Obesity Guide Englis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
![[Gamlath G.R.R.S. Et Al : a Survey on Usage of Kola Kanda (Herbal Gruel) Among Sri Lankan Population]](https://docslib.b-cdn.net/cover/8566/gamlath-g-r-r-s-et-al-a-survey-on-usage-of-kola-kanda-herbal-gruel-among-sri-lankan-population-1588566.webp)
[Gamlath G.R.R.S. Et Al : a Survey on Usage of Kola Kanda (Herbal Gruel) Among Sri Lankan Population]
International Journal of Applied Ayurved Research ISSN: 2347- 6362 A SURVEY ON USAGE OF KOLA KANDA (HERBAL GRUEL) AMONG SRI LANKAN POPULATION Gamlath G.R.R.S.1, Waratenne P. R.2 1BAMS Scholar (Final year) Institute of Indigenous Medicine, University of Colombo, Rajagiriya, Sri Lanka. 2Senior Lecturer, Institute of Indigenous Medicine, University of Colombo, Rajagiriya, Sri Lanka. ABSTRACT The Charaka Samhita has mentioned the three pillars of life, i.e. Ahara (Food), Nidra (Sleep) & Brahmacharya (observance of celibacy). Among these, food is a major supporting pillar which helps in sustenance of life and maintenance of health. Malnutrition is the most prevalent disease due to lack of having proper food. Malnutrition is a major health problem in Sri Lanka. To overcome the malnutrition a lots of nutritious and profitable food supplements can be implemented. Among them Kola kanda (herbal gruel) is a most profitable breakfast. The study was aimed to survey on usage of Kola kanda among Sri Lankan population. Data collected by using convenience sampling from randomly selected ten participants from each province of Sri Lanka, by a questionnaire in Sinhala or Tamil. Questionnaire was filled by the participants. The juice of edible leaves is the very specific ingredient in Kola kanda which are rich in vitamins and minerals. Hence they are very essential for human body as micro nutrition; a glass of Kola kanda fulfills that requirement easily. The other ingredients; i.e. grains and coconut milk in Kola kanda are very rich in carbohydrates, proteins and fats. The calories includes in ingredients of Kola kanda, it is obvious that one glass of Kola kanda contains enough calories as a breakfast. -

Experiences and Understandings of a Group of Sri Lankan Migrants in Australia with Type Two Diabetes
Controlling Diabetes or Keeping Life under Control? Experiences and Understandings of a Group of Sri Lankan Migrants in Australia with Type Two Diabetes Submitted in total fulfilment of the requirements of the degree of Doctor of Philosophy March Two Thousand and Fourteen Prabhathi Basnayake Ralalage Centre for Health and Society University of Melbourne Thesis Abstract Diabetes is a key public health priority and a major health concern for many migrant communities including the Sri Lankan community here in Australia. Understanding people’s comprehensions of the disease and its management is essential to successfully address any related issues in order to avoid premature deaths and high public health costs. According to many health reports published over the past years Sri Lankan migrants have been identified as having a significantly higher prevalence of type two diabetes in Australia compared to the general Australian population. This ethnography revolves around a group of first generation Sri Lankan migrants with type two diabetes in Australia. This thesis relates their story of encountering and dealing with difficulties and complexities of migrant life while having to build a ‘successful’ life in Australia and also having to concurrently manage a chronic illness. While arguing that understanding of diabetes management cannot be just reduced or confined to level of compliance to medical advice and blood sugar measurement readings on the glucometer, I point out in the research that the stories of Sri Lankans with diabetes in a developed country are different to the stories of other South Asian migrants with diabetes living elsewhere in the world as examined in other studies. -

Download (4MB)
Kamus M elayu Makasar-Indonesia Oleh Aburaerah Arief Abdul Muthalib Abdul Kadar Mulya P ER PU STAKAAN Zainuddjn Hakim PUS.T PEMBINAAN DAN FENGEMBJNGA BAHSA DEPMUEMEM pNDO1KAN OAr'.I KEBUDAVAA4 Pusat Pembinaan dan Pengembangan Bahasa Departemen Pendidikan dan Kebudayaan Jakarta 1985 Hak Cipta pada Departemen Pendidikan dan Kebudayaan Pusat Pembiflaafl an Pencembaflt8a erpustaka Induk: Penyunting KaíI1 .1qq. A'( Hariyanti 33 TgL kf-f Ttd. 'IL Seri: K-85.028 Cetakan Pertama Naskah buku mi, yang semula merupakan hasil Proyek Pengembanan Bahasa dan Sastra Indonesia dan Daerah tahun 1981/1982, diterbitkan dengan danE Proyek Pengembangan Bahasa dan Sastra Indonesia. Staf Intl Proyek Drs. Tony S. Rachmadie (Pemimpin), Samidjo (Bendaharawan), Drs. S.R.H. Sitanggang (Sekretaris), Drs. S. Amran Tasai, Drs. A. Patoni, Dra. Siti Zahra YundiafI, dan Drs. E. Zainal Arifm (Asisten). Sebagian atau seluruh isi buku irii dilãrang diperbanyak dalarn bentuk apa pun tanpa izin tertulis dari penerbit, kecuali dalam hal kutipan untuk keperluan penulisan artikel'atau kanangan ilmiáh. Alamat Penerbit Pusat Pembinaan dan Pengembangan Bahasa Jalan Daksinapati Barat IV, Rawamangun Jakarta 13220 PRAKATA Sejak Rencana Pembangunan Jima Tahun 11(1974), telah digariskan kebijakan .pembinaan dan pengembangan kebudayaan nasional dalam berba- gai seginya: Dalam garis haluan mi, masalah kebahasaan dan kesastraan me- rupakan salah satu masalah kebudayaan nasional yang perlu digarap dengan sungguh-sungguh dan, berencana sehingga tujuan akhir pembinaan dan pe- ngembangan bahasa Indonesia dan daerah, termasuk sastranya, dapat terca- pai. Tujuaii aithir pembinaan dan pengembangan itu, antara lain, adalah me- ningkatkn mutu kemampuan menggunakan bahasa Indonesia sebagai sarana koniunikasi nasional, sebagaimana digariskan dalam Garis-Garis Besar Ha- luan Negara. -

Inroom Dining Menu Revise
BREAKFAST FILLET OF FISH WITH BLACK BEAN SAUCE 1,100 With green and red pepper, bamboo shoots 6 10 ALL DAY & onions in black bean sauce {am/am { SWEET & SOUR DEEP FRIED PORK 950 STARTERS & SALADS In sweet and sour sauce served with egg fried rice CONTINENTAL 1,600 AVOCADO, PRAWN & LOBSTER SALAD 900 CHICKEN WITH CASHEW NUTS 950 With poached apple & shaved parmesan CHOICE OF FRESHLY SQUEEZED JUICES (V) FRUITS & CEREALS Toss-fried in special plum sauce & cashew nuts Orange, lemon, pineapple, mango, watermelon, served with egg fried rice FRESHLY SQUEEZED FRUIT JUICES (V) 650 CHOP CHOP SALAD 800 passion fruit Orange, mango, pineapple, papaya, French greens, roast chicken, cheddar cheese, red onions, mandarin & garlic croutons HOME BAKED BAKERY BASKET (V) strawberry, carrot, apple Croissant, danish pastry, raisin roll, FRESHLY MADE FRUIT SMOOTHIES 650 GREEN SALAD (V) 550 brown or white toast Green beans, cucumber, spring onions, SOUPS Banana, strawberry, mango Corn & fish chowder with garlic croutons 650 black & green olives, asparagus & potatoes YOUR CHOICE OF 2 FRESH EGGS FRESH YOGURT (V) 400 Lobster & crab bisque with cheese toast 800 Omelet, scrambled, poached, Blueberry, strawberry, vanilla, chocolate CLASSIC SEAFOOD COCKTAIL 750 Cream of mushroom with garlic toast 750 over easy or hard-boiled Served with spicy mayo & garlic toast Soup of the day 750 SEASONAL FRUIT PLATTER 750 Freshly brewed regular or decaffeinated coffee, TANDOORI CHICKEN SALAD 750 selection of fine teas, milk or hot chocolate HOMEMADE GRANOLA WITH BERRIES 700 With crisp -

Sri Lanka a SPICY DESTINATION
Sri Lanka A SPICY DESTINATION By Margaret Swaine Wholesome, healthy and packed with bold flavours, Sri Lankan food benefits both the body and your taste buds. The food is what I remember and miss the most During our stay at Serene Pavilions fish, fresh fish and bags of produce. On about Sri Lanka. The country has an abundance (serenepavilions.com), a beautiful oceanside the way back to the hotel, we stopped at a of all the things I love to eat: spices, curries, property near Wadduwa on the southwest roadside stand selling live lagoon crabs and seafood and fresh produce. Some of the spices, coast, we went with chef Ruwan Chandana added these to our purchases. At the hotel, such as the real cinnamon, are special to the to the local market. We were thrilled at the chef Ruwan cooked up what seemed like a island. As for the curries, you can have them at incredible array of fruits and vegetables, miniature banquet for my husband and I. It breakfast, lunch and dinner. And my husband many of which we had not seen or eaten was a spectacular meal and unlike any we and I did. before. Among the tropical fruits were diul had experienced elsewhere in the world. We (wood apple), annona (soursop), bael fruit, soon found it was also typical of the meals This small Indian Ocean island in the Bay durian, goraka, Ceylon oak, tamarind and we could enjoy while touring the country. of Bengal just below the southeastern tip multiple varieties of bananas. Vegetables of India was undergoing a huge surge in included bitter gourd, snake gourd, breadfruit, Basic rice and curry is an ubiquitous dish tourism when it was hard hit by the Easter tapioca root, grape sized thibbatu melon served up island wide. -
Justin P. Moore
SAMPLE Justin P. Moore About this Cookbook...................................................................................................................................9 Adventures in SRI LANKA ........................................................................................................................11 In the Kitchen ...............................................................................................................................................20 Lucky 13 Roasted Curry Powder original spice mix ...................................................................................23 Homemade Coconut Milk how to make & use ...........................................................................................24 SALADS & SAUCES .......................................................................................................................................25 Wild Greens with mango ginger dressing ....................................................................................................27 Pearly’s Mixed Salad with carrots, radish & coconut ..................................................................................29 Hikkaduwa Sunset Salad with pineapple, basil, lime, cucumber & cashews ............................................31 Amba Salad with mango, tomato & cucumber ............................................................................................33 Pol Sambol red-hot coconut topping ............................................................................................................35 -

Breakfast Menu Ceylon Tea and Coffee We Offer a Selection of Teas; Fresh Ceylon Teas, Green Tea, Mint and More
WHAT’S ON MENU @ BUONA VISTA HEIGHTS Breakfast Menu Ceylon Tea and Coffee We offer a selection of teas; fresh Ceylon teas, green tea, mint and more. We serve freshly ground local coffee, Italian cafetière can be provided upon request. To start the day with § Seasonal fruit plate § Buffalo curd with kittul treacle § Toasted bread and jam selection § Choice of cereal Cooked Western § Eggs any style – Fried/poached/scrambled/boiled/omelette § Add sausage, mushrooms, baked beans, grilled tomato Cooked Sri Lankan § Kola Kanda – A traditional Sri Lankan herbal gruel § Coconut rotti (ෙපා$ ෙරා) served with coconut sambol or katta sambol, dahl curry and chicken curry § Traditional milk rice (() බ) with katta sambol and coconut fish curry. § Hoppers (ආප) – A local favourite – bowl shaped thin pancakes made from rice and flour and coconut milk, either plain or with egg, served chicken curry and seeni sambol Main Menus (For Lunch and Dinner) § Traditional Sri Lankan rice and curry A spread of vegetable curries for the family to share, speak to the chef who will prepare your favourites along with fish, chicken or prawn curry, mango chutney and papa dam. § Catch of the day The chef will make his daily visit to the fish market to collect the days catch, select from fresh fish, prawns, jumbo prawns, calamari and more depending on the market. Your choice will be cooked to your liking with garlic butter or lemon sauce, potato wedges and garden salad. § Grilled chicken served with garlic rice and buttered vegetables § Plain and egg paratha served with coconut sambol, chicken or fish curry and dahl § Indonesian nasi goreng with chicken satay, cucumber salad and fried egg § String hoppers with coconut mallum, potato curry and coconut fish curry § Pasta and spaghetti – cooked to your taste with tomato, cheese or pesto sauce, add chicken or seafood and parmesan cheese. -

Anantara Tangalle Resort Brea
BREAKFAST À LA CARTE Eye-opener of the day served on the table FRESH CUT FRUIT SELECTIONS Papaya, Pineapple, Watermelon, Banana, Passion fruit, Guava FRESH JUICE SELECTIONS Watermelon, papaya, pineapple, passionfruit, lime, mango, mix fruit BAKERY SELECTIONS BREAD White toast/ brown toast/ soft rolls/ craftkorn wood fire bread (roast pan)/ viyan roll/ fish bun/ jam bread PASTRIES Danish pastry of the day/ chocolate croissants/ plain croissants/ chocolate muffin/ vanilla muffin Served with homemade jam and butter À LA CARTE SPECIALS EGGS BENEDICT Poached eggs with crispy pork bacon and hollandaise sauce on a toasted homemade muffin EGG SELECTIONS Scrambled egg/ fried egg / poached egg/ boiled egg Or mixed omelette (tomato, onion, chilli, mushroom, bell pepper) Select your preferred accompaniment: crispy pork bacon, baked beans, chicken sausage, pork sausage, sautéed mushroom, hash brown, grilled tomato OATMEAL PORRIDGE Rolled oats cooked in low-fat milk, almonds, banana, dry fruits and honey BIRCHER MUESLI Rolled oats soaked overnight in low-fat milk, mixed nuts, seeds, dry fruits, green apple and yoghurt BUTTERMILK PANCAKES With palm treacle, berry compote, whipped cream and Nutella OLD FASHIONED WAFFLES With palm treacle, berry compote, whipped cream and Nutella YOGHURTS Selection of traditional local buffalo curd, fruit or plain yoghurt CEREAL Cornflakes, all-bran, muesli, rice crispies or chocos Served with low-fat, full cream or soy milk CHEESE SELECTION Cheddar cheese, emmental cheese, brie cheese, camembert cheese, feta cheese SRI LANKAN -

Final) Villa Republic Bentota Menu (Editable) (Page in Order
MENU www.villarepublic.com VILLA REPUBLIC BENTOTA RELAX.EXPLORE.DISCOVER BREAKFAST ALL DAY SRI LANKAN SRI LANKAN SET MENU 01 King coconut water Steamed rice (red or white) Tropical fruit platter Curry: chicken | pork | beef | fish | prawn | crab | vegetable Kola kanda (V) Tempered dhal or potato Mallum (local greens) Milk rice or string hopper or pol roti served with chicken or fish or Sri Lankan salad (V) beef curry accompanied with dhal curry, pol sambol, katta sambol Pol sambol and papadam and kade pan (local bread) Curd and treacle SET MENU 02 Vegetable fried rice or yellow steamed rice Tea / cofee Devilled chicken | beef | pork | prawn WESTERN Stir-fried vegetables in black bean sauce King coconut water Green salad (V) Tropical fruit platter Stir-fried kankung with garlic Choice of cereal with fresh milk Pol Sambol and papadam Two eggs (as you like them) on toast served with avocado and sausages (pork or chicken) PASTA AND RICE Granola and yoghurt PASTA CARBONARA Tea / cofee Eggs, parmesan, smoky bacon and lots of black pepper — a Roman classic. DRINKS PASTA WITH BOLOGNESE SAUCE FRESH JUICES Homemade bolognese sauce with a choice of chicken or minced beef Orange SAUTÉED GARLIC PASTA (V) Mango The all-time classic pasta dish with a drizzle of olive oil Papaya Avocado PENNE ARRABBIATA (V) Watermelon Penne in fresh tomato sauce and olives, sprinkled with parmesan. Mixed fruit Chicken (optional) King coconut PENNE WITH WHITE SAUCE (V) Lime and soda Penne in cream sauce, sprinkled with parmesan, cheese and parsley MILK SHAKE NASI GORENG -
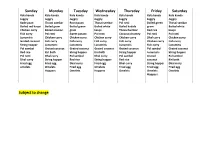
Breakfast Menu
Sunday Monday Tuesday Wednesday Thursday Friday Saturday Kola kanda Kola kanda Kola kanda Kola kanda Kola kanda Kola kanda Kola kanda Juggry Juggry Juggry Juggry Juggry Juggry Juggry Kade paan Thosai sambar Roast paan Thosai sambar Pol rotti Boiled green Thosai sambar Boiled red kaupi Boiled gram Boiled green Boiled white Boiled kadala gram Boiled white Chicken curry Boiled manioc gram kaupi Thosai Sambar Red rice kaupi Fish curry Pol rotti Sweet potato Pol rotti Coconut chutney Pol rotti Pol rotti Lunumiris Chicken curry Chicken curry Chicken curry Chicken curry Dhal curry Chicken curry Grated coconut Fish curry Fish curry Fish curry Fish curry Chicken curry Fish curry String hopper Lunumiris Lunumiris Lunumiris Lunumiris Fish curry Lunumiris Pol sambol Grated coconut Grated coconut Grated coconut Grated coconut Pol sambol Grated coconut Red rice Kiri bath String hopper Kiri bath String hopper Lunumiris String hopper Pol rotti Dhal curry Pol sambol Dhal curry Pol sambol Grated Pol sambol Dhal curry String hopper Red rice String hopper Red rice coconut Kiri bath Fried egg Fried egg Dhal curry Fried egg Dhal curry String hopper Dhal curry omelets Omelets Fried egg Omelets Fried egg Fried egg Fried egg Hoppers Omelets Hoppers Omelets Omelets Omelets Hoppers Subject to change . -
Wonder Hotel’S Brand Name at Any Event
TERMS AND CONDITIONS 1. The patients signing this form and accepting these terms and conditions shall be deemed to have signed and accepted the same for and on behalf of those persons whose names are listed in this form. 2. The hotel and Hospital strictly advices against keeping valuables in the guest room, neither the hotel nor Hospital shall not be held liable for loss of such items. 3. Consumption of liquor and smoking is strictly prohibited during the stay at hotel premises. 4. Loitering outside the room is strictly prohibited under any circumstance, in case if a patient requires assistance, they should contact the nurse station through intercom by dialing the given number for the respective floor or mobile number. 5. In no event either hotel or hospital will be liable for indirect, unforeseen consequential damages, future loss of profits or loss of revenues arising from any loss/damage suffered by the guest. 6. The guest is responsible for any loss or damage to hotel property owing or attributable to any act or omission of the guest and shall be held personally liable for such charges incurred during their stay and such damage or loss shall be charged to guest’s account as a liability for guests to be paid before discharge. 7. The room keys will not be handed over to the guest patient and the guest patient shall not lock his/her room under any circumstance during his/her stay at hotel. 8. Complaints and suggestions must be notified to the nurse station or coordinating officer in charge and cannot be published on social media to tarnish Nawaloka Hospital’s brand name or wonder Hotel’s brand name at any event. -
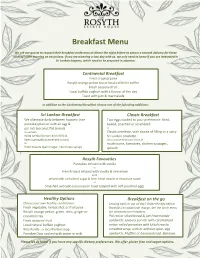
Breakfast Menu
Breakfast Menu We ask our guests to request their breakfast preference at dinner the night before to ensure a smooth delivery for those rushing in the morning on excursions. If you are planning a lazy day with us, we only need to know if you are interested in Sri Lankan hoppers, which need to be prepared in advance. Continental Breakfast Fresh tropical juice Rosyth orange pekoe tea or local cafetière coffee Fresh seasonal fruit Local buffalo yoghurt with a flavour of the day Toast with jam & marmalade In addition to the Continental Breakfast choose one of the following additions: Sri Lankan Breakfast Classic Breakfast We alternate daily between hoppers (rice Two eggs cooked to your preference: fried, pancake) plain or with an egg & boiled, poached or scrambled or pol roti (coconut flat bread) Served with Classic omelette, with choice of filling or a spicy Katta sambal (onion and chilli) & Sri Lankan omelette Seeni sambal (caramelised onion) All accompanied by your choice of Or mushrooms, tomatoes, chicken sausages, Kittul treacle (palm sugar, like maple syrup) spinach Rosyth Favourites Pancakes infused with vanilla or French toast infused with vanilla & cinnamon both served with a choice of sugar & lime, kittul treacle or chocolate sauce or Smashed avocado (seasonal) on toast topped with soft poached eggs Healthy Options Breakfast on the go Choose your own healthy combination: Leaving early or out all day? Order the day before. Fresh vegetable, herbal shot or fruit juice Breakfast no additional charge. See the lunch menu Rosyth orange pekoe, green, mint, ginger or for takeaway lunch options. cinnamon tea Pol roti or sliced bread & jam/marmalade Fresh seasonal fruit sandwich; savoury pol roti with caramelised Local natural buffalo yoghurt onion; rolled pancakes with kittul treacle; Kola Kanda - a local herbal soup omelette wrap, with or without spice; egg Porridge Oats cooked with water or milk sandwich.