2019 Spine Coding Basics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Modified Plate-Only Open-Door Laminoplasty Versus Laminectomy and Fusion for the Treatment of Cervical Stenotic Myelopathy
n Feature Article Modified Plate-only Open-door Laminoplasty Versus Laminectomy and Fusion for the Treatment of Cervical Stenotic Myelopathy LILI YANG, MD; YIFEI GU, MD; JUEQIAN SHI, MD; RUI GAO, MD; YANG LIU, MD; JUN LI, MD; WEN YUAN, MD, PHD abstract Full article available online at Healio.com/Orthopedics. Search: 20121217-23 The purpose of this study was to compare modified plate-only laminoplasty and lami- nectomy and fusion to confirm which of the 2 surgical modalities could achieve a better decompression outcome and whether a significant difference was found in postopera- tive complications. Clinical data were retrospectively reviewed for 141 patients with cervical stenotic myelopathy who underwent plate-only laminoplasty and laminectomy and fusion between November 2007 and June 2010. The extent of decompression was assessed by measuring the cross-sectional area of the dural sac and the distance of spinal cord drift at the 3 most narrowed levels on T2-weighted magnetic resonance imaging. Clinical outcomes and complications were also recorded and compared. Significant en- largement of the dural sac area and spinal cord drift was achieved and well maintained in both groups, but the extent of decompression was greater in patients who underwent Figure: T2-weighted magnetic resonance image laminectomy and fusion; however, a greater decompression did not seem to produce a showing the extent of decompression assessed by better clinical outcome. No significant difference was observed in Japanese Orthopaedic measuring the cross-sectional area of the dural sac Association and Nurick scores between the 2 groups. Patients who underwent plate-only (arrow). laminoplasty showed a better improvement in Neck Dysfunction Index and visual ana- log scale scores. -

Anterior Reconstruction Techniques for Cervical Spine Deformity
Neurospine 2020;17(3):534-542. Neurospine https://doi.org/10.14245/ns.2040380.190 pISSN 2586-6583 eISSN 2586-6591 Review Article Anterior Reconstruction Techniques Corresponding Author for Cervical Spine Deformity Samuel K. Cho 1,2 1 1 1 https://orcid.org/0000-0001-7511-2486 Murray Echt , Christopher Mikhail , Steven J. Girdler , Samuel K. Cho 1Department of Orthopedics, Icahn School of Medicine at Mount Sinai, New York, NY, USA Department of Orthopaedics, Icahn 2 Department of Neurological Surgery, Montefiore Medical Center/Albert Einstein College of Medicine, Bronx, School of Medicine at Mount Sinai, 425 NY, USA West 59th Street, 5th Floor, New York, NY, USA E-mail: [email protected] Cervical spine deformity is an uncommon yet severely debilitating condition marked by its heterogeneity. Anterior reconstruction techniques represent a familiar approach with a range Received: June 24, 2020 of invasiveness and correction potential—including global or focal realignment in the sagit- Revised: August 5, 2020 tal and coronal planes. Meticulous preoperative planning is required to improve or prevent Accepted: August 17, 2020 neurologic deterioration and obtain satisfactory global spinal harmony. The ability to per- form anterior only reconstruction requires mobility of the opposite column to achieve cor- rection, unless a combined approach is planned. Anterior cervical discectomy and fusion has limited focal correction, but when applied over multiple levels there is a cumulative ef- fect with a correction of approximately 6° per level. Partial or complete corpectomy has the ability to correct sagittal deformity as well as decompress the spinal canal when there is an- terior compression behind the vertebral body. -

Analysis of the Cervical Spine Alignment Following Laminoplasty and Laminectomy
Spinal Cord (1999) 37, 20± 24 ã 1999 International Medical Society of Paraplegia All rights reserved 1362 ± 4393/99 $12.00 http://www.stockton-press.co.uk/sc Analysis of the cervical spine alignment following laminoplasty and laminectomy Shunji Matsunaga1, Takashi Sakou1 and Kenji Nakanisi2 1Department of Orthopaedic Surgery, Faculty of Medicine, Kagoshima University; 2Department of Mechanical Engineering, Faculty of Engineering, Kagoshima University, Sakuragaoka, Kagoshima, Japan Very little detailed biomechanical examination of the alignment of the cervical spine following laminoplasty has been reported. We performed a comparative study regarding the buckling- type alignment that follows laminoplasty and laminectomy to know the mechanical changes in the alignment of the cervical spine. Lateral images of plain roentgenograms of the cervical spine were put into a computer and examined using a program we developed for analysis of the buckling-type alignment. Sixty-four patients who underwent laminoplasty and 37 patients who underwent laminectomy were reviewed retrospectively. The subjects comprised patients with cervical spondylotic myelopathy (CSM) and those with ossi®cation of the posterior longitudinal ligament (OPLL). The postoperative observation period was 6 years and 7 months on average after laminectomy, and 5 years and 6 months on average following laminoplasty. Development of the buckling-type alignment was found in 33% of patients following laminectomy and only 6% after laminoplasty. Development of buckling-type alignment following laminoplasty appeared markedly less than following laminectomy in both CSM and OPLL patients. These results favor laminoplasty over laminectomy from the aspect of mechanics. Keywords: laminoplasty; laminectomy; buckling; kyphosis; swan-neck deformity Introduction In 1930, Eiselberg1 reported a case of postoperative of postoperative abnormal alignment from the aspect kyphosis of the spine following laminectomy from the of the presence or absence of buckling-type alignment. -

Lumbar Laminectomy
Patient Education Lumbar Laminectomy Description The spine consists of five separate divisions: cervical (seven vertebrae), thoracic (12 vertebrae), lumbar (five vertebrae), the sacrum, and the coccyx. Each vertebra, interlocks with the segment above and below it through the superior and inferior articular processes. Between each vertebra is an intervertebral disc that provides cushioning for the spine. The lamina and pedicle, along with the vertebral body, provide the borders that create the spinal canal, which the spinal cord runs through to transmit nerve signals. There are several different scenarios or conditions that may produce symptoms that would lead your physician to further Medical Illustration © 2016 Nucleus Medical Art, Inc. investigate, and possibly recommend this surgery. Stenosis causing Radicular Pain Spinal stenosis is the narrowing of the articular spaces within the spine; this may impinge on the nerves or the spinal cord. This is a degenerative process and may eventually lead to further changes on the spine over time. Radicular symptoms are pain, numbness, weakness, tingling, etc., that radiate along a specific nerve root (or dermatome) to other parts of the body outside of the spine. Surgical correction of this problem may include a minimally invasive decompression (shaving bone away to create more space around the nerve), often referred to as laminectomy (removing part or all of the lamina in order to provide more space and relieve impingement). In some cases, movement of one vertebrae slipping against another (spondylolisthesis), may require a vertebral fusion. This may be performed open vs. minimally invasive. Disc Herniation Herniation of the intervertebral disc may be due to an acute traumatic incident. -
Modern Advances in Joint Replacement and Rapid Recovery
Modern Advances in Joint Replacement and Rapid Recovery UCSF Osher Mini-Med School Lecture Series Jeffrey Barry, M.D. Assistant Professor of Orthopaedic Surgery Division of Adult Reconstruction University of California, San Francisco Disclosures . No relevant disclosures to this talk About Me . Bay Area Native . UCSF - U Can Stay Forever Outline . Burden of Disease and Epidemiology . The Basics of Hip and Knee Replacement . What’s improving over the last decade - Longevity - Pain Management - Hospital Stay - Thromboembolism prophylaxis - Risk Reduction Question What is the most common inpatient surgery performed in the US? 1. Percutaneous coronary angioplasty 2. Total hip replacement 3. Lumbar Laminectomy 4. Appendectomy 5. Total knee replacement Burden of Disease . Arthritis = most common cause of disability in the US . 22.7% of adults have doctor-diagnosed arthritis - 43.2% of patients with arthritis report activity limitations due to disease . By 2030: - 3.5 million TKA (673%) - 570,000 THA (174%) . Curve updated 2014 – just as predicted! Causes of Increased Utilization . Aging Population . Patients receiving arthroplasty at a younger age - Improvements in technology - Obesity Why Replace a Joint? Arthritis arthro – joint itis – inflammation What is Arthritis – Disease of Cartilage . Cartilage Degeneration - Pain - Limp - Swelling - Loss of range of motion - Eventual deformity Arthritis Affects on Your Life • Quality of Life • Independence • Movement, Walking, Exercise • Self-image • Self-esteem • Family Life • Sleep • Everything and Everybody Causes of Arthritis . Osteoarthritis - “wear and tear” . Inflammatory arthritis . Trauma, old fractures . Infection . Osteonecrosis - “lack of oxygen to the bone” . Childhood/ developmental disease Diagnosis . Clinical Symptoms + Radiographic . Radiographs – Standing or Weight bearing! . MRI is RARELY needed!!! - Expensive - Brings in other issues - Unnecessary treatment - Unnecessary explanations Knee Arthritis . -

Two-Level Cervical Corpectomy—Long-Term Follow-Up Reveals the High Rate of Material Failure in Patients, Who Received an Anterior Approach Only
Neurosurgical Review (2019) 42:511–518 https://doi.org/10.1007/s10143-018-0993-6 ORIGINAL ARTICLE Two-level cervical corpectomy—long-term follow-up reveals the high rate of material failure in patients, who received an anterior approach only Simon Heinrich Bayerl1 & Florian Pöhlmann1 & Tobias Finger1 & Vincent Prinz1 & Peter Vajkoczy 1 Received: 25 August 2017 /Revised: 20 November 2017 /Accepted: 5 December 2017 /Published online: 18 June 2018 # Springer-Verlag GmbH Germany, part of Springer Nature 2018 Abstract In contrast to a one-level cervical corpectomy, a multilevel corpectomy without posterior fusion is accompanied by a high material failure rate. So far, the adequate surgical technique for patients, who receive a two-level corpectomy, remains to be elucidated. The aim of this study was to determine the long-term clinical outcome of patients with cervical myelopathy, who underwent a two-level corpectomy. Outcome parameters of 21 patients, who received a two-level cervical corpectomy, were retrospectively analyzed concerning reoperations and outcome scores (VAS, Neck Disability Index (NDI), Nurick scale, mod- ified Japanese Orthopaedic Association score (mJOAS), Short Form 36-item Health Survey Questionnaire (SF-36)). The failure rate was determined using postoperative radiographs. The choice over the surgical procedures was exercised by every surgeon individually. Therefore, a distinction between two groups was possible: (1) anterior group (ANT group) with a two-level corpectomy and a cervical plate, (2) anterior/posterior group (A/P group) with two-level corpectomy, cervical plate, and addi- tional posterior fusion. Both groups benefitted from surgery concerning pain, disability, and myelopathy. While all patients of the A/P group showed no postoperative instability, one third of the patients of the ANT group exhibited instability and clinical deterioration. -

The Need for Structural Allograft Biomechanical Guidelines
8 The Need for Structural Allograft Biomechanical Guidelines Satoshi Kawaguchi, MD Robert A. Hart, MD Abstract Because of their osteoconductive properties, structural bone allografts retain a theoretic advantage in biologic performance compared with artifi cial interbody fusion devices and endoprostheses. Current regulations have addressed the risks of disease transmission and tissue contamination, but comparatively few guidelines exist regarding donor eligibility and bone processing issues with a potential effect on the mechanical integrity of structural allograft bone. The lack of guidelines appears to have led to variation among allograft providers in terms of processing and donor screening regarding issues with recognized mechanical effects. Given the relative lack of data on which to base reasonable screening standards, a basic biomechanical evaluation was performed on one source of structural bone allograft, the femoral ring. Of the tested parameters, the minimum and maximum cortical wall thicknesses of femoral ring allograft were most strongly correlated with the axial compressive load to failure of the graft, suggesting that cortical wall thickness may be a useful screening tool for compressive resistance expected from fresh cortical bone allograft. Development of further biomechanical and clinical data to direct standard development appears warranted. Instr Course Lect 2015;64:87–93. Surgical implantation of structural al- form with limited anatomic modifi - by the US FDA as well as through vol- lograft bone continues to increase de- cations, modern tissue processing in- untary participation with the American spite advances in modern alternatives cludes preparations of amalgams of Association of Tissue Banks (AATB). to allograft, including spine interbody allograft bone tissue of specifi c shapes Guidelines for allograft bone products fusion devices and peripheral joint en- and sizes to suit specifi c surgical needs. -

Lumbar Laminectomy Or Laminotomy
Patient Instructions: Lumbar Laminectomy or Laminotomy Surgical Technique A lumbar laminectomy or laminotomy is a surgical approach performed from the back of the lumbar spine. It is usually done through an incision in the middle of the back. Using minimally invasive techniques a small window of bone is drilled in the lamina to allow the surgeon to unpinch the underlying nerves (laminotomy), or in more severe cases the bone is removed completely on both sides to allow nerves on both sides of the spinal canal to be decompressed (laminectomy). It is done using an operating microscope and microsurgical technique. It is used to treat spinal stenosis or lateral recess stenosis and alleviate the pain and/or numbness that occurs in a patients lower back or legs. It can many times be performed on an outpatient basis without the need for an overnight stay in a hospital. Before Surgery • Seven days prior to surgery, please do not take any anti-inflammatory NSAID medications (Celebrex, Ibuprofen, Aleve, Naprosyn, Advil, etc.) as this could prolong your bleeding time during surgery. • Do not eat or drink anything after midnight the day before surgery. This means nothing to drink the morning of surgery except you may take your normal medication with a sip of water if needed. This includes your blood pressure medicine, which in general should be taken. Consult your surgeon or primary care doctor regarding insulin if you take it. • Please do not be late to check in on the day of surgery or it may be cancelled. • Please bring your preoperative folder with you to the surgery and have it when you check in. -
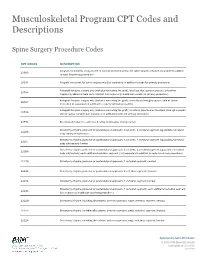
Musculoskeletal Program CPT Codes and Descriptions
Musculoskeletal Program CPT Codes and Descriptions Spine Surgery Procedure Codes CPT CODES DESCRIPTION Allograft, morselized, or placement of osteopromotive material, for spine surgery only (List separately in addition 20930 to code for primary procedure) 20931 Allograft, structural, for spine surgery only (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); local (eg, ribs, spinous process, or laminar 20936 fragments) obtained from same incision (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); morselized (through separate skin or fascial 20937 incision) (List separately in addition to code for primary procedure) Autograft for spine surgery only (includes harvesting the graft); structural, bicortical or tricortical (through separate 20938 skin or fascial incision) (List separately in addition to code for primary procedure) 20974 Electrical stimulation to aid bone healing; noninvasive (nonoperative) Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22206 body subtraction); thoracic Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22207 body subtraction); lumbar Osteotomy of spine, posterior or posterolateral approach, 3 columns, 1 vertebral segment (eg, pedicle/vertebral 22208 body subtraction); each additional vertebral segment (List separately in addition to code for -

Differences Between Subtotal Corpectomy and Laminoplasty for Cervical Spondylotic Myelopathy
Spinal Cord (2010) 48, 214–220 & 2010 International Spinal Cord Society All rights reserved 1362-4393/10 $32.00 www.nature.com/sc ORIGINAL ARTICLE Differences between subtotal corpectomy and laminoplasty for cervical spondylotic myelopathy S Shibuya1, S Komatsubara1, S Oka2, Y Kanda1, N Arima1 and T Yamamoto1 1Department of Orthopaedic Surgery, School of Medicine, Kagawa University, Kagawa, Japan and 2Oka Orthopaedic and Rehabilitation Clinic, Kagawa, Japan Objective: This study aimed to obtain guidelines for choosing between subtotal corpectomy (SC) and laminoplasty (LP) by analysing the surgical outcomes, radiological changes and problems associated with each surgical modality. Study Design: A retrospective analysis of two interventional case series. Setting: Department of Orthopaedic Surgery, Kagawa University, Japan. Methods: Subjects comprised 34 patients who underwent SC and 49 patients who underwent LP. SC was performed by high-speed drilling to remove vertebral bodies. Autologous strut bone grafting was used. LP was performed as an expansive open-door LP. The level of decompression was from C3 to C7. Clinical evaluations included recovery rate (RR), frequency of C5 root palsy after surgery, re-operation and axial pain. Radiographic assessments included sagittal cervical alignment and bone union. Results: Comparisons between the two groups showed no significant differences in age at surgery, preoperative factors, RR and frequency of C5 palsy. Progression of kyphotic changes, operation time and volumes of blood loss and blood transfusion were significantly greater in the SC (two- or three- level) group. Six patients in the SC group required additional surgery because of pseudoarthrosis, and four patients underwent re-operation because of adjacent level disc degeneration. -

Analysis of a Spine Registry Rate Among Smokers Undergoing
No Difference in Functional Outcome but Higher Revision Rate Among Smokers Undergoing Cervical Artificial Disc Replacement: Analysis of a Spine Registry Lee Wen-Shen, Maksim Lai Wern Sheng, William Yeo, Tan Seang Beng, Yue Wai Mun, Guo Chang Ming and Mohammad Mashfiqul Arafin Siddiqui Int J Spine Surg published online 29 December 2020 http://ijssurgery.com/content/early/2020/12/17/7140 This information is current as of October 2, 2021. Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://ijssurgery.com/alerts The International Journal of Spine Surgery 2397 Waterbury Circle, Suite 1, Aurora, IL 60504, Phone: +1-630-375-1432 © 2020 ISASS. All RightsDownloaded Reserved. from http://ijssurgery.com/ by guest on October 2, 2021 International Journal of Spine Surgery, Vol. 00, No. 00, 0000, pp. 000–000 https://doi.org/10.14444/7140 ÓInternational Society for the Advancement of Spine Surgery No Difference in Functional Outcome but Higher Revision Rate Among Smokers Undergoing Cervical Artificial Disc Replacement: Analysis of a Spine Registry LEE WEN-SHEN, MBBS (HONS),1,2 MAKSIM LAI WERN SHENG, MBBS,1 WILLIAM YEO,3 TAN SEANG BENG, MBBS, FRCS,1 YUE WAI MUN, MBBS, FRCS,1 GUO CHANG MING, MBBS, FRCS,1 MOHAMMAD MASHFIQUL ARAFIN SIDDIQUI, MBBS, FRCS1 1Department of Orthopaedic Surgery, Singapore General Hospital, Singapore 2Department of Surgery, The Alfred Hospital, Melbourne, Australia, 3Statistics and Clinical Research, Singapore General Hospital, Singapore ABSTRACT Background: Smoking is a known predictor of negative outcomes in spinal surgery. However, its effect on the functional outcomes and revision rates after ADR is not well-documented. -

Priority Health Spine and Joint Code List
Priority Health Joint Services Code List Category CPT® Code CPT® Code Description Joint Services 23000 Removal of subdeltoid calcareous deposits, open Joint Services 23020 Capsular contracture release (eg, Sever type procedure) Joint Services 23120 Claviculectomy; partial Joint Services 23130 Acromioplasty or acromionectomy, partial, with or without coracoacromial ligament release Joint Services 23410 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open; acute Joint Services 23412 Repair of ruptured musculotendinous cuff (eg, rotator cuff) open;chronic Joint Services 23415 Coracoacromial ligament release, with or without acromioplasty Joint Services 23420 Reconstruction of complete shoulder (rotator) cuff avulsion, chronic (includes acromioplasty) Joint Services 23430 Tenodesis of long tendon of biceps Joint Services 23440 Resection or transplantation of long tendon of biceps Joint Services 23450 Capsulorrhaphy, anterior; Putti-Platt procedure or Magnuson type operation Joint Services 23455 Capsulorrhaphy, anterior;with labral repair (eg, Bankart procedure) Joint Services 23460 Capsulorrhaphy, anterior, any type; with bone block Joint Services 23462 Capsulorrhaphy, anterior, any type;with coracoid process transfer Joint Services 23465 Capsulorrhaphy, glenohumeral joint, posterior, with or without bone block Joint Services 23466 Capsulorrhaphy, glenohumeral joint, any type multi-directional instability Joint Services 23470 ARTHROPLASTY, GLENOHUMERAL JOINT; HEMIARTHROPLASTY ARTHROPLASTY, GLENOHUMERAL JOINT; TOTAL SHOULDER [GLENOID