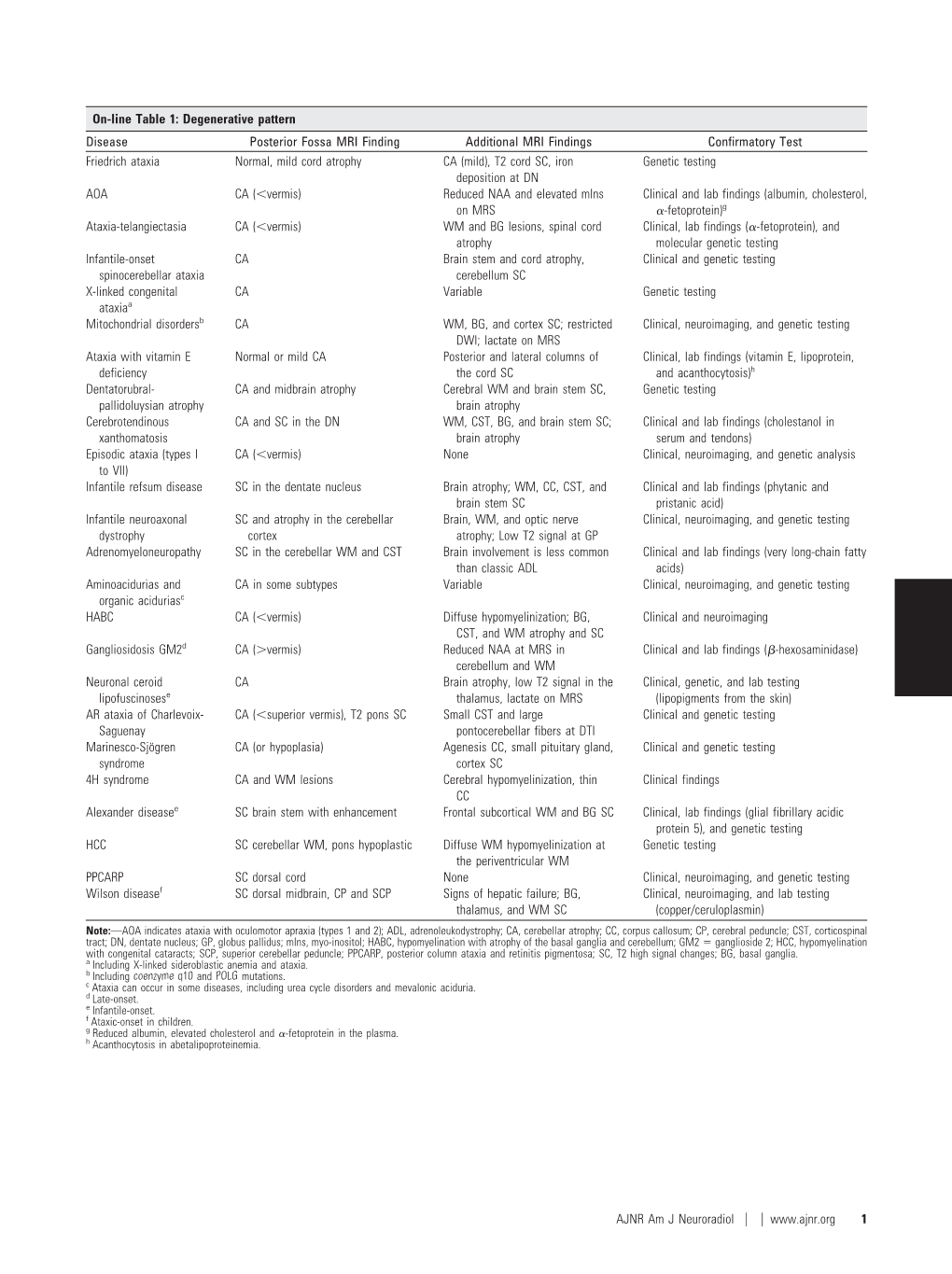
On-Line Table 1: Degenerative Pattern Disease Posterior Fossa MRI
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inherited Cerebellar Ataxia in Childhood: a Pattern-Recognition Approach Using Brain MRI
REVIEW ARTICLE Inherited Cerebellar Ataxia in Childhood: A Pattern-Recognition Approach Using Brain MRI L. Vedolin, G. Gonzalez, C.F. Souza, C. Lourenc¸o, and A.J. Barkovich ABSTRACT SUMMARY: Ataxia is the principal symptom of many common neurologic diseases in childhood. Ataxias caused by dysfunction of the cerebellum occur in acute, intermittent, and progressive disorders. Most of the chronic progressive processes are secondary to degen- erative and metabolic diseases. In addition, congenital malformation of the midbrain and hindbrain can also be present, with posterior fossa symptoms related to ataxia. Brain MR imaging is the most accurate imaging technique to investigate these patients, and imaging abnormalities include size, shape, and/or signal of the brain stem and/or cerebellum. Supratentorial and cord lesions are also common. This review will discuss a pattern-recognition approach to inherited cerebellar ataxia in childhood. The purpose is to provide a comprehensive discussion that ultimately could help neuroradiologists better manage this important topic in pediatric neurology. ABBREVIATIONS: AR ϭ autosomal recessive; CAC ϭ cerebellar ataxia in childhood; 4H ϭ hypomyelination with hypogonadotropic hypogonadism and hypodon- tia; JSRD ϭ Joubert syndrome and related disorders; OPHN1 ϭ oligophrenin-1 taxia is an inability to coordinate voluntary muscle move- plastic/paraneoplastic disorders, immune-mediated/demyelinat- Aments that cannot be attributed to weakness or involuntary ing disorders, and drugs/toxins (antiepileptic medications, -

Hyperplasia (Growth Factors
Adaptations Robbins Basic Pathology Robbins Basic Pathology Robbins Basic Pathology Coagulation Robbins Basic Pathology Robbins Basic Pathology Homeostasis • Maintenance of a steady state Adaptations • Reversible functional and structural responses to physiologic stress and some pathogenic stimuli • New altered “steady state” is achieved Adaptive responses • Hypertrophy • Altered demand (muscle . hyper = above, more activity) . trophe = nourishment, food • Altered stimulation • Hyperplasia (growth factors, . plastein = (v.) to form, to shape; hormones) (n.) growth, development • Altered nutrition • Dysplasia (including gas exchange) . dys = bad or disordered • Metaplasia . meta = change or beyond • Hypoplasia . hypo = below, less • Atrophy, Aplasia, Agenesis . a = without . nourishment, form, begining Robbins Basic Pathology Cell death, the end result of progressive cell injury, is one of the most crucial events in the evolution of disease in any tissue or organ. It results from diverse causes, including ischemia (reduced blood flow), infection, and toxins. Cell death is also a normal and essential process in embryogenesis, the development of organs, and the maintenance of homeostasis. Two principal pathways of cell death, necrosis and apoptosis. Nutrient deprivation triggers an adaptive cellular response called autophagy that may also culminate in cell death. Adaptations • Hypertrophy • Hyperplasia • Atrophy • Metaplasia HYPERTROPHY Hypertrophy refers to an increase in the size of cells, resulting in an increase in the size of the organ No new cells, just larger cells. The increased size of the cells is due to the synthesis of more structural components of the cells usually proteins. Cells capable of division may respond to stress by undergoing both hyperrtophy and hyperplasia Non-dividing cell increased tissue mass is due to hypertrophy. -

Reportable BD Tables Apr2019.Pdf
April 2019 Georgia Department of Public Health | Division of Health Protection | Maternal and Child Health Epidemiology Unit Reportable Birth Defects with ICD-10-CM Codes Reportable Birth Defects in Georgia with ICD-10-CM Diagnosis Codes Table D.1 Brain Malformations and Neural Tube Defects ICD-10-CM Diagnosis Codes Birth Defect ICD-10-CM 1. Brain Malformations and Neural Tube Defects Q00-Q05, Q07 Anencephaly Q00.0 Craniorachischisis Q00.1 Iniencephaly Q00.2 Frontal encephalocele Q01.0 Nasofrontal encephalocele Q01.1 Occipital encephalocele Q01.2 Encephalocele of other sites Q01.8 Encephalocele, unspecified Q01.9 Microcephaly Q02 Malformations of aqueduct of Sylvius Q03.0 Atresia of foramina of Magendie and Luschka (including Dandy-Walker) Q03.1 Other congenital hydrocephalus (including obstructive hydrocephaly) Q03.8 Congenital hydrocephalus, unspecified Q03.9 Congenital malformations of corpus callosum Q04.0 Arhinencephaly Q04.1 Holoprosencephaly Q04.2 Other reduction deformities of brain Q04.3 Septo-optic dysplasia of brain Q04.4 Congenital cerebral cyst (porencephaly, schizencephaly) Q04.6 Other specified congenital malformations of brain (including ventriculomegaly) Q04.8 Congenital malformation of brain, unspecified Q04.9 Cervical spina bifida with hydrocephalus Q05.0 Thoracic spina bifida with hydrocephalus Q05.1 Lumbar spina bifida with hydrocephalus Q05.2 Sacral spina bifida with hydrocephalus Q05.3 Unspecified spina bifida with hydrocephalus Q05.4 Cervical spina bifida without hydrocephalus Q05.5 Thoracic spina bifida without -

Neuropathology Category Code List
Neuropathology Page 1 of 27 Neuropathology Major Category Code Headings Revised 10/2018 1 General neuroanatomy, pathology, and staining 65000 2 Developmental neuropathology, NOS 65400 3 Epilepsy 66230 4 Vascular disorders 66300 5 Trauma 66600 6 Infectious/inflammatory disease 66750 7 Demyelinating diseases 67200 8 Complications of systemic disorders 67300 9 Aging and neurodegenerative diseases 68000 10 Prion diseases 68400 11 Neoplasms 68500 12 Skeletal Muscle 69500 13 Peripheral Nerve 69800 14 Ophthalmic pathology 69910 Neuropathology Page 2 of 27 Neuropathology 1 General neuroanatomy, pathology, and staining 65000 A Neuroanatomy, NOS 65010 1 Neocortex 65011 2 White matter 65012 3 Entorhinal cortex/hippocampus 65013 4 Deep (basal) nuclei 65014 5 Brain stem 65015 6 Cerebellum 65016 7 Spinal cord 65017 8 Pituitary 65018 9 Pineal 65019 10 Tracts 65020 11 Vascular supply 65021 12 Notochord 65022 B Cell types 65030 1 Neurons 65031 2 Astrocytes 65032 3 Oligodendroglia 65033 4 Ependyma 65034 5 Microglia and mononuclear cells 65035 6 Choroid plexus 65036 7 Meninges 65037 8 Blood vessels 65038 C Cerebrospinal fluid 65045 D Pathologic responses in neurons and axons 65050 1 Axonal degeneration/spheroid/reaction 65051 2 Central chromatolysis 65052 3 Tract degeneration 65053 4 Swollen/ballooned neurons 65054 5 Trans-synaptic neuronal degeneration 65055 6 Olivary hypertrophy 65056 7 Acute ischemic (hypoxic) cell change 65057 8 Apoptosis 65058 9 Protein aggregation 65059 10 Protein degradation/ubiquitin pathway 65060 E Neuronal nuclear inclusions 65100 -
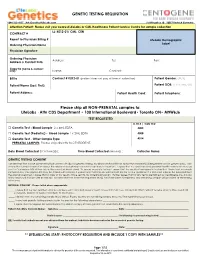
GENETIC TESTING REQUISITION Please Ship All
GENETIC TESTING REQUISITION 1-844-363-4357· [email protected] Schillingallee 68 · 18057 Rostock Germany Attention Patient: Please visit your nearest LifeLabs or CML Healthcare Patient Service Centre for sample collection LL: K012-01/ CML: CEN CONTRACT # Report to Physician Billing # LifeLabs Demographic Ordering Physician Name Label Physician Signature: Ordering Physician Address: Tel: Fax: Address & Contact Info: Copy to (name & contact info): Name: Contact: Bill to Contract # K012-01 (patient does not pay at time of collection) Patient Gender: (M/F) Patient Name (Last, First): Patient DOB: (YYYY/MM/DD) Patient Address: Patient Health Card: Patient Telephone: Please ship all NON-PRENATAL samples to: LifeLabs · Attn CDS Department • 100 International Boulevard• Toronto ON• M9W6J6 TEST REQUESTED LL TR # / CML TC# □ Genetic Test - Blood Sample 2 x 4mL EDTA 4005 □ Genetic Test (Pediatric) - Blood Sample 1 x 2mL EDTA 4008 □ Genetic Test - Other Sample Type 4014 PRENATAL SAMPLES: Please ship directly to CENTOGENE. Date Blood Collected (YYYY/MM/DD): ___________ Time Blood Collected (HH:MM)) :________ Collector Name: ___________________ GENETIC TESTING CONSENT I understand that a DNA specimen will be sent to LifeLabs for genetic testing. My physician has told me about the condition(s) being tested and its genetic basis. I am aware that correct information about the relationships between my family members is important. I agree that my specimen and personal health information may be sent to Centogene AG at their lab in Germany (address below). To ensure accurate testing, I agree that the results of any genetic testing that I have had previously completed by Centogene AG may be shared with LifeLabs. -

Atypical Development of the Cerebellum : Impact on Language Function Lynette M
University of New Mexico UNM Digital Repository Psychology ETDs Electronic Theses and Dissertations 8-28-2012 Atypical development of the cerebellum : impact on language function Lynette M. Silva Follow this and additional works at: https://digitalrepository.unm.edu/psy_etds Recommended Citation Silva, Lynette M.. "Atypical development of the cerebellum : impact on language function." (2012). https://digitalrepository.unm.edu/psy_etds/129 This Dissertation is brought to you for free and open access by the Electronic Theses and Dissertations at UNM Digital Repository. It has been accepted for inclusion in Psychology ETDs by an authorized administrator of UNM Digital Repository. For more information, please contact [email protected]. Lynette M. Silva Candidate Psychology Department This dissertation is approved, and it is acceptable in quality and form for publication: Approved by the Dissertation Committee: Steven Verney, Co-Chairperson Ron Yeo, Co-Chairperson Robert Thoma Jean Lowe ATYPICAL DEVELOPMENT OF THE CEREBELLUM: IMPACT ON LANGUAGE FUNCTION By LYNETTE M. SILVA B.A., English, Stanford University, 1996 M.S., Psychology, University of New Mexico, 2009 DISSERTATION Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Psychology The University of New Mexico Albuquerque, New Mexico July 2012 iii Dedication For my parents, extended family, and valued friends, because it took a village. And for Martin Rodriguez, who served as my Virgil, and showed me the way. iv Acknowledgements I would like to thank Drs. Steven Verney, Ron Yeo, Robert Thoma, and Jean Lowe for their guidance and support as members of my dissertation committee. I am very thankful for the encouragement and supervision I continue to receive from Dr. -

Chapter 1 Cellular Reaction to Injury 3
Schneider_CH01-001-016.qxd 5/1/08 10:52 AM Page 1 chapter Cellular Reaction 1 to Injury I. ADAPTATION TO ENVIRONMENTAL STRESS A. Hypertrophy 1. Hypertrophy is an increase in the size of an organ or tissue due to an increase in the size of cells. 2. Other characteristics include an increase in protein synthesis and an increase in the size or number of intracellular organelles. 3. A cellular adaptation to increased workload results in hypertrophy, as exemplified by the increase in skeletal muscle mass associated with exercise and the enlargement of the left ventricle in hypertensive heart disease. B. Hyperplasia 1. Hyperplasia is an increase in the size of an organ or tissue caused by an increase in the number of cells. 2. It is exemplified by glandular proliferation in the breast during pregnancy. 3. In some cases, hyperplasia occurs together with hypertrophy. During pregnancy, uterine enlargement is caused by both hypertrophy and hyperplasia of the smooth muscle cells in the uterus. C. Aplasia 1. Aplasia is a failure of cell production. 2. During fetal development, aplasia results in agenesis, or absence of an organ due to failure of production. 3. Later in life, it can be caused by permanent loss of precursor cells in proliferative tissues, such as the bone marrow. D. Hypoplasia 1. Hypoplasia is a decrease in cell production that is less extreme than in aplasia. 2. It is seen in the partial lack of growth and maturation of gonadal structures in Turner syndrome and Klinefelter syndrome. E. Atrophy 1. Atrophy is a decrease in the size of an organ or tissue and results from a decrease in the mass of preexisting cells (Figure 1-1). -
CELL INJURY MEDICAL (Lecture 1)
CELL INJURY MEDICAL (lecture 1) Sufia Husain Assistant Prof & Consultant College of Medicine, KSU, Riyadh. September 2015 Objectives for Cell Injury Chapter (3 lectures) The students should: A. Understand the concept of cells and tissue adaptation to environmental stress including the meaning of hypertrophy, hyperplasia, aplasia, atrophy, hypoplasia and metaplasia with their clinical manifestations. B. Is aware of the concept of hypoxic cell injury and its major causes. C. Understand the definitions and mechanisms of free radical injury. D. Knows the definition of apoptosis, tissue necrosis and its various types with clinical examples. E. Able to differentiate between necrosis and apoptosis. F. Understand the causes of and pathologic changes occurring in fatty change (steatosis), accumulations of exogenous and endogenous pigments (carbon, silica, iron, melanin, bilirubin and lipofuscin). G. Understand the causes of and differences between dystrophic and metastatic calcifications. Lecture 1 outline . Adaptation to environmental stress: hypertrophy, hyperplasia, aplasia, hypoplasia, atrophy, squamous metaplasia, osseous metaplasia and myeloid metaplasia. Hypoxic cell injury and its causes (ischaemia, anaemia, carbon monoxide poisoning, decreased perfusion of tissues by oxygen, carrying blood and poor oxygenation of blood). Free radical injury: definition of free radicals, mechanisms that generate free radicals, mechanisms that degrade free radicals. Reversible and irreversible cell injury ADAPTATION TO ENVIRONMENTAL STRESS Adaptation to environmental stress . Cells are constantly adjusting their structure and function to accommodate changing demands i.e. they adapt within physiological limits. As cells encounter physiologic stresses or pathologic stimuli, they can undergo adaptation. The principal adaptive responses are . hypertrophy, . hyperplasia, . atrophy, . metaplasia. (NOTE: If the adaptive capability is exceeded or if the external stress is harmful, cell injury develops. -

Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel
Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel Overview Arthrogryposis or arthrogryposis multiplex congenita (AMC) is a group of nonprogressive conditions characterized by multiple joint contractures found throughout the body at birth. It usually appears as a feature of other neuromuscular conditions or part of systemic diseases. Primary cases may present prenatally with decreased fetal movements associated with joint contractures as well as brain abnormalities, decreased muscle bulk and polyhydramnios whereas secondary causes may present with isolated contractures. Congenital Myasthenic Syndromes (CMS) are a clinically and genetically heterogeneous group of disorders characterized by impaired neuromuscular transmission. Clinically they usually present with abnormal fatigability upon exertion, transient weakness of extra-ocular, facial, bulbar, truncal or limb muscles. Severity ranges from mild, phasic weakness, to disabling permanent weakness with respiratory difficulties and ultimately death. The mode of inheritance of these diseases typically follows and autosomal recessive pattern, although dominant forms can be seen. The Igenomix Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel can be as a tool for an accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved, and their high or intermediate penetrance. -

Complete Androgen Insensitivity Syndrome in a Chinese Neonate
HK J Paediatr (new series) 2004;9:248-252 Complete Androgen Insensitivity Syndrome in a Chinese Neonate MC HO, KL NG Abstract Complete androgen insensitivity syndrome (CAIS) is a rare X-linked disorder with a female external phenotype.1 We report on a Chinese baby with CAIS who presented with bilateral inguinal hernias. The baby has a normal female phenotype at birth. On further evaluation, the karyotype was found to be 46, XY. Endocrine findings were compatible with androgen insensitivity syndrome. Bilateral herniotomy was performed. We would review the literature, offer an overview of the disease, and discuss the outcome with emphasis on the treatment modalities. Key words Complete androgen insensitivity; Male pseudohermaphrodites Introduction investigations which, to the best of our knowledge, has not been reported on the literature.4 Herein we report a case of In 1953, an American gynaecologist JM Morris firstly CAIS in a Chinese neonate in the local region. described a series of individuals with androgen insensitivity syndrome (AIS).2 He reported that these individuals had normal female external genitalia, normal female breast Case Report development, absent or scant axillary and pubic hair, absent internal genital organs and undescended testes. AIS is the The patient was a Chinese baby born at full term by most common condition that results in male under- spontaneous vaginal delivery weighing 2.67 Kg. The masculinisation.3 It is caused by mutations in the androgen antenatal and postnatal course was uneventful. She was the receptor (AR) gene and encompasses a wide spectrum of first child born to the parents. There was no consanguinity male pseudohermaphroditisms.2 In complete androgen nor any significant family history, in particular there was insensitivity syndrome (CAIS), the function of the AR is no abnormal puberty nor infertility on the maternal side. -

Early ACCESS Diagnosed Conditions List
Iowa Early ACCESS Diagnosed Conditions Eligibility List List adapted with permission from Early Intervention Colorado To search for a specific word type "Ctrl F" to use the "Find" function. Is this diagnosis automatically eligible for Early Medical Diagnosis Name Other Names for the Diagnosis and Additional Diagnosis Information ACCESS? 6q terminal deletion syndrome Yes Achondrogenesis I Parenti-Fraccaro Yes Achondrogenesis II Langer-Saldino Yes Schinzel Acrocallosal syndrome; ACLS; ACS; Hallux duplication, postaxial polydactyly, and absence of the corpus Acrocallosal syndrome, Schinzel Type callosum Yes Acrodysplasia; Arkless-Graham syndrome; Maroteaux-Malamut syndrome; Nasal hypoplasia-peripheral dysostosis-intellectual disability syndrome; Peripheral dysostosis-nasal hypoplasia-intellectual disability (PNM) Acrodysostosis syndrome Yes ALD; AMN; X-ALD; Addison disease and cerebral sclerosis; Adrenomyeloneuropathy; Siemerling-creutzfeldt disease; Bronze schilder disease; Schilder disease; Melanodermic Leukodystrophy; sudanophilic leukodystrophy; Adrenoleukodystrophy Pelizaeus-Merzbacher disease Yes Agenesis of Corpus Callosum Absence of the corpus callosum; Hypogenesis of the corpus callosum; Dysplastic corpus callosum Yes Agenesis of Corpus Callosum and Chorioretinal Abnormality; Agenesis of Corpus Callosum With Chorioretinitis Abnormality; Agenesis of Corpus Callosum With Infantile Spasms And Ocular Anomalies; Chorioretinal Anomalies Aicardi syndrome with Agenesis Yes Alexander Disease Yes Allan Herndon syndrome Allan-Herndon-Dudley -

Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017
Appendix 3.1 Birth Defects Descriptions for NBDPN Core, Recommended, and Extended Conditions Updated March 2017 Participating members of the Birth Defects Definitions Group: Lorenzo Botto (UT) John Carey (UT) Cynthia Cassell (CDC) Tiffany Colarusso (CDC) Janet Cragan (CDC) Marcia Feldkamp (UT) Jamie Frias (CDC) Angela Lin (MA) Cara Mai (CDC) Richard Olney (CDC) Carol Stanton (CO) Csaba Siffel (GA) Table of Contents LIST OF BIRTH DEFECTS ................................................................................................................................................. I DETAILED DESCRIPTIONS OF BIRTH DEFECTS ...................................................................................................... 1 FORMAT FOR BIRTH DEFECT DESCRIPTIONS ................................................................................................................................. 1 CENTRAL NERVOUS SYSTEM ....................................................................................................................................... 2 ANENCEPHALY ........................................................................................................................................................................ 2 ENCEPHALOCELE ..................................................................................................................................................................... 3 HOLOPROSENCEPHALY.............................................................................................................................................................