Coordinated Care Plan User Guide Guidelines and Examples
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

„When Am I?“ – Zeitlichkeit in Der US-Serie LOST, Teil 2
GABRIELE SCHABACHER „When Am I?“ – Zeitlichkeit in der US-Serie LOST, Teil 2 Previously on … An der US-Serie LOST lässt sich eine systematische Nutzung der temporalen Di- mension beobachten: Auf den Ebenen von Erzählzeit und erzählter Zeit – das konnte der erste Teil dieses Beitrags zeigen – ist der Einsatz von story arcs überspan- nenden Flashbacks bzw. Flashforwards sowie eine handlungsseitig ausgeführte Thematisierung und Problematisierung von Zeitreisen und Teleportation für das Seriennarrativ zentral. Schon diese zeitlichen Relationen ermöglichen der Narra- tion entscheidende Inversionen und paradoxe Konstruktionen, die für die Serie LOST charakteristisch geworden sind. 1. Die dritte Zeit Eine dritte Dimension der Narration, um die es dem zweiten Teil dieses Beitrags geht, lässt sich nun keiner der beiden bisher thematisierten Gruppen eindeutig zuordnen, weder also der Erzählzeit und damit den stilistischen Mitteln im engeren Sinne, noch der erzählten Zeit, d. h. der inhaltlichen Ebene der Geschichte. Es handelt sich vielmehr um eine Gruppe von Phänomen, die sich durch eine spezifi - sche Übergängigkeit zwischen diesen beiden Kategorien auszeichnen. Daher wird im Folgenden auf die in der Serie geäußerten Vorahnungen, Time Loops, Bewusst- seinsreisen und Zeitsprünge einzugehen sein, um die Hybridisierung von Stilistik und Inhaltsmomenten der Narration zu verdeutlichen. Das Vorhandensein solcher hybrider Elemente ist es, das eine mögliche Erklärung für die besondere Faszinati- on an LOST und eine spezifi sch temporal motivierte Komplexität -
Hamilton Niagara Haldimand Brant Health Links Coordinated Care Planning Toolkit
Hamilton Niagara Haldimand Brant Hamilton Niagara Haldimand Brant Health Links Coordinated Care Planning Toolkit April 1, 2016 Who should use this toolkit? This toolkit is for any individual or organization who will be participating in coordinated care planning. What is the purpose of this toolkit? This toolkit will describe the Coordinated Care Planning Framework and will provide staff with the tools, templates, and resources to support the creation and maintenance of Coordinated Care Plans (CCP) within an interdisciplinary care team. This toolkit contains all key documents and the links to each individual document. Simply click on the document title under the Table of Contents and you will be directed to the working tool, form, or template. Table of Contents Contents Page Introduction Health Link Model of Care Process and Key Requirements………………………………………………..2 Process Diagram………………………………………………………………………………………………..14 5% Cohort Target Population Definition and Criteria………………………………………………………..15 Coordinated Care Plan Process and Practice Coordinated Care Plan Detail Template……………………………………………………………………...16 HQO CCP User Guide………………………………………………………………………………………….20 Identification and Invite Health Link Patient Introduction Outline………………………………………………………….…………...58 Client Engagement Outline……………………………………………………………………………………..60 Generic Health Link Referral Form………………………………………………………………………….…62 CCAC Referral Process………………………………………………………………………………………....63 CCAC Referral Form………………………………………………………………………………………….…64 Consent Health Link Consent Form……………………………………………………………………………...............65 -

Information & Bibliothek
DVD / Blu-Ray-Gesamtkatalog der Bibliothek / Catálogo Completo de DVDs e Blu-Rays da Biblioteca Abkürzungen / Abreviações: B = Buch / Roteiro; D = Darsteller / Atores; R = Regie / Diretor; UT = Untertitel / Legendas; dtsch. = deutsch / alemão; engl. = englisch / inglês; port. = portugiesisch / português; franz. = französisch / francês; russ. = russisch / russo; span. = spanisch / espanhol; chin. = chinesisch / chinês; jap. = japanisch / japonês; mehrsprach. = mehrsprachig / plurilingüe; M = Musiker / M úsico; Dir. = Dirigent / Regente; Inter. = Interprete / Intérprete; EST = Einheitssachtitel / Título Original; Zwischent. = Zwischentitel / Entretítulos ● = Audio + Untertitel deutsch / áudio e legendas em alemão Periodika / Periódicos ------------------------------- 05 Kub KuBus. - Bonn: Inter Nationes ● 68. Film 1: Eine Frage des Vertrauens - Die Auflösung des Deutschen Bundestags. Film 2: Stelen im Herzen Berlins - Das Denkmal für die ermordeten Juden Europas. - 2005. - DVD: 30 Min. : farb. ; dtsch., engl., franz., span., + mehrspr. Begleitbuch ; dtsch., russ., chin. UT ; NTSC ; V+Ö. (KuBus , 68) ● 69: Film 1: Im Vorwärtsgang - Frauenfußball in Deutschland. Film 2: Faktor X - Die Fraunhofer-Gesellschaft und die digitale Zukunft. - 2005.- DVD: 30 Min. : farb. ; dtsch., engl., franz., span., + mehrspr. Begleitbuch ; dtsch., russ., chin. UT ; NTSC ; V+Ö. (KuBus ; 69) ● 70. Film 1: Wie deutsch darf man singen? Film 2: Traumberuf Dirigentin. - 2006. - DVD: 30 Min. : farb. ; dtsch., engl., franz., span., + mehrspr. Begleitbuch ; dtsch., russ., chin. UT ; NTSC ; V+Ö. (KuBus ; 70) ● 71. Film 1: Der Maler Jörg Immendorff. Film 2: Der junge deutsche Jazz. - 2006. - DVD: 30 Min. : farb. ; dtsch., engl., franz., span., + mehrspr. Begleitbuch ; dtsch., russ., chin. UT ; NTSC ; V+Ö. (KuBus ; 71) ● 72. Film 1: Die Kunst des Bierbrauens. Film 2: Fortschritt unter der Karosserie. - 2006. - DVD: 30 Min. : farb. ; dtsch., engl., franz., span., + mehrspr. -

Learning from Ambiguously Labeled Images
University of Pennsylvania ScholarlyCommons Technical Reports (CIS) Department of Computer & Information Science January 2009 Learning From Ambiguously Labeled Images Timothee Cour University of Pennsylvania Benjamin Sapp University of Pennsylvania Chris Jordan University of Pennsylvania Ben Taskar University of Pennsylvania, [email protected] Follow this and additional works at: https://repository.upenn.edu/cis_reports Recommended Citation Timothee Cour, Benjamin Sapp, Chris Jordan, and Ben Taskar, "Learning From Ambiguously Labeled Images", . January 2009. University of Pennsylvania Department of Computer and Information Science Technical Report No. MS-CIS-09-07 This paper is posted at ScholarlyCommons. https://repository.upenn.edu/cis_reports/902 For more information, please contact [email protected]. Learning From Ambiguously Labeled Images Abstract In many image and video collections, we have access only to partially labeled data. For example, personal photo collections often contain several faces per image and a caption that only specifies who is in the picture, but not which name matches which face. Similarly, movie screenplays can tell us who is in the scene, but not when and where they are on the screen. We formulate the learning problem in this setting as partially-supervised multiclass classification where each instance is labeled ambiguously with more than one label. We show theoretically that effective learning is possible under reasonable assumptions even when all the data is weakly labeled. Motivated by the analysis, we propose a general convex learning formulation based on minimization of a surrogate loss appropriate for the ambiguous label setting. We apply our framework to identifying faces culled from web news sources and to naming characters in TV series and movies. -

Columbia Chronicle College Publications
Columbia College Chicago Digital Commons @ Columbia College Chicago Columbia Chronicle College Publications 10-11-1999 Columbia Chronicle (10/11/1999) Columbia College Chicago Follow this and additional works at: http://digitalcommons.colum.edu/cadc_chronicle Part of the Journalism Studies Commons This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. Recommended Citation Columbia College Chicago, "Columbia Chronicle (10/11/1999)" (October 11, 1999). Columbia Chronicle, College Publications, College Archives & Special Collections, Columbia College Chicago. http://digitalcommons.colum.edu/cadc_chronicle/436 This Book is brought to you for free and open access by the College Publications at Digital Commons @ Columbia College Chicago. It has been accepted for inclusion in Columbia Chronicle by an authorized administrator of Digital Commons @ Columbia College Chicago. VOWME 33, NUMBER 3 COLUMBIA COLLEGE CHICAGO OCTOBER I I , I 999 CAMPUS VITALITY SPORTS Students get animated Columbia graduate scores Fall movie reviews over special-effects veteran on the airwaves PAGE3 INSIDE BACK PAGE Convo <jt~ first st eJS Th~EIVED Freshman ocr 1 2 1999 • COLUMBIA Re t en tkQJiLEGE LIBRARY DANIELLE HAAS Staff Writer Every year a new group of freshman enter Columbia ready, will ing and able to take on what we all know is not character istically your typical school. This year the start of their career here wi ll be marked with a New Student Convocation on Friday, Oct. 15. "The New Student Convocation is a very typical event at most colleges. It is a cere monial assembly where new students are Students design divine bovine we lcomed to the college. -

10 Lost Wanted
Wanted updated 03-12-13 LOST Season 1 Missing: Oceanic 815 Puzzle Cards (1:11 packs) M1 Charlie: Get it? Hurley: Dude, quit asking me Walkabout M3 Claire: I'm having contractions. Jack: How man Pilot Pt. 1 M4 Jack: Come on. Come on! Come on! Come on! Big Pilot Pt. 1 M5 Jack: We must have been at about forth thousan Pilot Pt. 1 M6 Michael: Hey, hey, where you going, man? Walt: Walkabout M7 Charlie: How does something like that happen? Pilot Pt. 1 M8 Pilot: Six hours in, our radio went out. No on Pilot Pt. 1 M9 Kate: Jack! Jack: There's someone else still o White Rabbit Numbers Die-Cut Cards (1:17 packs) 15 Sawyer: That what I think it is? Michael: Some Exodus, Pt. 2 23 Kate: I wanted you to make sure that Ray Mulle Tabula Rasa 42 Hurley: ...Stop! What are you doing?! Why'd yo Exodus, Pt. 2 Autograph Cards (1:36 packs) A-1 Evangeline Lilly as Kate Austen A-2 Josh Holloway as James "Sawyer" Ford A-3 Maggie Grace as Shannon Rutherford A-5 Mira Furlan as Danielle Rousseau A-6 William Mapother as Ethan Rom A-7 John Terry as Dr. Christian Shephard A-9 Daniel Roebuck as Dr. Leslie Arzt A-11 Kevin Tighe as Anthony Cooper A-12 Swoosie Kurtz as Emily Annabeth Locke AR1 (Redemption Card) Pieceworks Cards (1:36 packs) PW-1 Shirt worn by Evangeline Lilly as Kate Austen The Greater Good PW-2 T-shirt worn by Josh Holloway as Sawyer Ford Pilot PW-3 Top worn by Maggie Grace as Shannon Rutherford Hearts and Minds PW-4 T-shirt worn by Matthew Fox as Jack Shepherd All the Best Cowboys Have Daddy Issues PW-5 T-shirt worn by Dominic Monaghan as Charlie Pace Pilot PW-6 T-shirt worn by Terry O'Quinn as John Locke Numbers PW-8 T-shirt worn by Jorge Garcia as Hugo "Hurley" Reyes Hearts and Mind PW-10 Top worn by Yunjin Kim as Sun Kwon Exodus Pt. -

The Vilcek Foundation Celebrates a Showcase Of
THE VILCEK FOUNDATION CELEBRATES A SHOWCASE OF THE INTERNATIONAL ARTISTS AND FILMMAKERS OF ABC’S HIT SHOW EXHIBITION CATALOGUE BY EDITH JOHNSON Exhibition Catalogue is available for reference inside the gallery only. A PDF version is available by email upon request. Props are listed in the Exhibition Catalogue in the order of their appearance on the television series. CONTENTS 1 Sun’s Twinset 2 34 Two of Sun’s “Paik Industries” Business Cards 22 2 Charlie’s “DS” Drive Shaft Ring 2 35 Juliet’s DHARMA Rum Bottle 23 3 Walt’s Spanish-Version Flash Comic Book 3 36 Frozen Half Wheel 23 4 Sawyer’s Letter 4 37 Dr. Marvin Candle’s Hard Hat 24 5 Hurley’s Portable CD/MP3 Player 4 38 “Jughead” Bomb (Dismantled) 24 6 Boarding Passes for Oceanic Airlines Flight 815 5 39 Two Hieroglyphic Wall Panels from the Temple 25 7 Sayid’s Photo of Nadia 5 40 Locke’s Suicide Note 25 8 Sawyer’s Copy of Watership Down 6 41 Boarding Passes for Ajira Airways Flight 316 26 9 Rousseau’s Music Box 6 42 DHARMA Security Shirt 26 10 Hatch Door 7 43 DHARMA Initiative 1977 New Recruits Photograph 27 11 Kate’s Prized Toy Airplane 7 44 DHARMA Sub Ops Jumpsuit 28 12 Hurley’s Winning Lottery Ticket 8 45 Plutonium Core of “Jughead” (and sling) 28 13 Hurley’s Game of “Connect Four” 9 46 Dogen’s Costume 29 14 Sawyer’s Reading Glasses 10 47 John Bartley, Cinematographer 30 15 Four Virgin Mary Statuettes Containing Heroin 48 Roland Sanchez, Costume Designer 30 (Three intact, one broken) 10 49 Ken Leung, “Miles Straume” 30 16 Ship Mast of the Black Rock 11 50 Torry Tukuafu, Steady Cam Operator 30 17 Wine Bottle with Messages from the Survivor 12 51 Jack Bender, Director 31 18 Locke’s Hunting Knife and Sheath 12 52 Claudia Cox, Stand-In, “Kate 31 19 Hatch Painting 13 53 Jorge Garcia, “Hugo ‘Hurley’ Reyes” 31 20 DHARMA Initiative Food & Beverages 13 54 Nestor Carbonell, “Richard Alpert” 31 21 Apollo Candy Bars 14 55 Miki Yasufuku, Key Assistant Locations Manager 32 22 Dr. -

From William Golding's Lord of the Flies to ABC's LOST. By
Humanity Square One: From William Golding’s Lord of the Flies to ABC’s LOST. by Antonia Iliadou A dissertation to the Department of American Literature and Culture, School of English, Faculty of Philosophy of Aristotle University of Thessaloniki, in partial fulfillment of the requirements for the degree of Master of Arts. Aristotle University of Thessaloniki September 2013 Humanity Square One: From William Golding’s Lord of the Flies to ABC’s LOST. by Antonia Iliadou Has been approved September 2013 APPROVED: _________________________ _________________________ _________________________ Supervisory Committee ACCEPTED: _______________ Department Chairperson Iliadou 1 CONTENTS ACKNOWLEDGEMENTS .......................................................................................................1 ABSTRACT...............................................................................................................................3 INTRODUCTION......................................................................................................................5 CHAPTER 1: William Golding’s Lord of the Flies: Analysis and Contextualization ..............1 1.1. a. Lord of the Flies in an age of ambiguity: The position of Golding’s novel in the Post War United States...........................................................................................................2 1.1. b. The Impact of Golding’s Lord of the Flies on its Readers........................................14 1.2. “… The picture of man, at once heroic and sick”: The Depiction -
Nidevtip OWNSMAN
'Three i- nothing wrong "Ir ;con nigh to avoid for- the iinichinery of the nit„ D'L eign collision, you had better H EAD United Nation• except the „,H.„ abandon the ocean." “. CL.V1' m. —TRVGVE LIE In order time for NIDeVtip OWNSMAN NUMBER 29 ening, or VOLUME 60, ANDOVER, MASSACHUSETTS, APRIL 29, 1948 PRICE, 5 CENTS In ahead retiring Daylight VIEWS Two Teachers Elected Call Town Meeting To Act On In 1 Slinday OF To School Department Miss Luella M. Dunning and Mrs. Louise B. Low Rent Homes For Veterans • THE McQueston Appointed To Fill Vacancies Special Session May 18 To Decide Two new teachers were elected the annual department have had several years' to the Andover school department Primaries Id Saturday, teaching experience. Upon Accepting Housing Authority NEWS at a special meeting of the school rooms from Miss Dunning comes to Andover A special town meeting for direct cost or loss to the com- By LEONARD F. JAMES committee Monday night. Draw Only 'n completed with a wealth of background, train- Tuesday evening, May 18, in the munity, but a small appropriation Miss Luella M. Dunning was %Ion Auxil- The mere passage of a law ing and experience. She graduated 103 To Polls Municipal auditorium has been of $50 0 will be asked, If adopted elected to take the place of Mrs. from the State Teachers College, May be ob. does not necessarily solve a called by the Board of Selectmen here, to cover incidental ex- Emma G. Carter who has accepted DeKalb, Illinois, received her Bach- a Mules, 65 problem. -
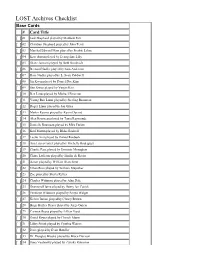
LOST Archives Checklist
LOST Archives Checklist Base Cards # Card Title [ ] 01 Jack Shephard played by Matthew Fox [ ] 02 Christian Shephard played by John Terry [ ] 03 Marshal Edward Mars played by Fredric Lehne [ ] 04 Kate Austin played by Evangeline Lilly [ ] 05 Diane Janssen played by Beth Broderick [ ] 06 Bernard Nadler played by Sam Anderson [ ] 07 Rose Nadler played by L. Scott Caldwell [ ] 08 Jin Kwon played by Daniel Dae Kim [ ] 09 Sun Kwon played by Yunjin Kim [ ] 10 Ben Linus played by Michael Emerson [ ] 11 Young Ben Linus played by Sterling Beaumon [ ] 12 Roger Linus played by Jon Gries [ ] 13 Martin Keamy played by Kevin Durand [ ] 14 Alex Rousseau played by Tania Raymonde [ ] 15 Danielle Rousseau played by Mira Furlan [ ] 16 Karl Martin played by Blake Bashoff [ ] 17 Leslie Arzt played by Daniel Roebuck [ ] 18 Ana Lucia Cortez played by Michelle Rodriguez [ ] 19 Charlie Pace played by Dominic Monaghan [ ] 20 Claire Littleton played by Emilie de Ravin [ ] 21 Aaron played by William Blanchette [ ] 22 Ethan Rom played by William Mapother [ ] 23 Zoe played by Sheila Kelley [ ] 24 Charles Widmore played by Alan Dale [ ] 25 Desmond Hume played by Henry Ian Cusick [ ] 26 Penelope Widmore played by Sonya Walger [ ] 27 Kelvin Inman played by Clancy Brown [ ] 28 Hugo Hurley Reyes played by Jorge Garcia [ ] 29 Carmen Reyes played by Lillian Hurst [ ] 30 David Reyes played by Cheech Marin [ ] 31 Libby Smith played by Cynthia Watros [ ] 32 Dave played by Evan Handler [ ] 33 Dr. Douglas Brooks played by Bruce Davison [ ] 34 Ilana Verdansky played by Zuleika -

Redalyc.Rose: Uma Ilha De Estereótipos Em Lost
Significação: revista de cultura audiovisual E-ISSN: 2316-7114 [email protected] Universidade de São Paulo Brasil de Almeida, Rogério; Pelegrini, Christian H. Rose: uma ilha de estereótipos em Lost Significação: revista de cultura audiovisual, vol. 40, núm. 39, enero-junio, 2013, pp. 243- 265 Universidade de São Paulo São Paulo, Brasil Disponível em: http://www.redalyc.org/articulo.oa?id=609765999013 Como citar este artigo Número completo Sistema de Informação Científica Mais artigos Rede de Revistas Científicas da América Latina, Caribe , Espanha e Portugal Home da revista no Redalyc Projeto acadêmico sem fins lucrativos desenvolvido no âmbito da iniciativa Acesso Aberto // Rose: uma ilha de estereótipos em Lost /////////////////// Rogério de Almeida1 Christian H. Pelegrini2 1. Doutor em educação pela Universidade de São Paulo. Professor da Faculdade de Educação da USP e pesquisador do Geifec (Grupo de Estudos sobre Itinerários de Formação em Educação e Cultura). E-mail: [email protected] 2. Doutorando na Escola de Comunicações e Artes da Universidade de São Paulo, professor dos cursos de comunicação social da Pontifícia Universidade Católica de São Paulo e da Universidade São Judas Tadeu e pesquisador do Geifec. E-mail: [email protected] 2013 | ano 40 | nº39 | significação | 243 /////////////////////////////////////////////////////////////////////////////////////////// Resumo Este artigo é resultado de pesquisas realizadas pelo Geifec (Grupo de Estudos sobre Itinerários de Formação em Educação e Cultura) e tem por objetivo a análise das formas de representação da personagem Rose Nadler, da série americana Lost. Mulher, negra, próxima dos 60 anos, acima do peso, Rose está na intersecção de uma série de grupos minoritários, e sua presença na tela incorre na sobreposição de estereótipos pouco comuns na série. -
History of Fanny Fern Miller Poor
HISTORY OF FANNY FERN MILLER POOR By LeGrande C. Poor My mother, Fanny Fern Miller Poor was a remarkable woman. She was loved by everyone. In the community of Herriman, where she was born and raised and where she died, she was Aunt Fern to everyone. Her grandson, Lindsay Thomas, moved to Herriman to live a number of years ago. He said that many people told him how much they loved and appreciated his grandmother. Early in her life, as a result of a bout with whooping cough she lost much of her hearing. In spite of that she raised four children. Although hard of hearing she was able to hear her children when she needed to when we were babies. In her history she recounts the problems she had in being unable to hear. I recall when attending a movie we would ask her if she could hear it and her answer always was, “Pretty good”. We never went to a movie or any other activity when the car wasn’t filled with other kids, usually her nieces and nephews. Having lunch at her place was an excursion. She would make a lunch and then we would go to the top of our lot, under the trees or bushes and have a picnic. We would also go to my grandfather’s farm for a picnic. My mother’s favorite candy bar was Mounds. During World War II I was stationed in California and prior to being shipped out I came home on leave and brought Mom a box of Mound candy bars.