A Morphometric Anatomical Study of the Ethmoidal Foramina on Dry Human Skulls Anatomy Section
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MR Imaging of the Orbital Apex
J Korean Radiol Soc 2000;4 :26 9-0 6 1 6 MR Imaging of the Orbital Apex: An a to m y and Pat h o l o g y 1 Ho Kyu Lee, M.D., Chang Jin Kim, M.D.2, Hyosook Ahn, M.D.3, Ji Hoon Shin, M.D., Choong Gon Choi, M.D., Dae Chul Suh, M.D. The apex of the orbit is basically formed by the optic canal, the superior orbital fis- su r e , and their contents. Space-occupying lesions in this area can result in clinical d- eficits caused by compression of the optic nerve or extraocular muscles. Even vas c u l a r changes in the cavernous sinus can produce a direct mass effect and affect the orbit ap e x. When pathologic changes in this region is suspected, contrast-enhanced MR imaging with fat saturation is very useful. According to the anatomic regions from which the lesions arise, they can be classi- fied as belonging to one of five groups; lesions of the optic nerve-sheath complex, of the conal and intraconal spaces, of the extraconal space and bony orbit, of the cav- ernous sinus or diffuse. The characteristic MR findings of various orbital lesions will be described in this paper. Index words : Orbit, diseases Orbit, MR The apex of the orbit is a complex region which con- tains many nerves, vessels, soft tissues, and bony struc- Anatomy of the orbital apex tures such as the superior orbital fissure and the optic canal (1-3), and is likely to be involved in various dis- The orbital apex region consists of the optic nerve- eases (3). -
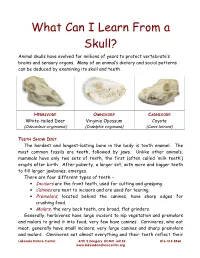
What Can I Learn from a Skull? Animal Skulls Have Evolved for Millions of Years to Protect Vertebrate’S Brains and Sensory Organs
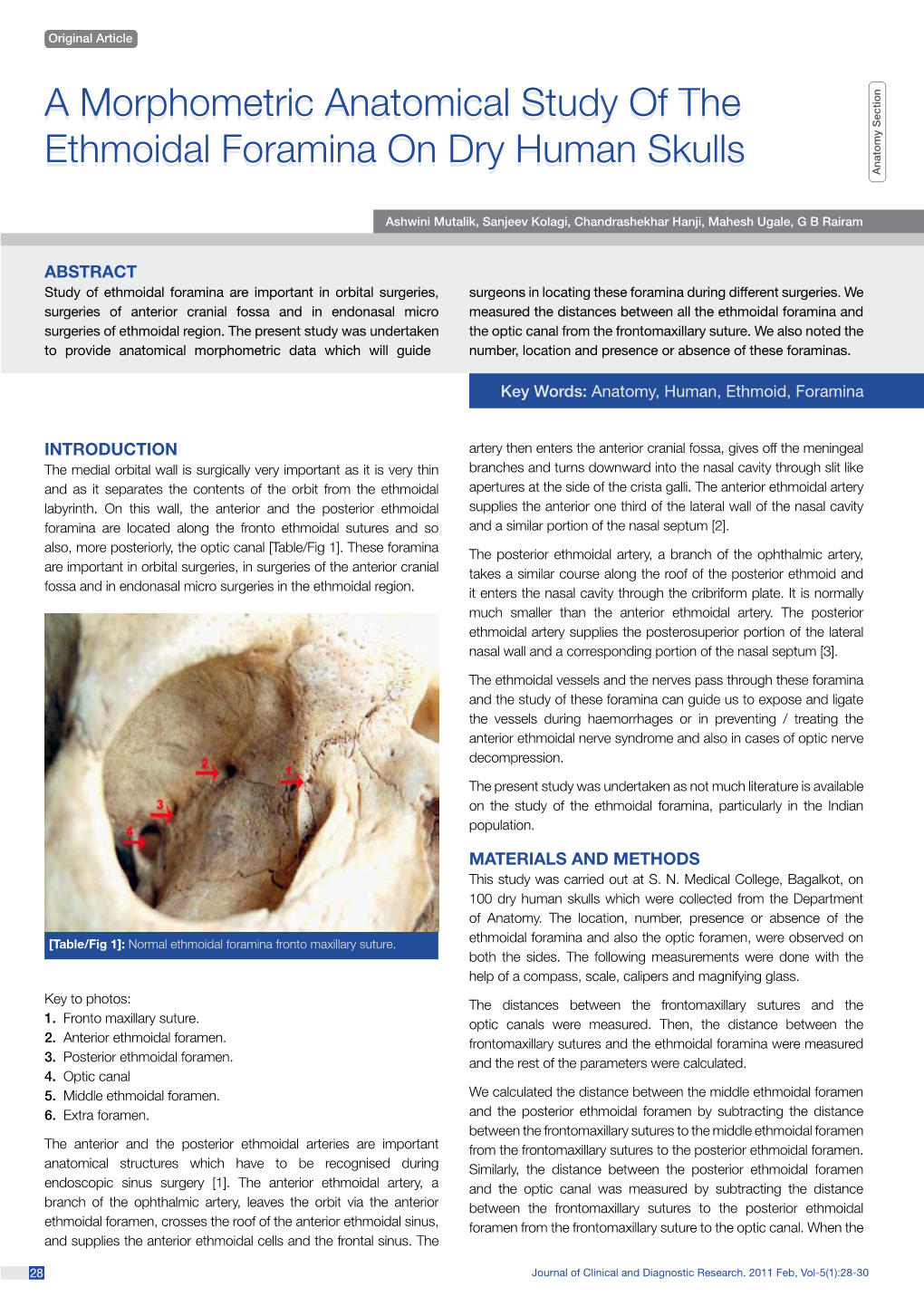
What Can I Learn From a Skull? Animal skulls have evolved for millions of years to protect vertebrate’s brains and sensory organs. Many of an animal’s dietary and social patterns can be deduced by examining its skull and teeth. HERBIVORE OMNIVORE CARNIVORE White-tailed Deer Virginia Opossum Coyote (Odocoileus virginianus) (Didelphis virginiana) (Canis latrans) TEETH SHOW DIET . The hardest and longest-lasting bone in the body is tooth enamel. The most common fossils are teeth, followed by jaws. Unlike other animals, mammals have only two sets of teeth, the first (often called ‘milk teeth’) erupts after birth. After puberty, a larger set, with more and bigger teeth to fill larger jawbones, emerges. There are four different types of teeth – • Incisors are the front teeth, used for cutting and grasping. • Canines are next to incisors and are used for tearing. • Premolars , located behind the canines, have sharp edges for crushing food. • Molars , the very back teeth, are broad, flat grinders. Generally, herbivores have large incisors to nip vegetation and premolars and molars to grind it into food; very few have canines. Carnivores, who eat meat, generally have small incisors, very large canines and sharp premolars and molars. Omnivores eat almost everything and their teeth reflect their Lakeside Nature Center 4701 E Gregory, KCMO 64132 816-513-8960 www.lakesidenaturecenter.org preferences; they have all four types of teeth. In fact, if you’d like to see an excellent example of an omnivore’s teeth, look in the mirror. EYE PLACEMENT IDENTIFIES PREDATORS . Carnivores generally have large eyes, placed so that the eyes look forward and the areas of vision of the two eyes overlap. -

Nerves of the Orbit Optic Nerve the Optic Nerve Enters the Orbit from the Middle Cranial Fossa by Passing Through the Optic Canal
human anatomy 2016 lecture fourteen Dr meethak ali ahmed neurosurgeon Nerves of the Orbit Optic Nerve The optic nerve enters the orbit from the middle cranial fossa by passing through the optic canal . It is accompanied by the ophthalmic artery, which lies on its lower lateral side. The nerve is surrounded by sheath of pia mater, arachnoid mater, and dura mater. It runs forward and laterally within the cone of the recti muscles and pierces the sclera at a point medial to the posterior pole of the eyeball. Here, the meninges fuse with the sclera so that the subarachnoid space with its contained cerebrospinal fluid extends forward from the middle cranial fossa, around the optic nerve, and through the optic canal, as far as the eyeball. A rise in pressure of the cerebrospinal fluid within the cranial cavity therefore is transmitted to theback of the eyeball. Lacrimal Nerve The lacrimal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward along the upper border of the lateral rectus muscle . It is joined by a branch of the zygomaticotemporal nerve, whi(parasympathetic secretomotor fibers). The lacrimal nerve ends by supplying the skin of the lateral part of the upper lid. Frontal Nerve The frontal nerve arises from the ophthalmic division of the trigeminal nerve. It enters the orbit through the upper part of the superior orbital fissure and passes forward on the upper surface of the levator palpebrae superioris beneath the roof of the orbit . -

Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: a Case Report
E CASE REPORT Maxillary Nerve-Mediated Postseptoplasty Nasal Allodynia: A Case Report Shikha Sharma, MD, PhD,* Wilson Ly, MD, PharmD,* and Xiaobing Yu, MD*† Endoscopic nasal septoplasty is a commonly performed otolaryngology procedure, not known to cause persistent postsurgical pain or hypersensitivity. Here, we discuss a unique case of persis- tent nasal pain that developed after a primary endoscopic septoplasty, which then progressed to marked mechanical and thermal allodynia following a revision septoplasty. Pain symptoms were found to be mediated by the maxillary division of the trigeminal nerve and resolved after percuta- neous radiofrequency ablation (RFA) of bilateral maxillary nerves. To the best of our knowledge, this is the first report of maxillary nerve–mediated nasal allodynia after septoplasty. (A&A Practice. 2020;14:e01356.) GLOSSARY CT = computed tomography; FR = foramen rotundum; HIPAA = Health Insurance Portability and Accountability Act; ION = infraorbital nerve; LPP = lateral pterygoid plate; MRI = magnetic reso- nance imaging; RFA = radiofrequency ablation; SPG = sphenopalatine ganglion; US = ultrasound ndoscopic nasal septoplasty is a common otolaryn- septoplasty for chronic nasal obstruction with resection of gology procedure with rare incidence of postsurgical the cartilage inferiorly and posteriorly in 2010. Before this Ecomplications. Minor complications include epistaxis, surgery, the patient only occasionally experienced mild septal hematoma, septal perforation, cerebrospinal fluid leak, headaches. However, his postoperative course was compli- and persistent obstruction.1 Numbness or hypoesthesia of the cated by significant pain requiring high-dose opioids. After anterior palate, secondary to injury to the nasopalatine nerve, discharge, patient continued to have persistent deep, “ach- has been reported, but is usually rare and temporary, resolv- ing” nasal pain which radiated toward bilateral forehead ing over weeks to months.2 Acute postoperative pain is also and incisors. -

Craniotomy for Anterior Cranial Fossa Meningiomas: Historical Overview
Neurosurg Focus 36 (4):E14, 2014 ©AANS, 2014 Craniotomy for anterior cranial fossa meningiomas: historical overview SAUL F. MORALES-VALERO, M.D., JAMIE J. VAN GOMPEL, M.D., IOANNIS LOUMIOTIS, M.D., AND GIUSEPPE LANZINO, M.D. Department of Neurologic Surgery, Mayo Clinic, Mayo Medical School, Rochester, Minnesota The surgical treatment of meningiomas located at the base of the anterior cranial fossa is often challenging, and the evolution of the surgical strategy to resect these tumors parallels the development of craniotomy, and neurosur- gery in general, over the past century. Early successful operations to treat these tumors were pioneered by prominent figures such as Sir William Macewen and Francesco Durante. Following these early reports, Harvey Cushing made significant contributions, allowing a better understanding and treatment of meningiomas in general, but particularly those involving the anterior cranial base. Initially, large-sized unilateral or bilateral craniotomies were necessary to approach these deep-seated lesions. Technical advances such as the introduction of electrosurgery, the operating microscope, and refined microsurgical instruments allowed neurosurgeons to perform less invasive surgical proce- dures with better results. Today, a wide variety of surgical strategies, including endoscopic surgery and radiosurgery, are used to treat these tumors. In this review, the authors trace the evolution of craniotomy for anterior cranial fossa meningiomas. (http://thejns.org/doi/abs/10.3171/2014.1.FOCUS13569) KEY WORDS • intracranial meningiomas • craniotomy • history • anterior cranial fossa ENINGIOMAS of the anterior cranial fossa represent has a few distinct clinical features. However, in practice, 12%–20% of all intracranial meningiomas.5,30 this group of tumors often represents a continuum. -

Ardipithecus Ramidus and the Evolution of the Human Cranial Base
Ardipithecus ramidus and the evolution of the human cranial base William H. Kimbela,1, Gen Suwab, Berhane Asfawc, Yoel Raka,d, and Tim D. Whitee,1 aInstitute of Human Origins and School of Human Evolution and Social Change, Arizona State University, Tempe, AZ 85287; bThe University Museum, University of Tokyo, Bunkyo-ku, Tokyo 113-0033, Japan; cRift Valley Research Service, Addis Ababa, Ethiopia; dDepartment of Anatomy and Anthropology, Sackler School of Medicine, Tel Aviv University, 69978 Ramat Aviv, Israel; and eDepartment of Integrative Biology, Human Evolution Research Center, University of California, Berkeley, CA 94720 Contributed by Tim D. White, December 5, 2013 (sent for review October 14, 2013) The early Pliocene African hominoid Ardipithecus ramidus was di- We report here results of a metrical and morphological study agnosed as a having a unique phylogenetic relationship with the of the Ar. ramidus basicranium as another test of its hypothesized Australopithecus + Homo clade based on nonhoning canine teeth, phylogenetic affinity with Australopithecus and Homo. We ana- a foreshortened cranial base, and postcranial characters related to lyzed the length and breadth of the external cranial base and the facultative bipedality. However, pedal and pelvic traits indicating structural relationship between the petrous and tympanic elements substantial arboreality have raised arguments that this taxon may of the temporal bone in Ar. ramidus, Australopithecus (including instead be an example of parallel evolution of human-like traits Paranthropus of some authors), and mixed-sex samples of extant among apes around the time of the chimpanzee–human split. Here African hominoid (Gorilla gorilla, Pan troglodytes, Pan paniscus) we investigated the basicranial morphology of Ar. -

Septation of the Sphenoid Sinus and Its Clinical Significance
1793 International Journal of Collaborative Research on Internal Medicine & Public Health Septation of the Sphenoid Sinus and its Clinical Significance Eldan Kapur 1* , Adnan Kapidžić 2, Amela Kulenović 1, Lana Sarajlić 2, Adis Šahinović 2, Maida Šahinović 3 1 Department of anatomy, Medical faculty, University of Sarajevo, Čekaluša 90, 71000 Sarajevo, Bosnia and Herzegovina 2 Clinic for otorhinolaryngology, Clinical centre University of Sarajevo, Bolnička 25, 71000 Sarajevo, Bosnia and Herzegovina 3 Department of histology and embriology, Medical faculty, University of Sarajevo, Čekaluša 90, 71000 Sarajevo, Bosnia and Herzegovina * Corresponding Author: Eldan Kapur, MD, PhD Department of anatomy, Medical faculty, University of Sarajevo, Bosnia and Herzegovina Email: [email protected] Phone: 033 66 55 49; 033 22 64 78 (ext. 136) Abstract Introduction: Sphenoid sinus is located in the body of sphenoid, closed with a thin plate of bone tissue that separates it from the important structures such as the optic nerve, optic chiasm, cavernous sinus, pituitary gland, and internal carotid artery. It is divided by one or more vertical septa that are often asymmetric. Because of its location and the relationships with important neurovascular and glandular structures, sphenoid sinus represents a great diagnostic and therapeutic challenge. Aim: The aim of this study was to assess the septation of the sphenoid sinus and relationship between the number and position of septa and internal carotid artery in the adult BH population. Participants and Methods: A retrospective study of the CT analysis of the paranasal sinuses in 200 patients (104 male, 96 female) were performed using Siemens Somatom Art with the following parameters: 130 mAs: 120 kV, Slice: 3 mm. -

A Forensic Case Report
Skeletonized body identified by analysis of frontal sinus morphology and characteristics of osteosynthesis material: a forensic case report Rhonan Ferreira-Silva1, Andréa Pinheiro de- Abreu Meirelles2, Isabela Machado3, Lívia Graziele Rodrigues4, Roberta Gomes-Resende5, Alicia Picapedra6, Carlos Sassi7 DOI: 10.22592/ode2018n31a10 Abstract Forensic dentistry is essential for the identification of highly decomposed and charred bodies, as well as skeletal remains. This study reports a case of human identification by analyzing the morphology of the frontal sinuses and osteosynthesis material. In the anthropological assess- ment of skeletal remains a surgical plate used for osteosynthesis was detected in the periorbital regions. Relatives of the potential victim provided ante-mortem (AM) radiographs which re- vealed the presence of an osteosynthesis plate. Post-mortem (PM) imaging exams were per- formed to reproduce the AM data. Similarities were observed between the AM and PM radio- graphs, especially regarding the morphology of the frontal sinuses and the position and outline of the surgical plate used for osteosynthesis. The comparison of AM and PM images made it possible to identify the victim and to aid the criminal investigation. It also highlighted the role of radiographs and anatomical characteristics in the process of human identification. Keywords: forensic dentistry, forensic anthropology, frontal sinus, radiography. 1 Professor of Forensic Dentistry, School of Dentistry, Universidad Federal de Goiás. Criminal Expert at the Scientific Police of Goiás (Goiânia, Goiás, Brazil). ORCID: 0000-0002-3680-7020 2 Undergraduate Student, School of Dentistry, Universidad Federal de Goiás (Goiânia, Goiás, Brazil). ORCID: 0000-0002-1290-3755 3 Undergraduate Student, School of Dentistry, Universidad Federal de Goiás (Goiânia, Goiás, Brazil). -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

Simple Ways to Dissect Ciliary Ganglion for Orbital Anatomical Education
OkajimasDetection Folia Anat. of ciliary Jpn., ganglion94(3): 119–124, for orbit November, anatomy 2017119 Simple ways to dissect ciliary ganglion for orbital anatomical education By Ming ZHOU, Ryoji SUZUKI, Hideo AKASHI, Akimitsu ISHIZAWA, Yoshinori KANATSU, Kodai FUNAKOSHI, Hiroshi ABE Department of Anatomy, Akita University Graduate School of Medicine, Akita, 010-8543 Japan –Received for Publication, September 21, 2017– Key Words: ciliary ganglion, orbit, human anatomy, anatomical education Summary: In the case of anatomical dissection as part of medical education, it is difficult for medical students to find the ciliary ganglion (CG) since it is small and located deeply in the orbit between the optic nerve and the lateral rectus muscle and embedded in the orbital fat. Here, we would like to introduce simple ways to find the CG by 1): tracing the sensory and parasympathetic roots to find the CG from the superior direction above the orbit, 2): transecting and retracting the lateral rectus muscle to visualize the CG from the lateral direction of the orbit, and 3): taking out whole orbital structures first and dissecting to observe the CG. The advantages and disadvantages of these methods are discussed from the standpoint of decreased laboratory time and students as beginners at orbital anatomy. Introduction dissection course for the first time and with limited time. In addition, there are few clear pictures in anatomical The ciliary ganglion (CG) is one of the four para- textbooks showing the morphology of the CG. There are sympathetic ganglia in the head and neck region located some scientific articles concerning how to visualize the behind the eyeball between the optic nerve and the lateral CG, but they are mostly based on the clinical approaches rectus muscle in the apex of the orbit (Siessere et al., rather than based on the anatomical procedure for medical 2008). -

Benign Tumors of the Frontal Sinuses with and Fibro-Osseous Tumors of the Frontal Sinus: Their Propensity to Recur and Cause Local Open Approaches
Chapter 18 Benign Tumors 18 of the Frontal Sinuses Brent A. Senior, Marc G. Dubin Management of Benign Lesions of the Frontal Sinus . 157 Core Messages Preoperative Evaluation . 157 í Surgical Treatment of Bony Benign tumors of the frontal sinuses with and Fibro-osseous Tumors of the Frontal Sinus: their propensity to recur and cause local Open Approaches . 157 injury present unique challenges to the Surgical Treatment of Bony otolaryngologist and Fibro-osseous Tumors of the Frontal Sinus: Endoscopic Approaches . 158 í Fibro-osseous lesions may be managed ex- Cases: Fibro-osseus Lesions of the Frontal Sinus . 159 pectantly, or may be removed in the setting Case 1: Endoscopic Resection of Tumor of symptomatic pathology such as cosmet- in the Frontal Recess . 159 ic or functional deformity Case 2: Open Resection of Tumor of the Frontal Sinus . 160 í Inverted papillomas with their high rate of Surgical Management of Inverted Papilloma: associated malignancy should be complete- Open and Endoscopic . 161 ly removed Cases: Inverted Papilloma of the Frontal Sinus . 161 Case 1: Recurrent Inverted Papilloma of the Frontal Sinus . 161 í Tumors that in the past required open ap- proaches may now be managed successful- Postoperative Considerations . 162 ly with endoscopic approaches alone or Conclusions . 163 with combined approaches, lowering over- References . 163 all morbidity while not sacrificing outcome í Cases must be individually assessed in or- der to determine the appropriate manage- ment approach Introduction Management of disease of the frontal recess and frontal sinus is one of the greatest challenges in rhi- nology. Despite advances in the understanding of the Contents anatomy and physiology of this area along with in- creased comfort with endoscopic techniques, man- Introduction . -

The Ophthalmic Artery Ii
Brit. J. Ophthal. (1962) 46, 165. THE OPHTHALMIC ARTERY II. INTRA-ORBITAL COURSE* BY SOHAN SINGH HAYREHt AND RAMJI DASS Government Medical College, Patiala, India Material THIS study was carried out in 61 human orbits obtained from 38 dissection- room cadavers. In 23 cadavers both the orbits were examined, and in the remaining fifteen only one side was studied. With the exception of three cadavers of children aged 4, 11, and 12 years, the specimens were from old persons. Method Neoprene latex was injected in situ, either through the internal carotid artery or through the most proximal part of the ophthalmic artery, after opening the skull and removing the brain. The artery was first irrigated with water. After injection the part was covered with cotton wool soaked in 10 per cent. formalin for from 24 to 48 hours to coagulate the latex. The roof of the orbit was then opened and the ophthalmic artery was carefully studied within the orbit. Observations COURSE For descriptive purposes the intra-orbital course of the ophthalmic artery has been divided into three parts (Singh and Dass, 1960). (1) The first part extends from the point of entrance of the ophthalmic artery into the orbit to the point where the artery bends to become the second part. This part usually runs along the infero-lateral aspect of the optic nerve. (2) The second part crosses over or under the optic nerve running in a medial direction from the infero-lateral to the supero-medial aspect of the nerve. (3) The thirdpart extends from the point at which the second part bends at the supero-medial aspect of the optic nerve to its termination.