Community Blue Group Benefits Certificate
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Area Code 205 Area Code 219 Area Code 231 Area
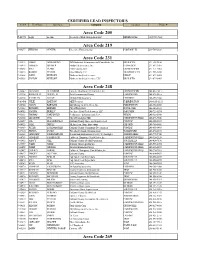
CERTIFIED LEAD INSPECTOR'S Cert # First Name Last Name Company Location Phone # Area Code 205 P-01571 Leigh Lachine Accelerated Risk Management LLC BIRMINGHAM (205)533-7662 Area Code 219 P-04277 WILLIAM CENTER Greentree Environmental PORTAGE, IN 219-764-2828 Area Code 231 P-01412 JAMES ARMSTRONG ARM Industrial & Environmental Consultants, Inc. BIG RAPIDS 231-592-9858 P-06974 HAROLD BROWER Norlund & Associates, Inc. LUDINGTON 231-843-3485 P-06268 KYLE CLARK PM Environmental GRAND RAPIDS 231-571-3082 P-00013 ROBERT PETERS Otwell Mawby P.C. TRAVERSE CITY 231-946-5200 P-01268 JOHN REHKOPF Northern Analytical Services LEROY 231-679-0005 P-05558 JUSTON REHKOPF Northern Analytical Services, LLC BIG RAPIDS 231-679-0005 Area Code 248 P-06647 ALI SALIH AL-HADDAD Fisbeck, Thompson, Carr & Huber, Inc. GRAND RAPIDS 248-410-7411 P-02334 ROOSEVELT AUSTIN, III Arch Environmental Group FARMINGTON 248-426-0165 P-06124 KATHLEEN BALAZE McDowell & Associates FERNDALE 248-399-2066 P-03480 JULIE BARTON AKT Peerless FARMINGTON 248-615-1333 P-04724 JASON BARYLSKI IAQ Management Services, Inc. FARMINGTON 248-932-8800 P-01082 RICHARD BREMER City of Royal Oak ROYAL OAK 248-246-3133 P-04983 JOSEPH BURLEY Freelance Envir-Tech Services, LLC OAK PARK 248-721-8574 P-05333 THOMAS CARPENTER Performance Environmental Serv. WIXOM 248-926-3800 P-06860 LEE EDWIN COX City of Farmington Hills FARMINGTON HILLS 248-473-9546 P-00657 JOE DEL MORONE II Oakland County Home and Improvement PONTIAC 248-858-5307 P-04823 JANE DIPPLE All American Home Inspections OXFORD 248-760-5441 P-00869 PETER ESSENMACHER Oakland County Community Development PONTIAC 248-858-0493 P-07010 DONNA EVANS Waterford Schools Transportation WATERFORD 248-674-2692 P-06262 GREGORY FAHRENBRUCH Restoration Environmental Safety Technologies AUBURN HILLS 248-778-5940 P-04763 JENNIFER FASHBAUGH Fishbeck, Thmpson, Carr & Huber, Inc. -

First Communications, LLC CLEC Price Guide
First Communications, LLC CLEC Price Guide First Communications, LLC This price guide sets forth the service offerings, rates, terms and conditions applicable to the furnishing of intrastate end-user telecommunications services by First Communications, LLC (“First”), hereinafter referred to as the Company, to customers within the State of Michigan. (N) 1 Effective: January 1, 2017 First Communications, LLC CLEC Price Guide TABLE OF CONTENTS TABLE OF CONTENTS ................................................................................................................................. 2 SECTION 1: DEFINITIONS ......................................................................................................................... 3 SECTION 2: Rules .......................................................................................................................................... 4 2.1 Undertaking of the Company ................................................................................................. 4 2.2 Prohibited Uses .................................................................................................................... 10 2.3 Obligations of the Customer ................................................................................................. 10 2.4 Customer Equipment and Channels ..................................................................................... 12 2.5 Payment Arrangements ........................................................................................................ -
Area Code 231 Area Code 248 Area Code
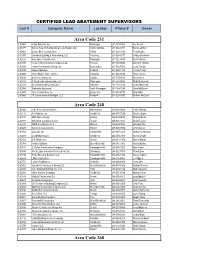
CERTIFIED LEAD ABATEMENT SUPERVISORS Cert # Company Name Location Phone # Owner Area Code 231 C-00483 4-Star Builders, Inc. Muskegon 231-773-7000 Joe Ferrier C-00779 Barry’s Total Home Maintenance & Repairs LLC Harbor Springs 231-526-4391 Barry Lambert C-00869 Beattie Bros. Construction Holton 231-638-3516 Tony Beattie C-00937 Grantham Building & Remodeling, LLC Petoskey 231-838-8777 Jeffrey Grantham C-00232 Gray Space Construction Muskegon 231-722-4430 Curtis Holden C-00918 Ironwood Construction Company, LLC Petosky 231-439-5590 Daniel R. Steffes C-00800 Jordan Construction Group, Inc. East Jorden 231-536-0600 Larry Trumble C-00819 Midwest Builders Fruitport 231-865-1118 Joseph Fehler C-00928 Myers Mobile Home Service Benzonia 231-882-9479 Shane Myers C-00410 Nichols Construction Cadillac 231-775-0020 Roy Nichols C-00797 R. Backensto Construction, LLC Muskegon 231-578-4982 Ricky Backensto C-00379 Scott Adamczak Construction Manistee 231-723-2214 Scott Adamczak C-00368 Statewide Abatement North Muskegon 231-744-7244 Dave McQueen C-00935 Thor Construction, Inc. Boyne City 231-675-4717 Chip Witte C-00860 TK Construction of Michigan, LLC Fremont 231-225-8766 Charles McCloud Area Code 248 C-00936 4 the Environment Service Walled Lake 248-838-9636 Leslie Pittman C-00172 A-1 Builders, Inc Southfield 248-875-7595 Chhote Gupta C-00185 ABR Alpine Design Berkley 248-584-5679 Richard Burke C-00283 Annointed Construction LLC Detroit 248-905-5033 David Fouche‘ C-00829 BBEK Construction LLC Warren 248-674-1600 Grzegpiz Rej C-00605 Burrow Construction Inc. Milford 248-563-9886 John Burrow C-00706 Concraft, Inc. -
Area Code 231 Area Code 248 Area Code 224 Area Code
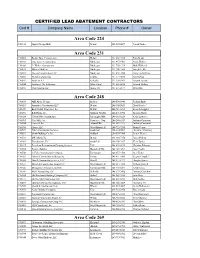
CERTIFIED LEAD ABATEMENT CONTRACTORS Cert # Company Name Location Phone # Owner Area Code 224 C-01036 August Design Build Detroit 224-567-0697 Patrick Linder Area Code 231 C-00869 Beattie Bros. Construction Holton 231-638-3516 Tony Beattie C-00232 Gray Space Construction Muskegon 231-955-9701 Curtis Holden C-01060 Jr. Walker Construction Muskegon 231-750-1719 Mark Walker Jr. C-00819 Midwest Builders Muskegon 231-206-3569 Joseph Fehler C-00981 Nassau Construction, LLC Muskegon 231-638-7880 Francena DePung C-00410 Nichols Construction Cadillac 231-775-0020 Roy Nichols C-00953 Northern A-1 Kalkaska 231-258-9961 Edward Ascione C-00944 Northwest Tile & Interiors White Cloud 231-689-6836 Edward Walters C-00935 Thor Construction Boyne City 231-675-4717 Chip Witte Area Code 248 C-00185 ABR Alpine Design Berkley 248-506-0940 Richard Burke C-00283 Annointed Construction LLC Detroit 248-905-5033 David Fouche‘ C-01059 Back To Life Properties, Inc. Detroit 248-761-3213 Kenneth Loggins C-00296 B.D. Harris, Inc. Madison Heights 248-291-5392 Benston Harris C-00324 Call On Him Construction Farmington Hills 248-615-0250 Kevin Lawrence C-00995 CasaValle, Inc. Commerce Twp. 248-246-6333 Anthony Casanova C-00706 Concraft, Inc. Auburn Hills 248-867-3213 Anthony Crimando C-00990 Cymex LLC West Bloomfield 248-722-7335 Martin Petrov C-00529 D & A Construction Services Southfield 248-424-9001 Demetris Armstrong C-00293 Dewitt Building Co. Inc. Oakland 248-559-7300 James Weiner C-00722 D.R. Martin, Inc. Detroit 248-210-7376 Darnell Martin C-01062 Enerdynamic, LLC Southfield 248-450-3467 Kevin Bailey C-01017 Everclean Restoration & Cleaning Services Troy 248-439-0215 Christian Fahoome C-00784 Fortune Builders Bloomfield Hills 248-342-3093 Ajay Chadha C-00748 G. -
MSU Member Handbook for Retirees Of
Member Handbook for retirees of Traditional Guide Comprehensive Major Medical Preferred Provider Organization (PPO) Dear Subscriber: We are pleased you have selected Blue Cross Blue Shield of Michigan for your health care coverage. Your coverage provides many benefits for you and your eligible dependents. Your benefits are described in this booklet, which outlines your certificate and riders. Your certificate, your signed application and your BCBSM identification card are your contract with us. You may also have riders. Riders make changes to your certificate and are an important part of your coverage. When you receive riders, keep them with this book. This booklet will help you understand your benefits and each of our responsibilities before you require services. Please read it carefully. If you have any questions about your coverage, call us at one of the BCBSM Customer Service telephone numbers listed in the “How to Reach Us” section of this book. Thank you for choosing Blue Cross Blue Shield of Michigan. We are dedicated to giving you the finest service and look forward to serving you for many years. Sincerely, Daniel J. Loepp President and Chief Executive Officer Blue Cross Blue Shield of Michigan How to Reach Us This section lists phone numbers and addresses to help you get information quickly. You may call or visit our BCBSM Customer Service center. To Call Most of our BCBSM Customer Service lines are open for calls from 8:30 a.m. to noon and from 1 p.m. to 5 p.m., Monday through Friday. Please have your ID card with your group and contract numbers ready when you call. -

List of Contractors.Xlsx
CERTIFIED LEAD ABATEMENT CONTRACTORS Cert #Company Name Location Phone # Owner Area Code 231 C-00483 4-Star Builders, Inc. Muskegon 231-773-7000 Joe Ferrier C-00869 Beattie Bros. Construction Holton 231-638-3516 Tony Beattie C-00937 Grantham Building & Remodeling, LLC Petoskey 231-838-8777 Jeffrey Grantham C-00232 Gray Space Construction Muskegon 231-955-9701 Curtis Holden C-00918 Ironwood Construction Company, LLC Petosky 231-439-5590 Daniel R. Steffes C-00977 JNL Hunt Construction Company, LLC Hesperia 231-854-6325 Jeffrey Hunt C-00800 Jordan Construction Group, Inc. East Jorden 231-536-0600 Larry Trumble C-00819 Midwest Builders Fruitport 231-865-1118 Joseph Fehler C-00928 Myers Mobile Home Service Benzonia 231-882-9479 Shane Myers C-00410 Nichols Construction Cadillac 231-775-0020 Roy Nichols C-00953 Northern A-1 Kalkaska 231-258-9961 Edward Ascione C-00944 Northwest Tile & Interiors White Cloud 231-689-6836 Edward Walters C-00797 R. Backensto Construction, LLC Muskegon 231-578-4982 Ricky Backensto C-00379 Scott Adamczak Construction Manistee 231-723-2214 Scott Adamczak C-00368 Statewide Abatement North Muskegon 231-744-7244 Dave McQueen C-00935 Thor Construction, Inc. Boyne City 231-675-4717 Chip Witte C-00860 TK Construction of Michigan, LLC Fremont 231-225-8766 Charles McCloud Area Code 248 C-00172 A-1 Builders, Inc Southfield 248-875-7595 Chhote Gupta C-00185 ABR Alpine Design Berkley 248-584-5679 Richard Burke C-00948 Ace Professional Solutions Farmington Hills 248-470-2828 Amit Pathak C-00283 Annointed Construction LLC Detroit 248-905-5033 David Fouche‘ C-00980 At Work Builders, LLC West Bloomfield 248-631-6654 Dashawn Stewart C-00829 BBEK Construction LLC Warren 248-674-1600 Grzegpiz Rej C-00296 B.D. -

LEAD ABATEMENT CONTRACTORS Cert # Company Name Location Phone # Owner
https://www.michigan.gov/mdhhs/0,5885,7-339-71548_54783_54784_74881-12875--,00.html CERTIFIED LEAD ABATEMENT CONTRACTORS Cert # Company Name Location Phone # Owner Area Code 231 C-00483 4 Star Builders, Inc. Muskegon 231-773-7000 Joe Ferrier C-00869 Beattie Bros. Construction Holton 231-638-3516 Tony Beattie C-00985 Bob Thornton Builder Excavator Traverse City 231-638-3420 Bob Thornton C-00937 Grantham Building & Remodeling, LLC Petoskey 231-838-8777 Jeffrey Grantham C-00232 Gray Space Construction Muskegon 231-955-9701 Curtis Holden C-00977 JNL Hunt Construction Company, LLC Hesperia 231-854-6325 Jeffrey Hunt C-00819 Midwest Builders Muskegon 231-206-3569 Joseph Fehler C-00410 Nichols Construction Cadillac 231-775-0020 Roy Nichols C-00953 Northern A-1 Kalkaska 231-258-9961 Edward Ascione C-00944 Northwest Tile & Interiors White Cloud 231-689-6836 Edward Walters C-00797 R. Backensto Construction, LLC Muskegon 231-578-4982 Ricky Backensto C-00379 Scott Adamczak Construction Manistee 231-723-2214 Scott Adamczak Area Code 248 C-00185 ABR Alpine Design Berkley 248-506-0940 Richard Burke C-00948 Ace Professional Solutions Farmington Hills 248-470-2828 Amit Pathak C-00283 Annointed Construction LLC Detroit 248-905-5033 David Fouche‘ C-00296 B.D. Harris, Inc. Madison Heights 248-291-5392 Benston Harris C-00324 Call On Him Construction Farmington Hills 248-615-0250 Kevin Lawrence C-00706 Concraft, Inc. Auburn Hills 248-867-3213 Anthony Crimando C-00529 D & A Construction Services Southfield 248-424-9001 Demetris Armstrong C-00293 Dewitt Building Co. Inc. Oakland 248-559-7300 James Weiner C-00722 D.R. -

A Brief History of Oceana County
**Changes made after printing are highlighted. TABLE OF CONTENTS Census Numbers by Jurisdictions……………………………………… Courthouse Hours…………………………………………………………… Telephone Directory……………………………………………………….. National Officers……………………………………………………………… State Officers………………………………………………………………….. Board of Commissioners……………………………………………………. County Offices………………………………………………………………… Local Boards and Committees……………………………………………. TOWNSHIPS Benona Township……………………………………………………………. Claybanks Township………………………………………………………… Colfax Township……………………………………………………………… Crystal Township……………………………………………………………. Elbridge Township………………………………………………………….. Ferry Township………………………………………………………………. Golden Township…………………………………………………………… Grant Township……………………………………………………………… Greenwood Township………………………………………………………. Hart Township……………………………………………………………….. Leavitt Township…………………………………………………………….. Newfield Township…………………………………………………………… Otto Township………………………………………………………………… Pentwater Township………………………………………………………… Shelby Township…………………………………………………………….. Weare Township……………………………………………………………… CITY City Of Hart…..……………………………………………………………….. VILLAGES Village of Hesperia……………………………………………………………. Village of New Era……………………………………………………………. Village of Pentwater………………………………………………………….. Village of Rothbury…………………………………………………………… Village of Shelby………………………………………………………………. Village of Walkerville………………………………………………………… UPDATES TO THIS COUNTY DIRECTORY MAY BE FOUND AT www.oceana.mi.us/clerk **Changes made after printing are highlighted. A BRIEF HISTORY OF OCEANA COUNTY The first settlement in Oceana