White Blood Cells (Wbcs)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Adaptive Tdetect Fact Sheet for Recipient
FACT SHEET FOR RECIPIENTS Coronavirus Adaptive Biotechnologies Corporation September 2, 2021 Disease 2019 T-Detect COVID Test (COVID-19) You are being given this Fact Sheet because your coughing, difficulty breathing, etc.). A full list of sample is being tested or was tested for an adaptive T- symptoms of COVID-19 can be found at the following cell immune response to the virus that causes link: https://www.cdc.gov/coronavirus/2019- Coronavirus Disease 2019 (COVID-19) using the T- ncov/symptoms-testing/symptoms.html. Detect COVID Test. How are people tested for COVID-19? Two main kinds of tests are currently available for You should not interpret the results of this COVID-19: diagnostic tests and adaptive immune response tests. test to indicate the presence or absence of immunity or protection from COVID-19 • A diagnostic test tells you if you have a current infection. infection. • An adaptive immune response test tells you if you may have had a previous infection This Fact Sheet contains information to help you understand the risks and benefits of using this test to What is the T-Detect COVID Test? evaluate your adaptive immune response to SARS-CoV- This test is similar to an antibody test in that it measures 2, the virus that causes COVID-19. After reading this your adaptive immune response to SARS-CoV-2, the Fact Sheet, if you have questions or would like to virus that causes COVID-19. However in this case it discuss the information provided, please talk to your specifically measures your adaptive T-cell immune healthcare provider. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Defining Natural Antibodies
PERSPECTIVE published: 26 July 2017 doi: 10.3389/fimmu.2017.00872 Defining Natural Antibodies Nichol E. Holodick1*, Nely Rodríguez-Zhurbenko2 and Ana María Hernández2* 1 Department of Biomedical Sciences, Center for Immunobiology, Western Michigan University Homer Stryker M.D. School of Medicine, Kalamazoo, MI, United States, 2 Natural Antibodies Group, Tumor Immunology Division, Center of Molecular Immunology, Havana, Cuba The traditional definition of natural antibodies (NAbs) states that these antibodies are present prior to the body encountering cognate antigen, providing a first line of defense against infection thereby, allowing time for a specific antibody response to be mounted. The literature has a seemingly common definition of NAbs; however, as our knowledge of antibodies and B cells is refined, re-evaluation of the common definition of NAbs may be required. Defining NAbs becomes important as the function of NAb production is used to define B cell subsets (1) and as these important molecules are shown to play numerous roles in the immune system (Figure 1). Herein, we aim to briefly summarize our current knowledge of NAbs in the context of initiating a discussion within the field of how such an important and multifaceted group of molecules should be defined. Edited by: Keywords: natural antibody, antibodies, natural antibody repertoire, B-1 cells, B cell subsets, B cells Harry W. Schroeder, University of Alabama at Birmingham, United States NATURAL ANTIBODY (NAb) PRODUCING CELLS Reviewed by: Andre M. Vale, Both murine and human NAbs have been discussed in detail since the late 1960s (2, 3); however, Federal University of Rio cells producing NAbs were not identified until 1983 in the murine system (4, 5). -

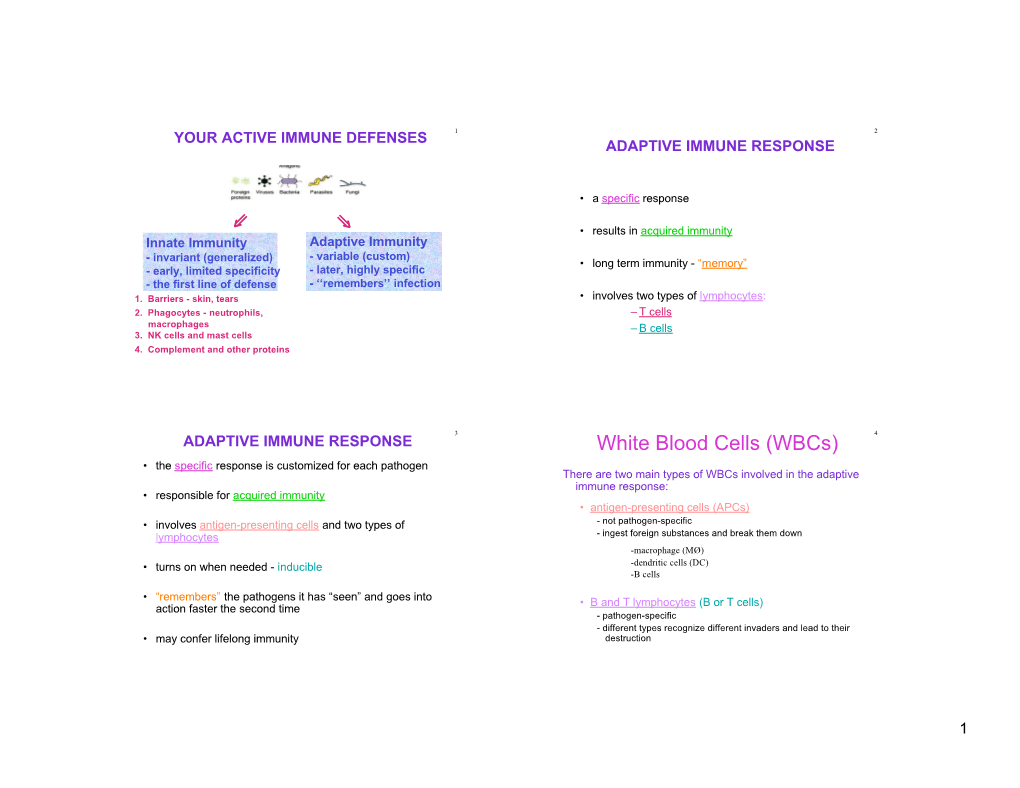
Adaptive Immune Systems
Immunology 101 (for the Non-Immunologist) Abhinav Deol, MD Assistant Professor of Oncology Wayne State University/ Karmanos Cancer Institute, Detroit MI Presentation originally prepared and presented by Stephen Shiao MD, PhD Department of Radiation Oncology Cedars-Sinai Medical Center Disclosures Bristol-Myers Squibb – Contracted Research What is the immune system? A network of proteins, cells, tissues and organs all coordinated for one purpose: to defend one organism from another It is an infinitely adaptable system to combat the complex and endless variety of pathogens it must address Outline Structure of the immune system Anatomy of an immune response Role of the immune system in disease: infection, cancer and autoimmunity Organs of the Immune System Major organs of the immune system 1. Bone marrow – production of immune cells 2. Thymus – education of immune cells 3. Lymph Nodes – where an immune response is produced 4. Spleen – dual role for immune responses (especially antibody production) and cell recycling Origins of the Immune System B-Cell B-Cell Self-Renewing Common Progenitor Natural Killer Lymphoid Cell Progenitor Thymic T-Cell Selection Hematopoetic T-Cell Stem Cell Progenitor Dendritic Cell Myeloid Progenitor Granulocyte/M Macrophage onocyte Progenitor The Immune Response: The Art of War “Know your enemy and know yourself and you can fight a hundred battles without disaster.” -Sun Tzu, The Art of War Immunity: Two Systems and Their Key Players Adaptive Immunity Innate Immunity Dendritic cells (DC) B cells Phagocytes (Macrophages, Neutrophils) Natural Killer (NK) Cells T cells Dendritic Cells: “Commanders-in-Chief” • Function: Serve as the gateway between the innate and adaptive immune systems. -

Stress and the Immune System Tracy B
4 World Health • 47th Yeor, No. 2, Morch-Aprill994 Stress and the immune system Tracy B. Herbert any people have the effects of factors as diverse as experienced the examinations, bereavement, divorce, Mconnection between stress unemployment, mental arithmetic, and getting sick. Colds, influenza, and looking after a relative with herpes and allergies seem worse Alzheimer's di sease. In general, when we are severely stressed at these studies find that stress is work or in the home. Others are related to changes in both the never sick until they go on vacation numbers of white blood cells in (that is, after the stress is over), and circulation and the quantity of then they spend the whole time antibody in the blood. Moreover, fighting the virus. Because of stress is associated with changes in intrinsic connections like these, the functioning of immune cells. many researchers are today That is, there is a relatively large exploring whether (and how) stress decrease in both lymphocyte and illness are actually linked. One proliferation and natural killer cell specific focus of this research is to activity in individuals who have study the effects of stress on the experienced stress. There seems to immune systems; after all, if stress A lymphocyte: stress may weaken the capacity be some connection between the affects immunity, that would be one of lymphocytes to combat infection. duration of the stress and the amount way in which stress could contribute of immune change. For example, the to illness. longer the stress, the greater the The function of the immune proliferation"- by incubating these decrease in the number of specific system is to protect us from cells for several days with types of white blood cells. -

LECTURE 05 Acquired Immunity and Clonal Selection
LECTURE: 05 Title: ACQUIRED "ADAPTIVE" IMMUNITY & CLONAL SELECTION THEROY LEARNING OBJECTIVES: The student should be able to: • Recognize that, acquired or adaptive immunity is a specific immunity. • Explain the mechanism of development of the specific immunity. • Enumerate the components of the specific immunity such as A. Primary immune response. B. Secondary immune response • Explain the different phases that are included in the primary and secondary immune responses such as: A. The induction phase. B. Exponential phase. C. Steady phase. D. Decline phase. • Compare between the phases of the primary and secondary immune responses. • Determine the type of the immunoglobulins involved in each phase. • Determine which immunoglobulin is induced first and, that last longer. • Enumerate the characteristics of the specific immunity such as: A. The ability to distinguish self from non-self. B. Specificity. C. Immunological memory. • Explain naturally and artificially acquired immunity (passive, and active). • Explain the two interrelated and independent mechanisms of the specific immune response such as : A. Humoral immunity. B. Cell-mediated (cellular) immunity. • Recognize that, the specific immunity is not always protective, for example; sometimes it causes allergies (hay fever), or it may be directed against one of the body’s own constituents, resulting in autoimmunity (thyroditis). LECTURE REFRENCE: 1. TEXTBOOK: ROITT, BROSTOFF, MALE IMMUNOLOGY. 6th edition. Chapter 2. pp. 15-31 2. TEXTBOOK: ABUL K. ABBAS. ANDREW H. LICHTMAN. CELLULAR AND MOLECULAR IMMUNOLOGY. 5TH EDITION. Chapter 1. pg 3-12. 1 ACQUIRED (SPECIFIC) IMMUNITY INTRODUCTION Adaptive immunity is created after an interaction of lymphocytes with particular foreign substances which are recognized specifically by those lymphocytes. -

Med-Pathway Zoom Workshop
MCAT Immunology Dr. Phillip Carpenter medpathwaymcat Med-pathway AAMC MCAT Content Outline: Immunology Category 1A: Structure/Function of Proteins/AA Immune System Category 3B: Organ Systems Innate vs. Adaptive Immunity T and B Lymphocytes Macrophages & Phagocytes Tissue-Bone marrow, Spleen, Thymus, Lymph nodes Antigen and Antibody Antigen Presentation Clonal Selection Antigen-Antibody recognition Structure of antibody molecule Self vs. Non-self, Autoimmune Diseases Major Histocompatibility Complex Lab Techniques: ELISA & Western Blotting Hematopoiesis Creates Immune Cells Self vs. Non-self Innate vs Adaptive Innate Immunity Physical Barriers: Skin, mucous membranes, pH Inflammatory mediators: Complement, Cytokines, Prostaglandins Cellular Components: Phagocytes-Neutrophils, Eosinophils, Basophils, Mast Cells Antigen Presenting Cells-Monocytes, Macrophages, Dendritic Cells Adaptive (Acquired) Immunity Composed of B and T lymphocytes: Activated by Innate Immunity B cells: Express B cell receptor and secrete antibodies as plasma cells T cells: Mature in thymus, express TCR surface receptor; Activated by Antigen Presenting Cells (APCs) Direct Immune response (The Ringleaders of immune system) Major Lymphoid Organs TYPE SITE FUNCTION Fetal production of Liver 1° lymphoid cells Hematopoietic production of 1° Bone marrow myeloid and lymphoid cells Receives bone marrow T 1° Thymus cells; site where self is selected from non-self Lymph nodes 2° Sites of antigen activation Spleen of lymphocytes; clearance Macrophages (Sentinel Cells) Pattern Recognition -

Rapid Induction of Antigen-Specific CD4+ T Cells Guides Coordinated Humoral and Cellular Immune Responses to SARS-Cov-2 Mrna Vaccination
bioRxiv preprint doi: https://doi.org/10.1101/2021.04.21.440862; this version posted April 22, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Rapid induction of antigen-specific CD4+ T cells guides coordinated humoral and cellular immune responses to SARS-CoV-2 mRNA vaccination Authors: Mark M. Painter1,2, †, Divij Mathew1,2, †, Rishi R. Goel1,2, †, Sokratis A. Apostolidis1,2,3, †, Ajinkya Pattekar2, Oliva Kuthuru1, Amy E. Baxter1, Ramin S. Herati4, Derek A. Oldridge1,5, Sigrid Gouma6, Philip Hicks6, Sarah Dysinger6, Kendall A. Lundgreen6, Leticia Kuri-Cervantes1,6, Sharon Adamski2, Amanda Hicks2, Scott Korte2, Josephine R. Giles1,7,8, Madison E. Weirick6, Christopher M. McAllister6, Jeanette Dougherty1, Sherea Long1, Kurt D’Andrea1, Jacob T. Hamilton2,6, Michael R. Betts1,6, Paul Bates6, Scott E. Hensley6, Alba Grifoni9, Daniela Weiskopf9, Alessandro Sette9, Allison R. Greenplate1,2, E. John Wherry1,2,7,8,* Affiliations 1 Institute for Immunology, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA 2 Immune Health™, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA 3 Division of Rheumatology, University of Pennsylvania Perelman School of Medicine, Philadelphia, PA, USA 4 NYU Langone Vaccine Center, Department of Medicine, New York University School of Medicine, New York, NY 5 Department -
Understanding the Complement System
Understanding the Complement System WHAT IS THE IMMUNE SYSTEM? The immune system is a complex network of organs, cells and proteins which work together to protect the body against infection and disease. WHAT IS THE COMPLEMENT SYSTEM? The complement system is a part of the immune system and is essential to the body’s defense against infection. Classical Pathway Lectin Pathway Alternative Pathway Made up of 3 UNIQUE PATHWAYS (Classical, Lectin and Alternative) Each pathway can become activated to trigger a cascade of protein reactions that initiate an immune response Inflammation Marks pathogen/damaged to detect and eliminate: cells for elimination Bacteria Viruses Inflammation Targeted destruction of damaged cells Dead cells When the complement system is working properly, it is a strong and powerful tool that protects the body against harmful invaders. • brain But when the system is thrown out of • nervous system balance, or dysregulated, the proteins can trigger a dangerous, uncontrolled cascade • blood stream of reactions that attack cells and tissues. • kidneys UNLOCKING THE POTENTIAL OF THE COMPLEMENT SYSTEM Alexion’s pioneering legacy in rare diseases is rooted in being the first to translate the complex biology of the complement system into transformative medicines. 3 DECADES 20 YEARS of complement of real-world evidence demonstrating the safety inhibition research and power of targeted complement inhibitors Dysregulation of the complement system is a key driver of many devastating diseases. Alexion has paved the way for a new class of medicines that inhibit the complement system, prevent further damage and reduce disease symptoms. Alexion is committed to continue unlocking the potential of the complement system and accelerating the discovery and development of new life-changing therapies for even more patients. -

Homeostatic and Activated Conditions Cell
The Journal of Immunology Dynamics of the Splenic Innate-like CD19+CD45Rlo Cell Population from Adult Mice in Homeostatic and Activated Conditions Bele´n de Andre´s,*,1 Carmen Prado,* Beatriz Palacios,* Mario Alı´a,* Sharmili Jagtap,† Natalia Serrano,† Isabel Cortegano,* Miguel Angel R. Marcos,† and Maria Luisa Gaspar*,1 In the adult spleen, CD19+CD45R2/lo (19+45Rlo) lymphocytes of embryonic origin exist as a distinct population to that of the conventional B cell lineage. These cells display a plasmablast phenotype, and they spontaneously secrete IgG1 and IgA, whereas the bone marrow population of 19+45Rlo cells contains B1 progenitors. In this study, we show that 19+45Rlo cells are also present in Peyer’s patches and in the spleen throughout the life span of wild-type mice, beginning at postnatal day 7. Although this population is heterogeneous, the surface phenotype of most of these cells distinguishes them from follicular, transitional, marginal zone, and B1 cells. In CBA/CaHN mice, few 19+45Rlo cells were detected at postnatal day 7, and none was observed in the adult spleen. Splenic 19+45Rlo cells exhibited homeostatic BrdU uptake in vivo and actively transcribed cell cycle genes. When trans- ferred to immunodeficient RAG22/2gchain2/2 recipient mice, 19+45Rlo cells survived and differentiated into IgG1– and IgA– plasma cells. Moreover, in vitro stimulation of splenic 19+45Rlo cells with LPS, CpG, BAFF/IL4, and CD40/IL4 induced cell proliferation, IgG1/IgA secretion and the release of IL-10, suggesting a potential immunoregulatory role for this subset of innate- like B cells. The Journal of Immunology, 2012, 189: 2300–2308. -

Hormones and the Immune Response
Ann Rheum Dis: first published as 10.1136/ard.48.1.1 on 1 January 1989. Downloaded from Annals of the Rheumatic Diseases, 1989; 48, 1-6 Review Hormones and the immune response Recent advances suggest that the immune system cells, are present on mouse spleen cells3 and human does not function in isolation but is influenced by peripheral blood mononuclear cells.4 Receptors, other physiological systems such as the endocrine identical to those in the central nervous system, for and neuroendocrine systems. This review discusses methionine enkephalin are present on splenocytes aspects of immune function altered by neuroendo- and T lymphocytes.3 In contrast, leucine enkephalin crine peptides, sex hormones, and vitamin D and j3-endorphin receptors on T lymphocyte differ metabolites. from those in the central nervous system as binding cannot be inhibited by opiate antagonists.5 6 In the Neuroendocrine effects case of ,3-endorphin the bindings occur through its carboxy terminal, whereas opiates bind their A system of bidirectional communication between receptor through the amino terminus. This raises the immune and neuroendocrine system exists, in an interesting possibility that a peptide such as which the two systems share a common set of f6-endorphin could form a bridge between two hormones and receptors.'2 Not only do immune lymphocyte subtypes by binding to one through its for peptides, to the and cells possess receptors neuroendocrine amino terminus opiate receptor through copyright. they are also capable of synthesising them and of its carboxy terminus to the non-opiate receptor on responding to them. Products of immune cells affect another lymphocyte.4 the central nervous system, which possesses recep- Other neuroendocrine peptide receptors present tors for cytokines and can also synthesise them on leucocztes include those for neurotensin,7 sub- (Fig. -

B-Cell Lymphomas Differ in Their Responsiveness to Cpg Oligodeoxynucleotides
1490 Vol. 11, 1490–1499, February 15, 2005 Clinical Cancer Research B-Cell Lymphomas Differ in their Responsiveness to CpG Oligodeoxynucleotides Bernd Jahrsdorfer,5 Lars Mu¨hlenhoff,1 responsiveness to CpG oligodeoxynucleotides. Focusing Sue E. Blackwell,5 Moritz Wagner,1 clinical studies on patients with highly CpG oligodeoxynu- cleotide–sensitive B-cell malignancies may improve the Hendrik Poeck,1 Evelyn Hartmann,3 Ralf Jox,1 clinical outcome of such trials. Thomas Giese,4 Bertold Emmerich,2 Stefan Endres,1 5 1 George J. Weiner, and Gunther Hartmann INTRODUCTION 1 2 Division of Clinical Pharmacology and Department of Internal The vast majority of lymphoid neoplasms worldwide are Medicine, Division of Hematology, and 3Department of Otorhinolaryngology, University of Munich, Munich, Germany; derived from B lymphocytes at various stages of differentiation. 4Institute of Immunology, University of Heidelberg, Heidelberg, Neoplasms originating from precursor B cells are rare. Neo- Germany; and 5Holden Comprehensive Cancer Center and plasms derived from mature naive B cells include B-cell chronic Department of Internal Medicine, University of Iowa, Iowa City, Iowa lymphocytic leukemia (B-CLL), B-cell small lymphocytic lymphoma (SLL), and mantle cell lymphoma (MCL). Follicular lymphoma (FL) and diffuse large B-cell lymphoma (LCL) are ABSTRACT derived from germinal center B cells. Memory B cells can Human B cells detect CpG motifs within microbial DNA develop into marginal zone B-cell lymphoma (MZL) and B- via TLR9. Synthetic CpG oligodeoxynucleotides are currently CLL. Plasmacytoma is related to plasma cells (1). The most being tested in clinical trials for the therapy of different types typical lymphomas are of diffuse large B-cell type (33%) of B cell non-Hodgkin’s lymphoma.