several case studies involving the blood. blood and immunity. Pretest 1. The scientific name for red blood cells 5. Substances produced by immune cells that is . counteract microorganisms and other foreign 2. The scientific name for white blood cells materials are called . is . 6. A deficiency of hemoglobin results in the disorder 3. Platelets, or thrombocytes, are involved in called . 7. A neoplasm involving overgrowth of white blood 4. The white blood cells active in adaptive immunity cells is called . are the . 225 226 ♦ PART THREE / Body Systems Other 1% Proteins 8% Plasma 55% Water 91% Whole blood Leukocytes and platelets Formed 0.9% elements 45% Erythrocytes 10 99.1% Figure 10-1 Composition of whole blood. -

Hemostasis and Thrombosis
PROCEDURES FOR HEMOSTASIS AND THROMBOSIS A Clinical Test Compendium PROCEDURES FOR HEMOSTASIS AND THROMBOSIS: A CLINICAL TEST COMPENDIUM Test No. Test Name Profile Includes Specimen Requirements Bleeding Profiles and Screening Tests 117199 aPTT Mixing Studies aPTT; aPTT 1:1 mix normal plasma (NP); aPTT 1:1 mix saline; aPTT 2 mL citrated plasma, frozen 1:1 mix, incubated; aPTT 1:1 mix NP, incubated control 116004 Abnormal Bleeding Profile PT; aPTT; thrombin time; platelet count 5 mL EDTA whole blood, one tube citrated whole blood (unopened), and 2 mL citrated plasma, frozen Minimum: 5 mL EDTA whole blood, one tube citrated whole blood (unopened), and 1 mL citrated plasma, frozen 503541 Bleeding Diathesis With Normal α2-Antiplasmin assay; euglobulin lysis time; factor VIII activity; 7 mL (1mL in each of 7 tubes) platelet-poor aPTT/PT Profile (Esoterix) factor VIII chromogenic; factor IX activity; factor XI activity; factor citrated plasma, frozen XIII activity; fibrinogen activity; PAI-1 activity with reflex to PAI-1 antigen and tPA; von Willebrand factor activity; von Willebrand factor antigen 336572 Menorrhagia Profile PT; aPTT; factor IX activity; factor VIII activity; factor XI activity; 3 mL citrated plasma, frozen von Willebrand factor activity; von Willebrand factor antigen Minimum: 2 mL citrated plasma, frozen 117866 Prolonged Protime Profile Factor II activity; factor V activity; factor VII activity; factor 3 mL citrated plasma, frozen X activity; fibrinogen activity; dilute prothrombin time Minimum: 2 mL citrated plasma, frozen -

Thrombophilia Testing Panel Now Available
Thrombophilia Testing Panel Now Available Bronson Laboratory offers a any impact on the patient’s therapy. Importantly, most people with an thrombophilia testing panel consisting For instance, the vast majority of older inheritable thrombophilic mutation will of the following: factor VIII activity, anti- patients with venous thromboses in the never experience a thrombotic event, thrombin III activity, protein setting of a recognized inciting event and most of those who do will never C activity, protein S antigen, factor V Leiden will not have a preexisting thrombophilic do so again. Because of this, screening mutation assay, prothrombin 90210A condition, and accordingly testing is the general population or even asympto- mutation assay, and a lupus anticoagulant generally not recommended in this pop- matic relatives of individuals with thrombo- assay. Abnormal values for protein C, ulation. In regards to arterial thromboses, philic mutations is discouraged because protein S, and antithrombin III will be the overwhelming majority are a direct of the potential for harmful overtreatment. automatically reflexed to confirmatory consequence of atherosclerosis, and the By similar reasoning, some hematologists testing at the Mayo Clinic laboratories. added presence of a thrombophilia in would recommend the same period of Although these tests are orderable indi- this setting will not affect patient anticoagulation, often 3-6 months after vidually, there is little rationale to do so management. (continued on page 4) except as noted below. Clinical circumstances that suggest The activity assays are clotting tests a laboratory evaluation for thrombophilia that require adequate amounts of func- tional protein to achieve a normal result. For reasons having to do with greater achievable precision, the free protein S Patient with a Asymptomatic patients Other clinical situations with a family history of VTE antigen test is used in lieu of an activity confirmed acute VTE assay, but it too depends on adequate amounts of circulating protein for a normal finding. -

HEMOCLOT™ Thrombin Time
HEMOCLOT™ Thrombin Time (T.T.) REF CK011K R 6 x 2 mL Sales and Support: CoaChrom Diagnostica GmbH REF CK011L R 6 x 8 mL www.coachrom.com | [email protected] Tel: +43-1-236 222 1 | Fax: +43-1-236 222 111 Toll-free contact for Germany: Tel: 0800-24 66 33-0 | Fax: 0800-24 66 33-3 Clotting method for the determination of Thrombin Time. English, last revision: 08-2019 INTENDED USE: R Reconstitute the contents of each vial with exactly: HEMOCLOT™ Thrombin Time (T.T.) kit is a clotting method for the in REF CK011K ➔ 2 mL of distilled water. vitro qualitative determination of Thrombin Time on human citrated REF CK011L ➔ 8 mL of distilled water. plasma, using manual or automated method. Shake vigorously until complete dissolution while avoiding formation of SUMMARY AND EXPLANATION: foam and load it directly on the analyzer following application guide Technical: instruction. The Thrombin Time is a coagulation assay measuring the time to For manual method, allow to stabilize for 15 minutes at room convert fibrinogen to fibrin. temperature (18-25°C), homogenize before use. Clinical:1 The Thrombin Time is a screening test to assess abnormalities of STORAGE AND STABILITY: fibrinogen and to detect inhibitors against thrombin or fibrin. It can be Unopened reagents should be stored at 2-8°C in their original useful for the evaluation of Disseminated Intravascular Coagulation packaging. Under these conditions, they can be used until the expiry (DIC) and liver disease. date printed on the kit. A prolonged Thrombin Time can result from: • Presence of antithrombin activity induced by therapy (eg Heparin, R Reagent stability after reconstitution, free from any contamination hirudin, argatroban, dabigatran). -

Reptilase@'-R-A New Reagent in Blmd Coagulation
British Journal of Haematology, 1971, 21, 43. Reptilase@'-R-A New Reagent in Blmd Coagulation C. FUNK,J. GMUR,R. HEROLDAND P. W. STRAUB Department of Medicine, Kantonsspital, University of Zurich, Switzerland (Received 8 September 1970; accepted for piiblication 29 September 1970) SUMMARY.Reptilase@-R, a purified thrombin-like snake-venom enzyme from Bothrops atrox, has been tested for its usefulness as a substitute for thrombin in two coagulation assay systems. Reptilase was found to be more stable than thrombin and not to be inhibited by heparin and hirudin. Performance of the Reptilase time allows the rapid exclusion of heparin con- tamination in plasma samples with prolonged thrombin times. In the presence of fibrinogenlfibrin split products, the Reptilase time is less prolonged than the thrombin time, whereas in patients with prolonged thrombin times because of congenital dysfibrinogenaemia the inverse is found. Thus, performance of both Reptilase time and thrombin time allows the rapid identification of three major causes for a prolongation of the thrombin time. In patients on heparin therapy because of a defibrination syndrome, the Reptilase time may replace the thrombin time as a guide for the degree of coagulation inhibition by FDP, although our re- sults show that it is somewhat less sensitive. Reptilase can also be substituted for thrombin in the rapid chronometric fibrino- gen assay. Unfortunately the advantages of reagent stability and insensitivity to heparin are balanced by a lesser reproducibility, especially in the presence of FDP. While thrombin liberates the fibrinopeptides of both the a- and p-chains of fibrinogen, the thrombin-like snake-venom enzyme Reptilase exclusively acts on the a-chain, thus leading to coagulation by liberating only fibrinopeptide A (Blombick et al, 1957; Stocker & Straub, 1970). -
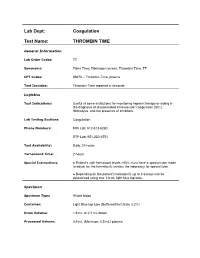
Thrombin Time
Lab Dept: Coagulation Test Name: THROMBIN TIME General Information Lab Order Codes: TT Synonyms: Fibrin Time; Fibrinogen screen, Thrombin Time, TT CPT Codes: 85670 – Thrombin Time, plasma Test Includes: Thrombin Time reported in seconds. Logistics Test Indications: Useful at some institutions for monitoring heparin therapy or aiding in the diagnosis of disseminated intravascular coagulation (DIC), fibrinolysis, and the presence of inhibitors. Lab Testing Sections: Coagulation Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6551 Test Availability: Daily, 24 hours Turnaround Time: 2 hours Special Instructions: ● Patient’s with hematocrit levels >55% must have a special tube made to adjust for the hematocrit; contact the laboratory for special tube. ● Depending on the patient's hematocrit, up to 3 assays can be determined using one 1.8 mL light blue top tube. Specimen Specimen Type: Whole blood Container: Light Blue top tube (Buffered Na Citrate 3.2%) Draw Volume: 1.8 mL or 2.7 mL blood Processed Volume: 0.9 mL (Minimum: 0.5 mL) plasma Collection: ● A clean venipuncture is essential, avoid foaming. ● Entire sample must be collected with single collection, pooling of sample is unacceptable. ● Capillary collection is unacceptable. ● Patient’s with a hematocrit level >55% must have a special tube made to adjust for the hematocrit; contact lab for a special tube. ● Mix thoroughly by gentle inversion. Deliver immediately to the laboratory at room temperature via courier or pneumatic tube. Off campus collections: ● Must be tested within 4 hours. ● Do not refrigerate. ● If not received in our lab within 4 hours of collection, sample must be centrifuged and *platelet-poor plasma removed from cells and transferred to an aliquot tube. -
Abnormal Hemostasis Screening Tests Leading to Diagnosis of Multiple Myeloma
Acta Haematologica Polonica 50(1) • March 2019 • 32-35 • DOI: 10.2478/ahp-2019-0006 CASE REPORT / KAZUISTYKA journal homepage: https://content.sciendo.com/ahp Abnormal hemostasis screening tests leading to diagnosis of multiple myeloma Article history: Abstract Received: 05.11.2018 Multiple myeloma (MM) is a rare malignancy, characterized by clonal proliferation of plasma cells, secreting monoclonal immunoglobu- Accepted: 04.02.2019 lin. It is usually diagnosed based on histopathologic and immunophenotypic bone marrow examination. Abnormal results of screening coagulation tests, including prothrombin time, activated partial thromboplastin time and thrombin time, are commonly encountered Teresa Iwaniec1*, in patients with plasma cell neoplasms. They do not, however, reflect bleeding tendency. We describe a 71-year-old patient who was Joanna Zdziarska2, 2 accidentally diagnosed with multiple myeloma during coagulation diagnostics. Artur Jurczyszyn © 2019 Polish Society of Hematology and Transfusion Medicine, Insitute of Hematology and Transfusion Medicine. All rights reserved. 1 Department of Medicine, Jagiellonian University Medical College, Krakow, Poland 2 Department of Haematology, Jagiellonian Keywords: University Medical College, Krakow, Poland multiple myleoma, paraprotein, hemostasis screening test, thrombin time Multiple myeloma (MM) is a rare malignancy, characterized by test results, including prothrombin time (PT), activated partial clonal proliferation of plasma cells. Monoclonal immunoglobulin thromboplastin time (APTT), and -

Partial Thromboplastin Time (PTT) CPT: 85730
Medicare National Coverage Determination Policy Partial Thromboplastin Time (PTT) CPT: 85730 CMS National Coverage Policy Coverage Indications, Limitations, and/or Medical Necessity Basic plasma coagulation function is readily assessed with a few simple laboratory tests: The Partial Thromboplastin Time (PTT), Prothrombin Time (PT), Thrombin Time (TT), or a quantitative fibrinogen determination. The PTT test is an in vitro laboratory test used to assess the intrinsic coagulation pathway and monitor heparin therapy. Indications 1. The PTT is most commonly used to quantitate the effect of therapeutic unfractionated heparin and to regulate its dosing. Except during transitions between heparin and warfarin therapy, in general both the PTT and PT are not necessary together to assess the effect of anticoagulation therapy. PT and PTT must be justified separately. 2. A PTT may be used to assess patients with signs or symptoms of hemorrhage orthrombosis. For example: • Abnormal bleeding, hemorrhage or hematoma petechiae or other signs ofthrombocytopenia that could be due to Disseminated Intravascular Coagulation • Swollen extremity with or without prior trauma 3. A PTT may be useful in evaluating patients who have a history of a condition known tobe associated with the risk of hemorrhage or thrombosis that is related to the intrinsiccoagulation pathway. Such abnormalities may be genetic or acquired. For example: • Dysfibrinogenemia; Afibrinogenemia (complete) • Acute or chronic liver dysfunction or failure, including Wilson’s disease • Hemophilia • Liver disease and failure; • Infectious processes • Bleeding disorders • Disseminated intravascular coagulation • Lupus erythematosus or other conditions associated with circulating inhibitors, e.g., factor VIII Inhibitor, lupus-like anticoagulant • Sepsis • Von Willebrand’s disease • Arterial and venous thrombosis, including the evaluation of hypercoagulable states • Clinical conditions associated with nephrosis or renal failure • Other acquired and congenital coagulopathies as well as thrombotic states 4. -
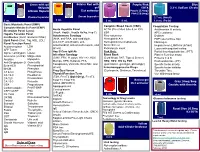
Order of Draw
Green with gel Gold or Red with Purple/Pink Blue 56 Units gel EDTA 3.2% Sodium Citrate Lithium Heparin Clot activator Purple (5.4mg) Pink (10.8mg) Plasma Separator Serum Separator 2.7 mL (Adult) 3 mL 5 mL 3 mL 6 mL 1.8 mL (Peds) Basic Metabolic Panel (BMP) Complete Blood Count (CBC) Coagulation Testing Complete Metabolic Panel (CMP) Acute Hepatitis Panel ACTH (Pre-chilled tube & on ICE) Antithrombin III activity Electrolyte Panel (Lytes) (HepA, HepBc, HepBs Ab/Ag, Hep C) ESR APC resistance Hepatic Function Panel Autoimmune Serology Flow cytometry D-dimer IronStudies (Iron/Transferrin/%Sat) (ANA, anti-DNA, anti-cardiolipin, Hemoglobin A1c FDP (special blue top) Lipid Panel (Chol, Trig, HDL, LDL) anti-CCP, anti-Gliadin, anti- Hemoglobin Electrophoresis Fibrinogen Renal Function Panel mitochondrial, anti-smooth muscle, and Sickle Screen Heparin level (LMWH & Unfract) Acetaminophen LDH others) Reticulocyte count Lupus anticoagulant testing AFP Tumor LH Hep B Core IgM Ab Pink Only: Partial thromboplastin time (PTT) Alpha-1-antitrypsin Lipase Infectious Serology Blood Bank Platelet Function assay Ammonia (on ICE) Magnesium (CMV, EBV, H. pylori, HIV 1+2, HSV, (Cord blood, DAT, Type & Screen) Proteins C & S Amylase Myoglobin Mumps, RPR, Rubeola, FTA, HBV, HCV, HIV by PCR Prothrombin time (PT) Anti-Streptolysin O Osmolality Toxoplasma, Varicella, West Nile, and (quantitative, genotype, phenotype) Specific factor activity Beta-HCG Phenobarbital others) Immunosuppressive Drugs Specific factor inhibitor BHOB Phenytoin Preg Qual Serum (Cyclosporin, -

Life-Threatening Hemorrhage Following Subcutaneous Heparin Therapy
CORE Metadata, citation and similar papers at core.ac.uk Provided by PubMed Central CASE REPORT Life-threatening hemorrhage following subcutaneous heparin therapy Jana Hudcova Abstract: Prophylactic administration of unfractionated heparin is a common practice in Daniel Talmor a perioperative period. Heparin monitoring with subcutaneous dosing is not recommended; however it becomes important in selected patients. We report a case of massive hemorrhage with Department of Anesthesia, Critical Care and Pain Medicine, Beth subcutaneous heparin administration in an HIV-positive male patient with cachexia and mild liver Israel Deaconess Medical Center dysfunction. Prolonged activated plasma thromboplastin time and thrombin time, but normal and Harvard Medical School, reptilase time well as response to protamine sulfate point towards the heparin effect. Inhibitor Boston, MA, USA screen was negative and factor VIII activity was normal. All these rule out the possibility of acquired factor VIII inhibitor or any other inhibitor and confi rm that this bleeding was due to heparin overdose. We believe that delayed clearance of UH secondary to possible involvement of reticuloendothelial system might have been be responsible for heparin overdose even though inadvertent administration of large dose of heparin intravenously can not be completely ruled out. Administration of unfractionated heparin to a patient with cachexia and abnormal liver function warrants close attention to heparin monitoring or switch to low molecular weight heparin since its mechanism of elimination differs. Keywords: unfractionated heparin, bleeding, prophylaxis, liver dysfunction, cachexia, HIV Introduction In critically ill patients, venous thromboembolism (VTE) prophylaxis has been included in the bundle of measures designed to prevent the development of complications in ventilated patients and became a core indicator of the quality of intensive care.1 Either low-dose unfractionated heparin (UH) or low molecular weight heparin (LMWH) is regularly used for prophylaxis. -

Transfusion Reaction Evaluation
Lab Dept: Transfusion Services Test Name: TRANSFUSION REACTION EVALUATION General Information Lab Order Codes: TRXR Synonyms: Transfusion Complication Workup; Hemolytic reaction CPT Codes: Dependent on testing involved. Refer to individual serologic procedures. Test Includes: If there is any evidence of significant reaction other than mild urticaria, stop the transfusion but keep normal saline dripping in slowly to keep the I.V. open. Report all reactions to Transfusion Service (612-813-6824/651-220-6558). Clerical Check: Examination of label on blood container(s) and all clerical work and records for possible error, and review possible mirror image or other-side-of-the-coin error. (If one unit is infused into a wrong patient, has another patient/unit been also mixed up?) Visible Plasma Hemoglobin: Examination of prereaction and postreaction serum or plasma for hemolysis or jaundice. This should be begun by examination of the postreaction blood sample sent very promptly to the Transfusion Service. Direct antiglobulin test on postreaction specimen. (If positive, it must be compared with a pretransfusion specimen.) ABO/Rh on Post reaction specimen. If the above are negative and there is no suspicion of incompatibility, additional tests are not essential. Minor reactions (e.g., febrile or allergic) need no further work-up. If actual hemolysis is suspected, the following may be done. Blood container, attached transfusion set and intravenous solutions must be sent to Transfusion Service. Culture of remaining donor blood, if: Patient temperature is ≥39ºC Patient’s temperature increases ≥2ºC Patient’s temperature increases ≥1ºC and is associated with chills and rigors. Repeat ABO and Rh typing on patient and donor blood; compare with previous reports.