Priority Health Spine and Joint Code List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Anterior Reconstruction Techniques for Cervical Spine Deformity
Neurospine 2020;17(3):534-542. Neurospine https://doi.org/10.14245/ns.2040380.190 pISSN 2586-6583 eISSN 2586-6591 Review Article Anterior Reconstruction Techniques Corresponding Author for Cervical Spine Deformity Samuel K. Cho 1,2 1 1 1 https://orcid.org/0000-0001-7511-2486 Murray Echt , Christopher Mikhail , Steven J. Girdler , Samuel K. Cho 1Department of Orthopedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA Department of Orthopaedics, Icahn 2 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, School of Medicine at Mount Sinai, 425 NY, USA West 59th Street, 5th Floor, New York, NY, USA E-mail: [email protected] Cervical spine deformity is an uncommon yet severely debilitating condition marked by its heterogeneity. Anterior reconstruction techniques represent a familiar approach with a range Received: June 24, 2020 of invasiveness and correction potential—including global or focal realignment in the sagit- Revised: August 5, 2020 tal and coronal planes. Meticulous preoperative planning is required to improve or prevent Accepted: August 17, 2020 neurologic deterioration and obtain satisfactory global spinal harmony. The ability to per- form anterior only reconstruction requires mobility of the opposite column to achieve cor- rection, unless a combined approach is planned. Anterior cervical discectomy and fusion has limited focal correction, but when applied over multiple levels there is a cumulative ef- fect with a correction of approximately 6° per level. Partial or complete corpectomy has the ability to correct sagittal deformity as well as decompress the spinal canal when there is an- terior compression behind the vertebral body. -

2019 Spine Coding Basics
2019 Spine Coding Basics Presenter: Kerri Larson, CPC Directory of Coding and Audit Services 2019 Spine Surgery 01 Spine Surgery Terminology & Anatomy 02 Spine Procedures 03 Case Study 04 Diagnosis 05 Q & A Spine Surgery Terminology & Anatomy Spine Surgery Terminology & Anatomy Term Definition Arthrodesis Fusion, or permanent joining, of a joint, or point of union of two musculoskeletal structures, such as two bones Surgical procedure that replaces missing bone with material from the patient's own body, or from an artificial, synthetic, or Bone grafting natural substitute Corpectomy Surgical excision of the main body of a vertebra, one of the interlocking bones of the back. Cerebrospinal The protective body fluid present in the dura, the membrane covering the brain and spinal cord fluid or CSF Decompression A procedure to remove pressure on a structure. Diskectomy, Surgical removal of all or a part of an intervertebral disc. discectomy Dura Outermost of the three layers that surround the brain and spinal cord. Electrode array Device that contains multiple plates or electrodes. Electronic pulse A device that produces low voltage electrical pulses, with a regular or intermittent waveform, that creates a mild tingling or generator or massaging sensation that stimulates the nerve pathways neurostimulator Spine Surgery Terminology & Anatomy Term Definition The space that surrounds the dura, which is the outermost layer of membrane that surrounds the spinal canal. The epidural space houses the Epidural space spinal nerve roots, blood and lymphatic vessels, and fatty tissues . Present inside the skull but outside the dura mater, which is the thick, outermost membrane covering the brain or within the spine but outside Extradural the dural sac enclosing the spinal cord, nerve roots and spinal fluid. -

Effectiveness of Distal Tibial Osteotomy
Nozaka et al. BMC Musculoskeletal Disorders (2020) 21:31 https://doi.org/10.1186/s12891-020-3061-7 RESEARCH ARTICLE Open Access Effectiveness of distal tibial osteotomy with distraction arthroplasty in varus ankle osteoarthritis Koji Nozaka* , Naohisa Miyakoshi, Takeshi Kashiwagura, Yuji Kasukawa, Hidetomo Saito, Hiroaki Kijima, Shuichi Chida, Hiroyuki Tsuchie and Yoichi Shimada Abstract Background: In highly active older individuals, end-stage ankle osteoarthritis has traditionally been treated using tibiotalar arthrodesis, which provides considerable pain relief. However, there is a loss of ankle joint movement and a risk of future arthrosis in the adjacent joints. Distraction arthroplasty is a simple method that allows joint cartilage repair; however, the results are currently mixed, with some reports showing improved pain scores and others showing no improvement. Distal tibial osteotomy (DTO) without fibular osteotomy is a type of joint preservation surgery that has garnered attention in recent years. However, to our knowledge, there are no reports on DTO with joint distraction using a circular external fixator. Therefore, the purpose of this study was to examine the effect of DTO with joint distraction using a circular external fixator for treating ankle osteoarthritis. Methods: A total of 21 patients with medial ankle arthritis were examined. Arthroscopic synovectomy and a microfracture procedure were performed, followed by angled osteotomy and correction of the distal tibia; the ankle joint was then stabilized after its condition improved. An external fixator was used in all patients, and joint distraction of approximately 5.8 mm was performed. All patients were allowed full weight-bearing walking immediately after surgery. Results: The anteroposterior and lateral mortise angle during weight-bearing, talar tilt angle, and anterior translation of the talus on ankle stress radiography were improved significantly (P < 0.05). -

Two-Level Cervical Corpectomy—Long-Term Follow-Up Reveals the High Rate of Material Failure in Patients, Who Received an Anterior Approach Only
Neurosurgical Review (2019) 42:511–518 https://doi.org/10.1007/s10143-018-0993-6 ORIGINAL ARTICLE Two-level cervical corpectomy—long-term follow-up reveals the high rate of material failure in patients, who received an anterior approach only Simon Heinrich Bayerl1 & Florian Pöhlmann1 & Tobias Finger1 & Vincent Prinz1 & Peter Vajkoczy 1 Received: 25 August 2017 /Revised: 20 November 2017 /Accepted: 5 December 2017 /Published online: 18 June 2018 # Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract In contrast to a one-level cervical corpectomy, a multilevel corpectomy without posterior fusion is accompanied by a high material failure rate. So far, the adequate surgical technique for patients, who receive a two-level corpectomy, remains to be elucidated. The aim of this study was to determine the long-term clinical outcome of patients with cervical myelopathy, who underwent a two-level corpectomy. Outcome parameters of 21 patients, who received a two-level cervical corpectomy, were retrospectively analyzed concerning reoperations and outcome scores (VAS, Neck Disability Index (NDI), Nurick scale, mod- ified Japanese Orthopaedic Association score (mJOAS), Short Form 36-item Health Survey Questionnaire (SF-36)). The failure rate was determined using postoperative radiographs. The choice over the surgical procedures was exercised by every surgeon individually. Therefore, a distinction between two groups was possible: (1) anterior group (ANT group) with a two-level corpectomy and a cervical plate, (2) anterior/posterior group (A/P group) with two-level corpectomy, cervical plate, and addi- tional posterior fusion. Both groups benefitted from surgery concerning pain, disability, and myelopathy. While all patients of the A/P group showed no postoperative instability, one third of the patients of the ANT group exhibited instability and clinical deterioration. -

The Need for Structural Allograft Biomechanical Guidelines
8 The Need for Structural Allograft Biomechanical Guidelines Satoshi Kawaguchi, MD Robert A. Hart, MD Abstract Because of their osteoconductive properties, structural bone allografts retain a theoretic advantage in biologic performance compared with artifi cial interbody fusion devices and endoprostheses. Current regulations have addressed the risks of disease transmission and tissue contamination, but comparatively few guidelines exist regarding donor eligibility and bone processing issues with a potential effect on the mechanical integrity of structural allograft bone. The lack of guidelines appears to have led to variation among allograft providers in terms of processing and donor screening regarding issues with recognized mechanical effects. Given the relative lack of data on which to base reasonable screening standards, a basic biomechanical evaluation was performed on one source of structural bone allograft, the femoral ring. Of the tested parameters, the minimum and maximum cortical wall thicknesses of femoral ring allograft were most strongly correlated with the axial compressive load to failure of the graft, suggesting that cortical wall thickness may be a useful screening tool for compressive resistance expected from fresh cortical bone allograft. Development of further biomechanical and clinical data to direct standard development appears warranted. Instr Course Lect 2015;64:87–93. Surgical implantation of structural al- form with limited anatomic modifi - by the US FDA as well as through vol- lograft bone continues to increase de- cations, modern tissue processing in- untary participation with the American spite advances in modern alternatives cludes preparations of amalgams of Association of Tissue Banks (AATB). to allograft, including spine interbody allograft bone tissue of specifi c shapes Guidelines for allograft bone products fusion devices and peripheral joint en- and sizes to suit specifi c surgical needs. -
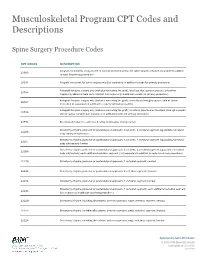
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Differences Between Subtotal Corpectomy and Laminoplasty for Cervical Spondylotic Myelopathy
Spinal Cord (2010) 48, 214–220 & 2010 International Spinal Cord Society All rights reserved 1362-4393/10 $32.00 www.nature.com/sc ORIGINAL ARTICLE Differences between subtotal corpectomy and laminoplasty for cervical spondylotic myelopathy S Shibuya1, S Komatsubara1, S Oka2, Y Kanda1, N Arima1 and T Yamamoto1 1Department of Orthopaedic Surgery, School of Medicine, Kagawa University, Kagawa, Japan and 2Oka Orthopaedic and Rehabilitation Clinic, Kagawa, Japan Objective: This study aimed to obtain guidelines for choosing between subtotal corpectomy (SC) and laminoplasty (LP) by analysing the surgical outcomes, radiological changes and problems associated with each surgical modality. Study Design: A retrospective analysis of two interventional case series. Setting: Department of Orthopaedic Surgery, Kagawa University, Japan. Methods: Subjects comprised 34 patients who underwent SC and 49 patients who underwent LP. SC was performed by high-speed drilling to remove vertebral bodies. Autologous strut bone grafting was used. LP was performed as an expansive open-door LP. The level of decompression was from C3 to C7. Clinical evaluations included recovery rate (RR), frequency of C5 root palsy after surgery, re-operation and axial pain. Radiographic assessments included sagittal cervical alignment and bone union. Results: Comparisons between the two groups showed no significant differences in age at surgery, preoperative factors, RR and frequency of C5 palsy. Progression of kyphotic changes, operation time and volumes of blood loss and blood transfusion were significantly greater in the SC (two- or three- level) group. Six patients in the SC group required additional surgery because of pseudoarthrosis, and four patients underwent re-operation because of adjacent level disc degeneration. -

Analysis of a Spine Registry Rate Among Smokers Undergoing
No Difference in Functional Outcome but Higher Revision Rate Among Smokers Undergoing Cervical Artificial Disc Replacement: Analysis of a Spine Registry Lee Wen-Shen, Maksim Lai Wern Sheng, William Yeo, Tan Seang Beng, Yue Wai Mun, Guo Chang Ming and Mohammad Mashfiqul Arafin Siddiqui Int J Spine Surg published online 29 December 2020 http://ijssurgery.com/content/early/2020/12/17/7140 This information is current as of October 2, 2021. Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://ijssurgery.com/alerts The International Journal of Spine Surgery 2397 Waterbury Circle, Suite 1, Aurora, IL 60504, Phone: +1-630-375-1432 © 2020 ISASS. All RightsDownloaded Reserved. from http://ijssurgery.com/ by guest on October 2, 2021 International Journal of Spine Surgery, Vol. 00, No. 00, 0000, pp. 000–000 https://doi.org/10.14444/7140 ÓInternational Society for the Advancement of Spine Surgery No Difference in Functional Outcome but Higher Revision Rate Among Smokers Undergoing Cervical Artificial Disc Replacement: Analysis of a Spine Registry LEE WEN-SHEN, MBBS (HONS),1,2 MAKSIM LAI WERN SHENG, MBBS,1 WILLIAM YEO,3 TAN SEANG BENG, MBBS, FRCS,1 YUE WAI MUN, MBBS, FRCS,1 GUO CHANG MING, MBBS, FRCS,1 MOHAMMAD MASHFIQUL ARAFIN SIDDIQUI, MBBS, FRCS1 1Department of Orthopaedic Surgery, Singapore General Hospital, Singapore 2Department of Surgery, The Alfred Hospital, Melbourne, Australia, 3Statistics and Clinical Research, Singapore General Hospital, Singapore ABSTRACT Background: Smoking is a known predictor of negative outcomes in spinal surgery. However, its effect on the functional outcomes and revision rates after ADR is not well-documented. -

Clinical Guidelines
CLINICAL GUIDELINES Interventional Pain Management Services Version 1.0.2019 Clinical guidelines for medical necessity review of comprehensive musculoskeletal management services. © 2019 eviCore healthcare. All rights reserved. Regence: Comprehensive Musculoskeletal Management Guidelines V1.0.2019 Interventional Pain Management CMM-200: Epidural Steroid Injections (ESI) 3 CMM-201: Facet Joint Injections/Medial Branch Blocks 17 CMM-202: Trigger Point Injections 21 CMM-203: Sacroiliac Joint Injections 32 CMM-204: Prolotherapy 37 CMM-207: Epidural Adhesiolysis 40 CMM-208: Radiofrequency Joint Ablations/Denervations 44 CMM-209: Regional Sympathetic Blocks 51 CMM 210: Implantable Intrathecal Drug Delivery Systems 57 CMM-211: Spinal Cord Stimulators 65 CMM-308: Thermal Intradiscal Procedures 66 CMM-310: Manipulation of the Spine Under Anesthesia 71 ______________________________________________________________________________________________________ © 2019 eviCore healthcare. All Rights Reserved. Page 2 of 73 400 Buckwalter Place Boulevard, Bluffton, SC 29910 (800) 918-8924 www.eviCore.com Regence: Comprehensive Musculoskeletal Management Guidelines V1.0.2019 CMM-200: Epidural Steroid Injections (ESI) CMM-200.1: Definitions 4 CMM-200.2: General Guidelines 5 CMM-200.3: Indications: Selective Nerve Root Block (SNRB) 6 CMM-200.4: Indications: Epidural Steroid Injections 7 CMM-200.5: Non-Indications: SNRB 8 CMM-200.6: Non-Indications: ESI 8 ® CMM-200.7: Procedure (CPT ) Codes 9 CMM-200.8: References 10 ______________________________________________________________________________________________________ -

TESSYS Technique with Small Grade of Facetectomy Has Potential Biomechanical Advantages Compared to the In-Out TED with Intact Articular Process : an In-Silico Study
TESSYS Technique With Small Grade of Facetectomy Has Potential Biomechanical Advantages Compared to the In-Out TED With Intact Articular Process : An In-Silico Study Jingchi Li West China Hospital/West China School of Medicine for Sichuan University Chen Xu Changzheng Hospital Aliated to the Naval Medical University Xiaoyu Zhang Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Zhipeng Xi Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Mengnan Liu Macau University of Science and Technology Zhongxin Fang Xihua University Nan Wang Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Lin Xie ( [email protected] ) Aliated Hospital of Integrated Traditional Chinese and Western Medicine for Nanjing University of Chinese Medicine Yueming Song West China Hospital/West China School of Medicine for Sichuan University Research Article Keywords: Biomechanical deterioration, Transforaminal endoscopic discectomy, Endoscopic dynamic drill, Facetectomy, Iatrogenic annulus injury Posted Date: April 26th, 2021 Page 1/27 DOI: https://doi.org/10.21203/rs.3.rs-429749/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published at BMC Musculoskeletal Disorders on July 10th, 2021. See the published version at https://doi.org/10.1186/s12891-021-04504-1. Page 2/27 Abstract Background: The facetectomy was reported as an important procedure in both in-out and out-in (i.e. transforaminal endoscopic spine system (TESSYS)) techniques in the transforaminal endoscopic discectomy (TED), and which was also related to the deterioration of postoperative biomechanical environment and related poor prognosis. -

Musculoskeletal Surgical Procedures Requiring Prior Authorization (Effective 11.1.2020)
Musculoskeletal Surgical Procedures Requiring Prior Authorization (Effective 11.1.2020) Procedure Code Description ACL Repair 27407 Repair, primary, torn ligament and/or capsule, knee; cruciate ACL Repair 27409 Repair, primary, torn ligament and/or capsule, knee; collateral and cruciate ligaments ACL Repair 29888 Arthroscopically aided anterior cruciate ligament repair/augmentation or reconstruction Acromioplasty and Rotator Cuff Repair 23130 Acromioplasty Or Acromionectomy, Partial, With Or Without Coracoacromial Ligament Release Acromioplasty and Rotator Cuff Repair 23410 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open; acute Acromioplasty and Rotator Cuff Repair 23412 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open; chronic Acromioplasty and Rotator Cuff Repair 23415 Coracoacromial Ligament Release, With Or Without Acromioplasty Acromioplasty and Rotator Cuff Repair 23420 Reconstruction of complete shoulder (rotator) cuff avulsion, chronic (includes acromioplasty) Arthroscopy, Shoulder, Surgical; Decompression Of Subacromial Space With Partial Acromioplasty, With Coracoacromial Ligament (Ie, Arch) Release, When Performed (List Separately In Addition Acromioplasty and Rotator Cuff Repair 29826 To Code For Primary Procedure) Acromioplasty and Rotator Cuff Repair 29827 Arthroscopy, shoulder, surgical; with rotator cuff repair Allograft for Spinal Fusion [BMP] 20930 Allograft, morselized, or placement of osteopromotive material, for spine surgery only Ankle Fusion 27870 Arthrodesis, ankle, open Ankle Fusion -

Knee Joint Surgery: Open Synovectomy
Musculoskeletal Surgical Services: Open Surgical Procedures; Knee Joint Surgery: Open Synovectomy POLICY INITIATED: 06/30/2019 MOST RECENT REVIEW: 06/30/2019 POLICY # HH-5588 Overview Statement The purpose of these clinical guidelines is to assist healthcare professionals in selecting the medical service that may be appropriate and supported by evidence to improve patient outcomes. These clinical guidelines neither preempt clinical judgment of trained professionals nor advise anyone on how to practice medicine. The healthcare professionals are responsible for all clinical decisions based on their assessment. These clinical guidelines do not provide authorization, certification, explanation of benefits, or guarantee of payment, nor do they substitute for, or constitute, medical advice. Federal and State law, as well as member benefit contract language, including definitions and specific contract provisions/exclusions, take precedence over clinical guidelines and must be considered first when determining eligibility for coverage. All final determinations on coverage and payment are the responsibility of the health plan. Nothing contained within this document can be interpreted to mean otherwise. Medical information is constantly evolving, and HealthHelp reserves the right to review and update these clinical guidelines periodically. No part of this publication may be reproduced, stored in a retrieval system or transmitted, in any form or by any means, electronic, mechanical, photocopying, or otherwise, without permission from HealthHelp.