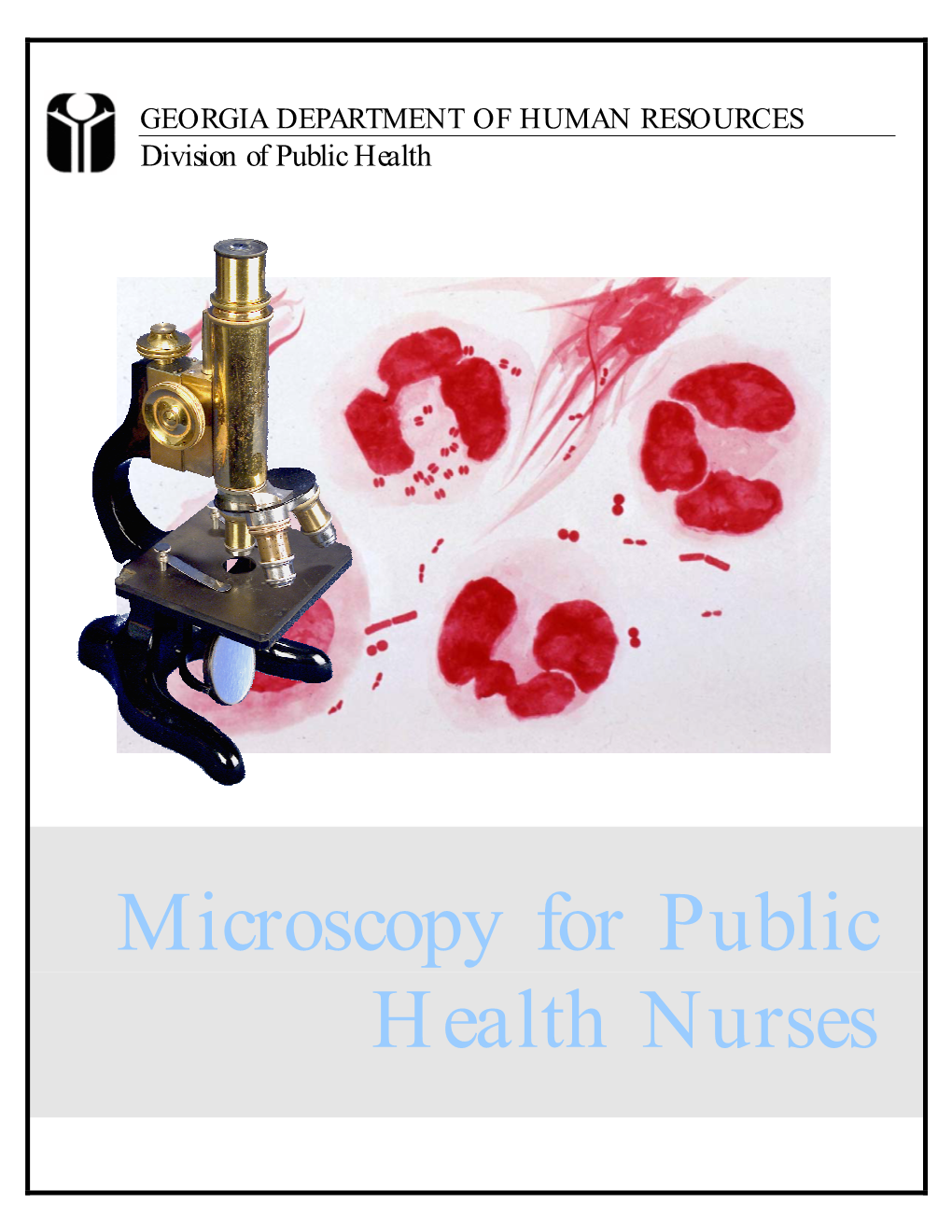
Microscopy for Public Health Nurses
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Morphology, Ultrastructure and Molecular Phylogeny of a New Freshwater Heterolobose Amoeba Parafumarolamoeba Stagnalis N. Sp
diversity Article The Morphology, Ultrastructure and Molecular Phylogeny of a New Freshwater Heterolobose Amoeba Parafumarolamoeba stagnalis n. sp. (Vahlkampfiidae; Heterolobosea) Anastasia S. Borodina 1,2, Alexander P. Mylnikov 1,†, Jan Janouškovec 3 , Patrick J. Keeling 4 and Denis V. Tikhonenkov 1,5,* 1 Papanin Institute for Biology of Inland Waters, Russian Academy of Sciences, 152742 Borok, Russia; [email protected] 2 Department of Zoology and Parasitology, Voronezh State University, Universitetskaya Ploshad 1, 394036 Voronezh, Russia 3 Centre Algatech, Laboratory of Photosynthesis, Institute of Microbiology, Czech Academy of Sciences, Opatovický Mlýn, 37981 Tˇreboˇn,Czech Republic; [email protected] 4 Department of Botany, University of British Columbia, 6270 University Boulevard, Vancouver, BC V6T1Z4, Canada; [email protected] 5 AquaBioSafe Laboratory, University of Tyumen, 625003 Tyumen, Russia * Correspondence: [email protected]; Tel.: +7-485-472-4533 † Alexander P. Mylnikov is deceased. http://zoobank.org/References/e543a49a-16c1-4b7c-afdb-0bc56b632ef0 Abstract: Heterolobose amoebae are important members of marine, freshwater, and soil microbial Citation: Borodina, A.S.; Mylnikov, communities, but their diversity remains under-explored. We studied the diversity of Vahlkampfiidae A.P.; Janouškovec, J.; Keeling, P.J.; to improve our understanding of heterolobosean relationships and their representation in aquatic Tikhonenkov, D.V. The Morphology, benthos. Using light and electron microscopy, and molecular phylogenies based on the SSU rRNA Ultrastructure and Molecular and ITS loci, we describe the fine morphology and evolutionary relationships of a new heterolobosean Phylogeny of a New Freshwater Parafumarolamoeba stagnalis n. sp. from a small pond in European Russia. Cells of P. stagnalis possess Heterolobose Amoeba a clearly distinguishable anterior hyaline pseudopodium, eruptive movement, several thin and Parafumarolamoeba stagnalis n. -

Small Wonder Acetone Vaporizer
Acetone Vaporizers and Clearing Supplies: 84-85 Microscope Slides & Cover Glass: 86-87 Sample Collection and Storage Bags: 88 Respirator Fit Test Kits: 89-91 Small Wonder Acetone Vaporizer The Wonder Makers Small Wonder Acetone Vaporizer was developed as an economical and quick way to clear asbestos PCM slides. Specifically designed to meet NIOSH 7400, 7402, or ORM requirements for preparation of PCM samples. Features: ■ Heat control and thermometer built into vaporizer unit ■ Padded carrying case protects equipment and supplies ■ Detailed instruction manual ■ Enough supplies for the analysis of 1/2 gross of slides ■ Lightweight but solidly built ■ Designed in strict compliance with the NIOSH 7400, 7402, or ORM requirements for preparation of microscope slides for PCM analysis Specifications 4-7/8” L x 4-1/2” W x 2-3/4” H (Small Wonder vaporizer) DIMENSIONS 13” L x 11” W x 4” H (Complete Analysis Kit) Plastic case, ABS plastic cover on vaporizer, clear MATERIALS plastic bottles, metal and plastic tools. 2-1/2 lbs. (Small Wonder vaporizer) WEIGHT 8 lbs. (Complete Analysis Kit) Black vaporizer cover with FINISH gray cord. Case color may vary. Complete Kit Shown Includes everything needed to clear slides for PCM analysis PRODUCT DESCRIPTION Small Wonder Analysis Kit WM-42 Includes acetone vaporizer, 1 box microscope slides, 1/2oz Triacetin, 2oz Acetone, 1 microdropper, 1 syringe, 1 scalpel, tweezers, padded carrying case and instruction manual. WM-44 Acetone reagent, 2oz, 99% pure WM-45 Triacetin reagent, 1/2oz, 99% pure WM-47 1cc Syringe WM-48 Rounded Edge Scalpel WM-49 Microdropper 81 The Professionals Choice for Air Sampling Equipment Perm-O-Fix Acetone Vaporizer A simple, easy to use, actone vaporizer for use in preparing asbestos PCM samples as per NIOSH 7400. -

Catalogue of Bacteria Shapes
We first tried to use the most general shape associated with each genus, which are often consistent across species (spp.) (first choice for shape). If there was documented species variability, either the most common species (second choice for shape) or well known species (third choice for shape) is shown. Corynebacterium: pleomorphic bacilli. Due to their snapping type of division, cells often lie in clusters resembling chinese letters (https://microbewiki.kenyon.edu/index.php/Corynebacterium) Shown is Corynebacterium diphtheriae Figure 1. Stained Corynebacterium cells. The "barred" appearance is due to the presence of polyphosphate inclusions called metachromatic granules. Note also the characteristic "Chinese-letter" arrangement of cells. (http:// textbookofbacteriology.net/diphtheria.html) Lactobacillus: Lactobacilli are rod-shaped, Gram-positive, fermentative, organotrophs. They are usually straight, although they can form spiral or coccobacillary forms under certain conditions. (https://microbewiki.kenyon.edu/index.php/ Lactobacillus) Porphyromonas: A genus of small anaerobic gram-negative nonmotile cocci and usually short rods thatproduce smooth, gray to black pigmented colonies the size of which varies with the species. (http:// medical-dictionary.thefreedictionary.com/Porphyromonas) Shown: Porphyromonas gingivalis Moraxella: Moraxella is a genus of Gram-negative bacteria in the Moraxellaceae family. It is named after the Swiss ophthalmologist Victor Morax. The organisms are short rods, coccobacilli or, as in the case of Moraxella catarrhalis, diplococci in morphology (https://en.wikipedia.org/wiki/Moraxella). *This one could be changed to a diplococcus shape because of moraxella catarrhalis, but i think the short rods are fair given the number of other moraxella with them. Jeotgalicoccus: Jeotgalicoccus is a genus of Gram-positive, facultatively anaerobic, and halotolerant to halophilicbacteria. -

Porphyromonas Gingivalis, Strain F0566 Catalog
Product Information Sheet for HM-1141 Porphyromonas gingivalis, Strain F0566 immediately upon arrival. For long-term storage, the vapor phase of a liquid nitrogen freezer is recommended. Freeze- thaw cycles should be avoided. Catalog No. HM-1141 Growth Conditions: For research use only. Not for human use. Media: Supplemented Tryptic Soy broth or equivalent Contributor: Tryptic Soy agar with 5% defibrinated sheep blood or Floyd E. Dewhirst, D.D.S., Ph.D., Senior Member of the Staff, Supplemented Tryptic Soy agar or equivalent Department of Microbiology and Jacques Izard, Assistant Incubation: Member of the Staff, Department of Molecular Genetics, The Temperature: 37°C Forsyth Institute, Cambridge, Massachusetts, USA Atmosphere: Anaerobic Propagation: Manufacturer: 1. Keep vial frozen until ready for use, then thaw. BEI Resources 2. Transfer the entire thawed aliquot into a single tube of broth. Product Description: 3. Use several drops of the suspension to inoculate an Bacteria Classification: Porphyromonadaceae, agar slant and/or plate. Porphyromonas 4. Incubate the tube, slant and/or plate at 37°C for 24 to Species: Porphyromonas gingivalis 72 hours. Broth cultures should include shaking. Strain: F0566 Original Source: Porphyromonas gingivalis (P. gingivalis), Citation: strain F0566 was isolated in October 1987 from the tooth Acknowledgment for publications should read “The following of a patient diagnosed with moderate periodontitis in the reagent was obtained through BEI Resources, NIAID, NIH as United States.1 part of the Human Microbiome Project: Porphyromonas Comments: P. gingivalis, strain F0566 (HMP ID 1989) is a gingivalis, Strain F0566, HM-1141.” reference genome for The Human Microbiome Project (HMP). HMP is an initiative to identify and characterize Biosafety Level: 2 human microbial flora. -

Using Microscopes
Using Microscopes Grade Level: 6, 7, 8, 9, 10 Duration: 30-45 minutes Classification: Classroom Subject(s): Biology, Microbiology Categories (STEM): Science, Technology Keywords: Staining, Microscopes, Microbes Introduction ● Summary: Students will learn how to properly use microscopes and view different cells and organisms. ● Description: Microscopes are often used to view different types of organisms, cells, and organelles. Microscopes can be used to visualize changes in cell structure and identify unknown organisms. Students will learn all the parts of microscopes and how to use and adjust them. Another important step of using microscopes is to learn how to properly prepare slides and wet mounts. Different organisms, cells, and organelles will be viewed under a microscope. In case of school policy limitations, note that student role models are required to cut vegetables at schools before the visit starts. *Note - School is responsible for providing microscopes for this activity. Online Resources: https://www.youtube.com/watch?v=SUo2fHZaZCU\ Vocabulary Organisms: an individual animal, plant, or single-celled life form Cell: smallest structural unit of an organism Organelle: organized structures (compartments) within a living cell Nucleus: dense organelle (generally in the middle of a cell) that contains genetic information Wet Mount: microscope slide holding a specimen suspended in a drop of liquid Materials Materials Quantity Reusable? Nail Polish 1 red per classroom Yes Microscopes (provided by school) TBD by school Yes Dirty -

Introduction to Bacteriology and Bacterial Structure/Function
INTRODUCTION TO BACTERIOLOGY AND BACTERIAL STRUCTURE/FUNCTION LEARNING OBJECTIVES To describe historical landmarks of medical microbiology To describe Koch’s Postulates To describe the characteristic structures and chemical nature of cellular constituents that distinguish eukaryotic and prokaryotic cells To describe chemical, structural, and functional components of the bacterial cytoplasmic and outer membranes, cell wall and surface appendages To name the general structures, and polymers that make up bacterial cell walls To explain the differences between gram negative and gram positive cells To describe the chemical composition, function and serological classification as H antigen of bacterial flagella and how they differ from flagella of eucaryotic cells To describe the chemical composition and function of pili To explain the unique chemical composition of bacterial spores To list medically relevant bacteria that form spores To explain the function of spores in terms of chemical and heat resistance To describe characteristics of different types of membrane transport To describe the exact cellular location and serological classification as O antigen of Lipopolysaccharide (LPS) To explain how the structure of LPS confers antigenic specificity and toxicity To describe the exact cellular location of Lipid A To explain the term endotoxin in terms of its chemical composition and location in bacterial cells INTRODUCTION TO BACTERIOLOGY 1. Two main threads in the history of bacteriology: 1) the natural history of bacteria and 2) the contagious nature of infectious diseases, were united in the latter half of the 19th century. During that period many of the bacteria that cause human disease were identified and characterized. 2. Individual bacteria were first observed microscopically by Antony van Leeuwenhoek at the end of the 17th century. -
Handheld Microscope Users Guide
Handheld Microscope Users Guide www.ScopeCurriculum.com ii Handheld Microscope Users Guide Hand-Held Microscope User’s Guide Table of Contents INTRODUCTION ..................................................................................................................................1 What is a Scope-On-A-Rope? .....................................................................................................1 Which model do you have?.........................................................................................................2 Analog vs. Digital .........................................................................................................................3 Where can I buy a SOAR? ...........................................................................................................3 NEW SCOPE-ON-A-ROPE..................................................................................................................4 Parts and Assembly of SOAR .....................................................................................................4 Connections .................................................................................................................................5 Turning It On.................................................................................................................................5 Comparing and Installing Lenses...............................................................................................6 How to Use and Capture Images with the 30X Lens.................................................................7 -
Microscope Slide-Making Kit
Microscope Slide-Making Kit 665 Carbon Street, Billings, MT 59102 Phone: 800.860.6272 Fax: 888.860.2344 www.homesciencetools.com Copyright 2005 by Home Training Tools, Ltd. All rights reserved. Viewing Slides Scan a slide at low power (usually 40X) to get an overview of the specimen. Center the part of the specimen you want to view at higher power. Adjust your lighting until the slide specimen has clear, sharp contrast. Then switch to medium power (usually 100X) and refocus to observe tissue and cell variations. Repeat at high power (usually 400X). Making Your Own Slides Whole Mounts: Whole mounts are made by placing small objects or specimens whole on a blank slide and then covering them with a coverslip. If your specimen is thick, a concavity slide will work better. You can make whole mounts of many things. Here are some ideas: Colored thread Feather (piece) Thin plant leaf Print (letters) Cloth fibers Hair strand Small insects Dust Algae Pond water Thin paper Insect parts Whole mount specimens must be thin enough to allow light to pass through them. Do not use large, hard objects like rocks, as they can break your slides and microscope lenses. Sections: Section mounts are made by slicing a very thin section of specimen. A cross section is made by slicing across the width or diameter of the specimen. A longitudinal section is made by slicing across the length of the specimen. It is difficult to make sections thin enough without an instrument called a microtome. You can make a simple microtome with a thread spool, a 1/4” diameter bolt at least 2” long, and a 1/4” nut. -

Laboratory Exercises in Microbiology: Discovering the Unseen World Through Hands-On Investigation
City University of New York (CUNY) CUNY Academic Works Open Educational Resources Queensborough Community College 2016 Laboratory Exercises in Microbiology: Discovering the Unseen World Through Hands-On Investigation Joan Petersen CUNY Queensborough Community College Susan McLaughlin CUNY Queensborough Community College How does access to this work benefit ou?y Let us know! More information about this work at: https://academicworks.cuny.edu/qb_oers/16 Discover additional works at: https://academicworks.cuny.edu This work is made publicly available by the City University of New York (CUNY). Contact: [email protected] Laboratory Exercises in Microbiology: Discovering the Unseen World through Hands-On Investigation By Dr. Susan McLaughlin & Dr. Joan Petersen Queensborough Community College Laboratory Exercises in Microbiology: Discovering the Unseen World through Hands-On Investigation Table of Contents Preface………………………………………………………………………………………i Acknowledgments…………………………………………………………………………..ii Microbiology Lab Safety Instructions…………………………………………………...... iii Lab 1. Introduction to Microscopy and Diversity of Cell Types……………………......... 1 Lab 2. Introduction to Aseptic Techniques and Growth Media………………………...... 19 Lab 3. Preparation of Bacterial Smears and Introduction to Staining…………………...... 37 Lab 4. Acid fast and Endospore Staining……………………………………………......... 49 Lab 5. Metabolic Activities of Bacteria…………………………………………….…....... 59 Lab 6. Dichotomous Keys……………………………………………………………......... 77 Lab 7. The Effect of Physical Factors on Microbial Growth……………………………... 85 Lab 8. Chemical Control of Microbial Growth—Disinfectants and Antibiotics…………. 99 Lab 9. The Microbiology of Milk and Food………………………………………………. 111 Lab 10. The Eukaryotes………………………………………………………………........ 123 Lab 11. Clinical Microbiology I; Anaerobic pathogens; Vectors of Infectious Disease….. 141 Lab 12. Clinical Microbiology II—Immunology and the Biolog System………………… 153 Lab 13. Putting it all Together: Case Studies in Microbiology…………………………… 163 Appendix I. -

An Antique Microscope Slide Brings the Thrill of Discovery Into a Contemporary Biology Classroom
ARTICLE An Antique Microscope Slide Brings the Thrill of Discovery into a Contemporary Biology Classroom FRANK REISER ABSTRACT that few others share my interests), I add them to my growing collection. The discovery of a Victorian-era microscope slide titled “Grouped Flower Seeds” began When I found skillfully prepared Victorian-era microscope slides listed an investigation into the scientific and historical background of the antique slide to under the category “Folk Art” in an antique dealer’s online catalog, it led develop its usefulness as a multidisciplinary tool for PowerPoint presentations usable in not only to my acquiring them but also to the beginning of a journey contemporary biology classrooms, particularly large-enrollment sections. The resultant involving Internet and library research, trips to herbaria, field collecting presentation was intended to engage students in discussing historical and contempo- excursions, and, finally, to the development of a PowerPoint lecture for rary biology education, as well as some of the intricacies of seed biology. Comparisons between the usefulness and scope of various seed identification resources, both online community college biology students. The slide that triggered the snow- and in print, were made. balling project is titled “Grouped Flower Seeds” (Figure 1). Having spent most of my life as a biology educator, I view most of Key Words: Grouped Flower Seeds; Watson and Sons; antique microscope slide; what I encounter in life from a science-oriented perspective. Finding pre- online seed identification resources; seed identification manuals; seed biology; pared microscope slides described as “folk art” sharply conflicted with large-enrollment lecture. my sense of the correct order of disciplines – particularly for items that I would reverently classify as the tools of scientists. -

Laboratory Manual for Diagnosis of Sexually Transmitted And
Department of AIDS Control LaborLaboraattororyy ManualManual fforor DiagnosisDiagnosis ofof SeSexxuallyually TTrransmitansmittteded andand RRepreproductivoductivee TTrractact InInffectionsections FOREWORD Sexually Transmitted Infections (STIs) and Reproductive Tract Infections (RTIs) are diseases of major global concern. About 6% of Indian population is reported to be having STIs. In addition to having high levels of morbidity, they also facilitate transmission of HIV infection. Thus control of STIs goes hand in hand with control of HIV/AIDS. Countrywide strengthening of laboratories by helping them to adopt uniform standardized protocols is very important not only for case detection and treatment, but also to have reliable epidemiological information which will help in evaluation and monitoring of control efforts. It is also essential to have good referral services between primary level of health facilities and higher levels. This manual aims to bring in standard testing practices among laboratories that serve health facilities involved in managing STIs and RTIs. While generic procedures such as staining, microscopy and culture have been dealt with in detail, procedures that employ specific manufacturer defined kits have been left to the laboratories to follow the respective protocols. An introduction to quality system essentials and quality control principles has also been included in the manual to sensitize the readers on the importance of quality assurance and quality management system, which is very much the need of the hour. Manual of Operating Procedures for Diagnosis of STIs/RTIs i PREFACE Sexually Transmitted Infections (STIs) are the most common infectious diseases worldwide, with over 350 million new cases occurring each year, and have far-reaching health, social, and economic consequences. -

Can Protozoa Prove the Beginning of the World?
Southeastern University FireScholars Classical Conversations Spring 2020 Can Protozoa Prove the Beginning of the World? Karina L. Burton Southeastern University - Lakeland, [email protected] Follow this and additional works at: https://firescholars.seu.edu/ccplus Part of the Cell Biology Commons, and the Evolution Commons Recommended Citation Burton, Karina L., "Can Protozoa Prove the Beginning of the World?" (2020). Classical Conversations. 9. https://firescholars.seu.edu/ccplus/9 This Term Paper is brought to you for free and open access by FireScholars. It has been accepted for inclusion in Classical Conversations by an authorized administrator of FireScholars. For more information, please contact [email protected]. 1 Can Protozoa Prove the Beginning of the World? Karina L. Burton Classical Conversations: Challenge 4; Southeastern University ENGL 1233: English Composition II Grace Veach April 16, 2020 2 Abstract Protozoa are magnificent creatures. They exhibit all of the functions intrinsic to living organisms: irritability, metabolism, growth and reproduction. Within these functions, there are numerous examples of mutations that occur in order for organisms to adapt to their given environments. Irritability is demonstrated in protozoa by their use of pseudopodia, flagella, or cilia for motility; it has been shown that such locomotors exhibit diversity while maintaining similar protein and chemical structures that appear to be a result of evolutionary processes. Metabolism in protozoa is similar to that of larger animals, but their diet is unique. They primarily feast upon bacteria, which have begun mutating to evade easy ingestion and digestion by protozoa, therefore increasing their survival rate and making it necessary for protozoa to adapt.