MSU Member Handbook for Retirees Of
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

News, East Lansing, Michigan I
MICHIGAN STATE t a t e n e w s UNIVERSITY Sunday, November 14, 1965 East Lansing, Michigan WINBYWIN STANDINGS W L MSU13 UCLA 3 MICH. ST. 7 0 Ohio State 5 1 MSU 23 Penn St. 0 Minnesota 4 2 MSU 22 Illinois 12 Purdue 4 2 MSU 24 Michigan 7 Wisconsin 3 3 MSU 32 Ohio State 7 Illinois 3 3 MSU 14 Purdue 10 N ’western 2 4 jbmk -1 m m *mt m MSU 49 N’western 7 Michigan 2 4 MSU 35 Iow a 0 Indiana 1 5 Indiana 13 Io w a 0 7 MSU 27 A-2 Sunday, November 14, 1965 BIG TEN CHAMPIONS Unbeaten ! First Outright r all afternoon by an agj!gravated knee injury, ran for 47 yards and fumbled once. Indiana Throws Scare, This sloppy ball handling was partially due to the cold 39-degrcc weather. , , The Spartans ground out 194 yards rushing to Indiana s 65. Quarterback Frank Stavroff completed 14 of 27 attempted passes But State Rallies,27-13 for 173 yards. End Bill Malinchak haunted Slate’ s defensive lacks all after By RICK PI AN IN noon, catching five passes for 89 yards and one TD. Malinchak State News Staff W riter hauled in a beautiful 46-yard pass late in the second quarter and caught a 10-yard touchdown pass on the next play, with only 46 The Spartan football team claimed its seconds remaining. first undisputed Big Ten championship’here This cut State's early lead to 1 0 -7 and sparked Indiana to go ahead in the third quarter. -
Community Blue Group Benefits Certificate
SIMPLY BLUE℠ HRA GROUP BENEFITS CERTIFICATE LG (for large, insured group customers) © 2019 Blue Cross Blue Shield of Michigan This contract is between you and Blue Cross Blue Shield of Michigan. Because we are an independent corporation licensed by the Blue Cross and Blue Shield Association - an association of independent Blue Cross and Blue Shield plans - we are allowed to use the Blue Cross and Blue Shield names and service marks in the state of Michigan. However, we are not an agent of BCBSA and, by accepting this contract, you agree that you made this contract based only on what you were told by BCBSM or its agents. Only BCBSM has an obligation to provide benefits under this certificate and no other obligations are created or implied by this language. © 2019 Blue Cross Blue Shield of Michigan © 2019 Blue Cross Blue Shield of Michigan SIMPLY BLUE HRA GROUP BENEFITS CERTIFICATE LG Dear Subscriber: We are pleased you have selected Blue Cross Blue Shield of Michigan for your health care coverage. Your coverage provides many benefits for you and your eligible dependents. These benefits are described in this book, which is your certificate. Your certificate, your signed application and your BCBSM identification card are your contract with us. You may also have riders. Riders make changes to your certificate and are an important part of your coverage. When you receive riders, keep them with this book. This certificate will help you understand your benefits and each of our responsibilities before you require services. Please read it carefully. If you have any questions about your coverage, call us at one of the BCBSM customer service telephone numbers listed in the "How to Reach Us" section of this book. -
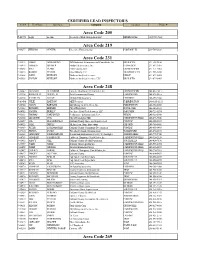
Area Code 205 Area Code 219 Area Code 231 Area
CERTIFIED LEAD INSPECTOR'S Cert # First Name Last Name Company Location Phone # Area Code 205 P-01571 Leigh Lachine Accelerated Risk Management LLC BIRMINGHAM (205)533-7662 Area Code 219 P-04277 WILLIAM CENTER Greentree Environmental PORTAGE, IN 219-764-2828 Area Code 231 P-01412 JAMES ARMSTRONG ARM Industrial & Environmental Consultants, Inc. BIG RAPIDS 231-592-9858 P-06974 HAROLD BROWER Norlund & Associates, Inc. LUDINGTON 231-843-3485 P-06268 KYLE CLARK PM Environmental GRAND RAPIDS 231-571-3082 P-00013 ROBERT PETERS Otwell Mawby P.C. TRAVERSE CITY 231-946-5200 P-01268 JOHN REHKOPF Northern Analytical Services LEROY 231-679-0005 P-05558 JUSTON REHKOPF Northern Analytical Services, LLC BIG RAPIDS 231-679-0005 Area Code 248 P-06647 ALI SALIH AL-HADDAD Fisbeck, Thompson, Carr & Huber, Inc. GRAND RAPIDS 248-410-7411 P-02334 ROOSEVELT AUSTIN, III Arch Environmental Group FARMINGTON 248-426-0165 P-06124 KATHLEEN BALAZE McDowell & Associates FERNDALE 248-399-2066 P-03480 JULIE BARTON AKT Peerless FARMINGTON 248-615-1333 P-04724 JASON BARYLSKI IAQ Management Services, Inc. FARMINGTON 248-932-8800 P-01082 RICHARD BREMER City of Royal Oak ROYAL OAK 248-246-3133 P-04983 JOSEPH BURLEY Freelance Envir-Tech Services, LLC OAK PARK 248-721-8574 P-05333 THOMAS CARPENTER Performance Environmental Serv. WIXOM 248-926-3800 P-06860 LEE EDWIN COX City of Farmington Hills FARMINGTON HILLS 248-473-9546 P-00657 JOE DEL MORONE II Oakland County Home and Improvement PONTIAC 248-858-5307 P-04823 JANE DIPPLE All American Home Inspections OXFORD 248-760-5441 P-00869 PETER ESSENMACHER Oakland County Community Development PONTIAC 248-858-0493 P-07010 DONNA EVANS Waterford Schools Transportation WATERFORD 248-674-2692 P-06262 GREGORY FAHRENBRUCH Restoration Environmental Safety Technologies AUBURN HILLS 248-778-5940 P-04763 JENNIFER FASHBAUGH Fishbeck, Thmpson, Carr & Huber, Inc. -

First Communications, LLC CLEC Price Guide
First Communications, LLC CLEC Price Guide First Communications, LLC This price guide sets forth the service offerings, rates, terms and conditions applicable to the furnishing of intrastate end-user telecommunications services by First Communications, LLC (“First”), hereinafter referred to as the Company, to customers within the State of Michigan. (N) 1 Effective: January 1, 2017 First Communications, LLC CLEC Price Guide TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................. 2 SECTION 1: DEFINITIONS ......................................................................................................................... 3 SECTION 2: Rules .......................................................................................................................................... 4 2.1 Undertaking of the Company ................................................................................................. 4 2.2 Prohibited Uses .................................................................................................................... 10 2.3 Obligations of the Customer ................................................................................................. 10 2.4 Customer Equipment and Channels ..................................................................................... 12 2.5 Payment Arrangements ........................................................................................................ -
PROGRAM (Annual Conf
83rd ANNUAL CONVENTION • Michigan Association '. ..' of County Drain Commissioners • HILTON INN LANSING, MICHIGAN • Wednesday, Thursday, Friday February 17th, 18th, 19th Nineteen Hundred Eighty-Two 1 N I 10 Df1l0l1 On behalf of the Association and myself personally, I wish to express my appreciation to the members of this organization for their assistance and cooperation during my term of office. Thomas Donahue President A thank you to all who have supported and worked with our association. My appreciation to all of you for your part in this convention and directory. Harry J. Harden Secretary-Treasurer RECEPTION COMMITTEE Thomas Donahue President Mr. & Mrs. Harry 1. Harden Secretary-Treasurer Mr. & Mrs. Jack Robinson 1st Vice-President Mr. George Griffiths Ingham County Drain Commissioner Mr. & Mrs. Hal Halquist Chairman Entertainment Committee INDEX Life Memberships ... ... ... .. .. .. ........... ... .. 5 M.A.C.D.C. Winter Program 198 1.... .... ..... .. 6,7 Association Officers and Committees . .. ..... .. 8,9, I 0, I I Drain Commissioners .. .. .... ............ .. 12,13 Association Members and Agents of Contributors .. .... ..... ..... .. ..... 14,15,16,17,18,19,20.21 ,22 ADVERTISERS FOR 1982 Contractors Boeve Construction Co. ... ..... ... .. ... .. .. 30 Donald D. Lapham ... .. ... .... .. .. .. ..... ..... 26 Dunigan Bros. , Inc . ....... .... ... .. ......... .... 27 E. L. Erickson . .. .... .... ........ ... ......... ..... 27 Easlick Contracting, Inc. - E & E Construction Co .. ... 31 Greenfield Construction Company, Inc ... -

Carter Named County Clerk
112th Year, No. 39 ST. JOHNS, MICH. — THURSDAY, iJANUARY"l87V967 2 SECTIONS - 28 PAGES 15 Cents Clinton bogged down 1 day by weekend snow Schools • •- • • • • • • • closed Monday Carter named Clinton County gots its first real winter snow storm Sunday night, and the seven inches of heavy snow which fell succeeded in clogging things up to a great extent all over the county. county clerk All schools were closed Monday as winds and the accum ulation of snow drifted rural roads and driveways—partic ularly east-west roads, although some north-south roads were in Tiedt equalization director the same conditions. Clinton County Road Commis Two changes in Clinton County officialdom were confirmed sion spreader trucks worked all this week with the formal announcement that Ernest Carter of day Sunday salting the state high ways and the principal primary Watertown Township has been named county clerk and Lorenz roads of the county, and Monday Tiedt of St. Johns has been appointed county equalization director. morning 14 snow plowers were mounted on trucks and sent out Circuit Judge Leo M. Corkin announced the appointment Monday to clear the roads of snow. Three of Carter, who is presently Watertown Township supervisor and motor graders and five trucks spreading salt were also out. chairman of the Clinton County Board of Supervisors. His new appointment is effective Feb. 1. BY MONDAY NIGHT, almost all east-west roads had been Carter replaces the plowed once, and Tuesday morn ^Y. late Paul Wakefield, ing county road crews started in the other directions. Many of who died Dec. -
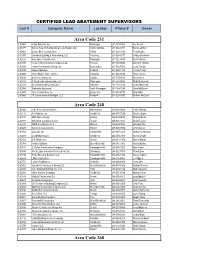
Area Code 231 Area Code 248 Area Code
CERTIFIED LEAD ABATEMENT SUPERVISORS Cert # Company Name Location Phone # Owner Area Code 231 C-00483 4-Star Builders, Inc. Muskegon 231-773-7000 Joe Ferrier C-00779 Barry’s Total Home Maintenance & Repairs LLC Harbor Springs 231-526-4391 Barry Lambert C-00869 Beattie Bros. Construction Holton 231-638-3516 Tony Beattie C-00937 Grantham Building & Remodeling, LLC Petoskey 231-838-8777 Jeffrey Grantham C-00232 Gray Space Construction Muskegon 231-722-4430 Curtis Holden C-00918 Ironwood Construction Company, LLC Petosky 231-439-5590 Daniel R. Steffes C-00800 Jordan Construction Group, Inc. East Jorden 231-536-0600 Larry Trumble C-00819 Midwest Builders Fruitport 231-865-1118 Joseph Fehler C-00928 Myers Mobile Home Service Benzonia 231-882-9479 Shane Myers C-00410 Nichols Construction Cadillac 231-775-0020 Roy Nichols C-00797 R. Backensto Construction, LLC Muskegon 231-578-4982 Ricky Backensto C-00379 Scott Adamczak Construction Manistee 231-723-2214 Scott Adamczak C-00368 Statewide Abatement North Muskegon 231-744-7244 Dave McQueen C-00935 Thor Construction, Inc. Boyne City 231-675-4717 Chip Witte C-00860 TK Construction of Michigan, LLC Fremont 231-225-8766 Charles McCloud Area Code 248 C-00936 4 the Environment Service Walled Lake 248-838-9636 Leslie Pittman C-00172 A-1 Builders, Inc Southfield 248-875-7595 Chhote Gupta C-00185 ABR Alpine Design Berkley 248-584-5679 Richard Burke C-00283 Annointed Construction LLC Detroit 248-905-5033 David Fouche‘ C-00829 BBEK Construction LLC Warren 248-674-1600 Grzegpiz Rej C-00605 Burrow Construction Inc. Milford 248-563-9886 John Burrow C-00706 Concraft, Inc. -
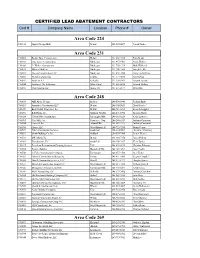
Area Code 231 Area Code 248 Area Code 224 Area Code
CERTIFIED LEAD ABATEMENT CONTRACTORS Cert # Company Name Location Phone # Owner Area Code 224 C-01036 August Design Build Detroit 224-567-0697 Patrick Linder Area Code 231 C-00869 Beattie Bros. Construction Holton 231-638-3516 Tony Beattie C-00232 Gray Space Construction Muskegon 231-955-9701 Curtis Holden C-01060 Jr. Walker Construction Muskegon 231-750-1719 Mark Walker Jr. C-00819 Midwest Builders Muskegon 231-206-3569 Joseph Fehler C-00981 Nassau Construction, LLC Muskegon 231-638-7880 Francena DePung C-00410 Nichols Construction Cadillac 231-775-0020 Roy Nichols C-00953 Northern A-1 Kalkaska 231-258-9961 Edward Ascione C-00944 Northwest Tile & Interiors White Cloud 231-689-6836 Edward Walters C-00935 Thor Construction Boyne City 231-675-4717 Chip Witte Area Code 248 C-00185 ABR Alpine Design Berkley 248-506-0940 Richard Burke C-00283 Annointed Construction LLC Detroit 248-905-5033 David Fouche‘ C-01059 Back To Life Properties, Inc. Detroit 248-761-3213 Kenneth Loggins C-00296 B.D. Harris, Inc. Madison Heights 248-291-5392 Benston Harris C-00324 Call On Him Construction Farmington Hills 248-615-0250 Kevin Lawrence C-00995 CasaValle, Inc. Commerce Twp. 248-246-6333 Anthony Casanova C-00706 Concraft, Inc. Auburn Hills 248-867-3213 Anthony Crimando C-00990 Cymex LLC West Bloomfield 248-722-7335 Martin Petrov C-00529 D & A Construction Services Southfield 248-424-9001 Demetris Armstrong C-00293 Dewitt Building Co. Inc. Oakland 248-559-7300 James Weiner C-00722 D.R. Martin, Inc. Detroit 248-210-7376 Darnell Martin C-01062 Enerdynamic, LLC Southfield 248-450-3467 Kevin Bailey C-01017 Everclean Restoration & Cleaning Services Troy 248-439-0215 Christian Fahoome C-00784 Fortune Builders Bloomfield Hills 248-342-3093 Ajay Chadha C-00748 G. -
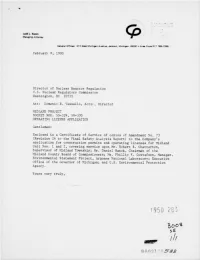
Forwards Certificate of Svc Re Amend 73 to Application for Cps & Ols
< % - 3 . ..... ,, , s. > ,, s ~ . ~ ~ ' Judd L. Bacon ' ' ' Managing Attorney General offices: 212 West Michigan Avenue, Jackson, Michigan 49201 e Area Code 517 788-1366 February 8, 1980 Director of Nuclear Reactor Regulation U.S. Nuclear Regulatory Coc: mission Washington, DC 20555 Att: Domenic B. Vassallo, Actir t Director MIDLAND PROJECT DOCKET NOS. 50-329, 50-330 OPERATING LICENSE APPLICATION Gentlemen: Enclosed is a Certificate of Service of copies of Amendment No. 73 (Revision 26 to the Final Safety Arialysis Report) to the Company's application for construction permits and operating licenses for Midland Unit Nos. 1 and 2, covering service upon Mr. Robert B. Chatterton, Supervisor of Midland Township; Mr. Daniel Ranck, Chairman of the Midland County Board of Con:missioners; Mr. Phillip F. Gustafson, Manager, Environmental Statement Project, Argonne National Laboratory; Executive Office of the Governor of Michigan; and U.S. Environmental Protection Agency. Yours very truly,_ . .. c~ - 1950 283 Boos SE , /// 8 0 021905BB . - UNITED STATES OF AMERICA NUCLEAR REGULATORY COMMISSION In the Matter of ) CONSUMERS POWER COMPANY ) Application for Reactor ) Docket No. 50-329 Construction Permit and ) Docket No. 50-330 Operating License ) ) CERTIFICATL OF SERVICE Amendment No. 73 (Revision 26 to the Final Safety Analysis Report) to Consumers Power Company's Application for Reactor Construction Permit and Operating License for Midland Plant Unit Nos. 1 and 2 has been served today upon the following persons by deposit in the United States mail: U.S. Environmental Protection Agency Mr. Robert B. Chatterton Federal Activities Branch Supervisor of Midland Township Region V Office 928 Clarence Court, Route 7 Attention: EIS Coordinator Midland, Michigan 48640 230 South Dearborn Street Chicago, Illinois 60606 Mr. -

List of Contractors.Xlsx
CERTIFIED LEAD ABATEMENT CONTRACTORS Cert #Company Name Location Phone # Owner Area Code 231 C-00483 4-Star Builders, Inc. Muskegon 231-773-7000 Joe Ferrier C-00869 Beattie Bros. Construction Holton 231-638-3516 Tony Beattie C-00937 Grantham Building & Remodeling, LLC Petoskey 231-838-8777 Jeffrey Grantham C-00232 Gray Space Construction Muskegon 231-955-9701 Curtis Holden C-00918 Ironwood Construction Company, LLC Petosky 231-439-5590 Daniel R. Steffes C-00977 JNL Hunt Construction Company, LLC Hesperia 231-854-6325 Jeffrey Hunt C-00800 Jordan Construction Group, Inc. East Jorden 231-536-0600 Larry Trumble C-00819 Midwest Builders Fruitport 231-865-1118 Joseph Fehler C-00928 Myers Mobile Home Service Benzonia 231-882-9479 Shane Myers C-00410 Nichols Construction Cadillac 231-775-0020 Roy Nichols C-00953 Northern A-1 Kalkaska 231-258-9961 Edward Ascione C-00944 Northwest Tile & Interiors White Cloud 231-689-6836 Edward Walters C-00797 R. Backensto Construction, LLC Muskegon 231-578-4982 Ricky Backensto C-00379 Scott Adamczak Construction Manistee 231-723-2214 Scott Adamczak C-00368 Statewide Abatement North Muskegon 231-744-7244 Dave McQueen C-00935 Thor Construction, Inc. Boyne City 231-675-4717 Chip Witte C-00860 TK Construction of Michigan, LLC Fremont 231-225-8766 Charles McCloud Area Code 248 C-00172 A-1 Builders, Inc Southfield 248-875-7595 Chhote Gupta C-00185 ABR Alpine Design Berkley 248-584-5679 Richard Burke C-00948 Ace Professional Solutions Farmington Hills 248-470-2828 Amit Pathak C-00283 Annointed Construction LLC Detroit 248-905-5033 David Fouche‘ C-00980 At Work Builders, LLC West Bloomfield 248-631-6654 Dashawn Stewart C-00829 BBEK Construction LLC Warren 248-674-1600 Grzegpiz Rej C-00296 B.D. -
County Drain
76th ANNUAL CONVENTION • Michigan Association of County Drain Commissioners • RAMADA INN MIDLAND, MICHIGAN • Wednesday, Thursday, Friday February 12th, 13th, 14th Nineteen Hundred Seventy-Five ,. o "'f:ftllt.Jrrtt: 0 11 0 m . ~ ~n ~ us IOeIJSIH£S$ 0 .,. " '".. 0 0 [] 0 0 343 ENTRANCE" 318 344 o 1ST FLOOR 319 345 320 346 321. 347 322 348 , liCE EII1"'" RAMADA INN 1ST FLOOR Motel Rooms (301 to 388) A - Registration Lobby B - Gift Shop C - Goodie Shop H D - Game Room and Sport Courts E - Lobby Lounge (Cocktails) D F - I ndoor Swimming Pools G - Health Spa (Sauna, Whirlpool, Exercise Area) X - Vending Area 2ND FLOOR J 2ND FLOOR Motel Rooms - same as 1st floor (401 to 488) H - Captain Nemo - Garden Room I - Captain Nemo - Cocktail Lounge J - Captain Nemo - Dining Rooms K - Meeting Rooms (464-466-471-473) I sincerely appreciate the privilege of serving as your Secretary-Treasurer and trust that the office has been efficiently managed to meet your ap proval. Should there be any corrections necessary I in this program, please notify me so that the Sec - retary's office can compile a completely accurate record of all members, contractors, suppl iers, en gineers and consultants. THOMASE.MOORE Secretary-Treasurer On behalf of the Association and myself person ally, I wish to express my appreciation to the mem bers of this organization for their assistance and co operation during my term of office. ORRIE FRANCIS President -1- INDEX In Memoriam ..................... 4 Life Memberships ................. 4 Association Officers and Committees ... 5,6,7 Drain Commissioners .............. 8,9 Paid-up Memberships ....... -
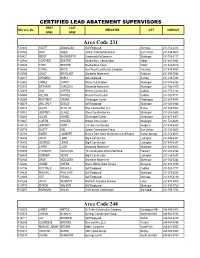
Area Code 231 Area Code
CERTIFIED LEAD ABATEMENT SUPERVISORS FIRST LAST HHS Cert. No. EMPLOYER CITY CONTACT NAME NAME Area Code 231 P-03036 SCOTT ADAMCZAK Self Employed Manistee 231-723-2214 P-05762 RICK AGER Jordan Construction Group East Jordan 231-536-0600 P-04421 RICKY BACKENSTO Community EnCompass Muskegon 231-728-3117 P-05944 HEATHER BEATTIE Beattie Bros. Construction Holton 231-821-0892 P-05945 TONY BEATTIE Beattie Bros. Const. Holton 231-638-3516 P-06263 CRAIG BOYD Iron Wood Construction Company Petoskey 231-439-5590 P-03769 SAM T. BRUFLADT Statewide Abatement Rothbury 231-893-7256 P-06337 WENDELL BUELL Self-employed Buckley 231-218-5338 P-00962 JAMES CANTU Mossy Oak Builders Muskegon 231-578-6286 P-01376 BRYAN M. CARLSON Statewide Abatement Muskegon 231-788-2470 P-04079 GUY COFFEL Nichols Construction Cadillac 231-775-3192 P-04080 KELVIN COFFEL Nichols Construction Cadillac 231-920-7777 P-06264 MATTHEW CRONK Cheboygan County Cheboygan 231-627-8488 P-06079 WILLIAM F. DODGE Self Employed Muskegon 231-343-0844 P-04473 ALLEN ELYA, JR. Elya Construction, LLC Brutus 231-529-7002 P-05551 JEFFREY GLASS Glass Construction Inc. Muskegon 231-206-2665 P-06265 ALLAN HOARD Cheboygan County Cheboygan 231-627-8407 P-01467 CURTIS HOLDEN Holden Construction Muskegon 231 722-4430 P-04128 JEFFERY HUNT J A Hunt Construction Hesperia 231-854-6325 P-05778 DUSTY KIEL Jordan Construction Group East Jordan 231-536-0600 P-05164 BARRY LAMBERT Barry’s Total Home Maintenance and Repair Harbor Springs 231-373-6009 P-06404 JOHN LARR Big K Construction Ludington 231-845-6347 P-06403 GEORGE LEWIS Big K Construction Ludington 231-845-6347 P-03553 LARRY LOVE Statewide Abatement Muskegon 231-638-6302 P-05889 CHARLES MCCLOUD TK Construction of Mich/Self Empl.