Neuropathology Category Code List
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inherited Cerebellar Ataxia in Childhood: a Pattern-Recognition Approach Using Brain MRI
REVIEW ARTICLE Inherited Cerebellar Ataxia in Childhood: A Pattern-Recognition Approach Using Brain MRI L. Vedolin, G. Gonzalez, C.F. Souza, C. Lourenc¸o, and A.J. Barkovich ABSTRACT SUMMARY: Ataxia is the principal symptom of many common neurologic diseases in childhood. Ataxias caused by dysfunction of the cerebellum occur in acute, intermittent, and progressive disorders. Most of the chronic progressive processes are secondary to degen- erative and metabolic diseases. In addition, congenital malformation of the midbrain and hindbrain can also be present, with posterior fossa symptoms related to ataxia. Brain MR imaging is the most accurate imaging technique to investigate these patients, and imaging abnormalities include size, shape, and/or signal of the brain stem and/or cerebellum. Supratentorial and cord lesions are also common. This review will discuss a pattern-recognition approach to inherited cerebellar ataxia in childhood. The purpose is to provide a comprehensive discussion that ultimately could help neuroradiologists better manage this important topic in pediatric neurology. ABBREVIATIONS: AR ϭ autosomal recessive; CAC ϭ cerebellar ataxia in childhood; 4H ϭ hypomyelination with hypogonadotropic hypogonadism and hypodon- tia; JSRD ϭ Joubert syndrome and related disorders; OPHN1 ϭ oligophrenin-1 taxia is an inability to coordinate voluntary muscle move- plastic/paraneoplastic disorders, immune-mediated/demyelinat- Aments that cannot be attributed to weakness or involuntary ing disorders, and drugs/toxins (antiepileptic medications, -

November 2016 NEMSN Newsletter
Vol. Vol. 26 No.No. 1 1 The National Eosinophilia-Myalgia Syndrome Network, Inc. November Page 2016 1 Friends Supporting Friends National EMS Network NEMSN National Eosinophilia-Myalgia Syndrome Network, Inc. http:www.nemsn.org Newsletter Points of interest ………………..……………... NEMSN is extremely pleased to announce that Stephen Naylor, • Your continued do- Ph.D. has joined our Medical Advisory Panel as NEMSN's nations have kept Science Advisor. Welcome, Dr. Naylor. this Newsletter and NEMSN alive. Dr. Stephen Naylor is one of only a handful of distin- Please keep those guished scientists who have devoted years of research in donations coming an attempt to achieve a complete explanation of EMS. no matter how Known as a chemist, biochemist, toxicologist and business large or small. Our originator, he has co-authored hundreds of scientific re- thanks. search papers and book chapters while delivering un- ………………………………….. counted presentations at universities and medical centers • We are interested worldwide. In the 1990s he and NEMSN advisor Gerald J. in your story. Please Gleich, M.D. partnered at the Mayo Clinic in Rochester, take the time to MN to undertake definitive EMS and L-tryptophan re- write it and send to search. Naylor and Gleich received NIH and WHO grants us for our newslet- and co-authored a number of scholarly papers during that period. ter. …………………………………... Stephen Naylor received his Ph.D. from the University of Cambridge (UK) in Biochem- • If you have not seen istry. He completed postdoctoral work at the Massachusetts Institute of Technology our web site yet, it where he later became a visiting faculty member in the Division of Biological Engineer- is very informative. -

Strategies to Improve Nerve Regeneration After Radical Prostatectomy: a Narrative Review
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Institutional Research Information System University of Turin Strategies to improve nerve regeneration after radical prostatectomy: a narrative review Stefano Geuna 1, 2, Luisa Muratori1, 2, Federica Fregnan 1, 2, Matteo Manfredi4 , Riccardo Bertolo 3, 4 , Francesco Porpiglia4. 1 Department of Clinical and Biological Sciences, University of Turin, Orbassano (To), 10043, Italy. 2 Neuroscience Institute Cavalieri Ottolenghi (NICO), Orbassano (To), 10043, Italy. 3 Urological and Kidney Institute, Cleveland Clinic, Cleveland, OH, US. 4 Department of Oncology, University of Turin, Orbassano (To), 10043, Italy. Abstract Peripheral nerves are complex organs that spread throughout the entire human body. They are frequently affected by lesions not only as a result of trauma but also following radical tumor resection. In fact, despite the advancement in surgical techniques, such as nerve- sparing robot assisted radical prostatectomy, some degree of nerve injury may occur resulting in erectile dysfunction with significant impairment of the quality of life. The aim of this review is to provide an overview on the mechanisms of the regeneration of injured peripheral nerves and to describe the potential strategies to improve the regeneration process and the functional recovery. Yet, the recent advances in bio- engineering strategies to promote nerve regeneration in the urological field are outlined with a view on the possible future regenerative therapies which might ameliorate the functional outcome after radical prostatectomy. 1 Introduction Radical prostatectomy is the gold standard surgical treatment for organ-confined prostate cancer. The employment of innovative surgical technique such as nerve-sparing robot assisted radical prostatectomy allowed to magnify the anatomical field leading to a three- dimensional perspective obtained through the robotic lenses and a better anatomical knowledge. -

To View the ESE Recommended Curriculum of Specialisation in Clinical Endocrinology, Diabetes and Metabolism
European Society of Endocrinology Recommended Curriculum of Specialisation in Clinical Endocrinology, Diabetes and Metabolism Version 2, November 2019 Contents Endorsement ........................................................................................................................................ 2 Introduction .......................................................................................................................................... 3 1. Diabetes mellitus .............................................................................................................................. 4 2. Lipid disorders ................................................................................................................................... 5 3. Obesity and bariatric endocrinology ................................................................................................. 5 4. Pituitary ............................................................................................................................................ 5 5. Thyroid .............................................................................................................................................. 6 6. Parathyroid, calcium and bone ......................................................................................................... 7 7. Adrenal ............................................................................................................................................. 8 8. Reproductive endocrinology and sexual function -

RD-Action Matchmaker – Summary of Disease Expertise Recorded Under
Summary of disease expertise recorded via RD-ACTION Matchmaker under each Thematic Grouping and EURORDIS Members’ Thematic Grouping Thematic Reported expertise of those completing the EURORDIS Member perspectives on Grouping matchmaker under each heading Grouping RD Thematically Rare Bone Achondroplasia/Hypochondroplasia Achondroplasia Amelia skeletal dysplasia’s including Achondroplasia/Growth hormone cleidocranial dysostosis, arthrogryposis deficiency/MPS/Turner Brachydactyly chondrodysplasia punctate Fibrous dysplasia of bone Collagenopathy and oncologic disease such as Fibrodysplasia ossificans progressive Li-Fraumeni syndrome Osteogenesis imperfecta Congenital hand and fore-foot conditions Sterno Costo Clavicular Hyperostosis Disorders of Sex Development Duchenne Muscular Dystrophy Ehlers –Danlos syndrome Fibrodysplasia Ossificans Progressiva Growth disorders Hypoparathyroidism Hypophosphatemic rickets & Nutritional Rickets Hypophosphatasia Jeune’s syndrome Limb reduction defects Madelung disease Metabolic Osteoporosis Multiple Hereditary Exostoses Osteogenesis imperfecta Osteoporosis Paediatric Osteoporosis Paget’s disease Phocomelia Pseudohypoparathyroidism Radial dysplasia Skeletal dysplasia Thanatophoric dwarfism Ulna dysplasia Rare Cancer and Adrenocortical tumours Acute monoblastic leukaemia Tumours Carcinoid tumours Brain tumour Craniopharyngioma Colon cancer, familial nonpolyposis Embryonal tumours of CNS Craniopharyngioma Ependymoma Desmoid disease Epithelial thymic tumours in -

Multiple Orbital Neurofibromas, Painful Peripheral Nerve Tumors, Distinctive
European Journal of Human Genetics (2012) 20, 618–625 & 2012 Macmillan Publishers Limited All rights reserved 1018-4813/12 www.nature.com/ejhg ARTICLE Multiple orbital neurofibromas, painful peripheral nerve tumors, distinctive face and marfanoid habitus: a new syndrome D Babovic-Vuksanovic*,1, Ludwine Messiaen2, Christoph Nagel3, Hilde Brems4, Bernd Scheithauer5, Ellen Denayer4, Rong Mao6, Raf Sciot7, Karen M Janowski2, Martin U Schuhmann3, Kathleen Claes8, Eline Beert4, James A Garrity9, Robert J Spinner10, Anat Stemmer-Rachamimov11, Ralitza Gavrilova1, Frank Van Calenbergh12, Victor Mautner13 and Eric Legius4 Four unrelated patients having an unusual clinical phenotype, including multiple peripheral nerve sheath tumors, are reported. Their clinical features were not typical of any known familial tumor syndrome. The patients had multiple painful neurofibromas, including bilateral orbital plexiform neurofibromas, and spinal as well as mucosal neurofibromas. In addition, they exhibited a marfanoid habitus, shared similar facial features, and had enlarged corneal nerves as well as neuronal migration defects. Comprehensive NF1, NF2 and SMARCB1 mutation analyses revealed no mutation in blood lymphocytes and in schwann cells cultured from plexiform neurofibromas. Furthermore, no mutations in RET, PRKAR1A, PTEN and other RAS-pathway genes were found in blood leukocytes. Collectively, the clinical and pathological findings in these four cases fit no known syndrome and likely represent a new disorder. European Journal of Human Genetics (2012) 20, 618–625; doi:10.1038/ejhg.2011.275; published online 18 January 2012 Keywords: orbital neurofibroma; plexiform neurofibroma; enlarged corneal nerves; marfanoid habitus INTRODUCTION Ruvalcaba syndrome, a part of the PHTS spectrum, develop cafe´- Peripheral nerve sheath tumors, specifically neurofibromas and au-lait spots and macules of the glans penis. -

Clinicians Using the Classification Will Identify a Seizure As Focal Or Generalized Onset If There Is About an 80% Confidence Level About the Type of Onset
GENERALIZED ONSET SEIZURES Generalized onset seizures are not characterized by level of awareness, because awareness is almost always impaired. Generalized tonic-clonic: Immediate loss of Generalized epileptic spasms: Brief seizures with awareness, with stiffening of all limbs (tonic phase), flexion at the trunk and flexion or extension of the followed by sustained rhythmic jerking of limbs and limbs. Video-EEG recording may be required to face (clonic phase). Duration is typically 1 to 3 minutes. determine focal versus generalized onset. The seizure may produce a cry at the start, falling, tongue biting, and incontinence. Generalized typical absence: Sudden onset when activity stops with a brief pause and staring, Generalized clonic: Rhythmical sustained jerking of sometimes with eye fluttering and head nodding or limbs and/or head with no tonic stiffening phase. other automatic behaviors. If it lasts for more than These seizures most often occur in young children. several seconds, awareness and memory are impaired. Recovery is immediate. The EEG during these seizures Generalized tonic: Stiffening of all limbs, without always shows generalized spike-waves. clonic jerking. Generalized atypical absence: Like typical absence Generalized myoclonic: Irregular, unsustained jerking seizures, but may have slower onset and recovery and of limbs, face, eyes, or eyelids. The jerking of more pronounced changes in tone. Atypical absence generalized myoclonus may not always be left-right seizures can be difficult to distinguish from focal synchronous, but it occurs on both sides. impaired awareness seizures, but absence seizures usually recover more quickly and the EEG patterns are Generalized myoclonic-tonic-clonic: This seizure is like different. -

Imaging Surgical Epilepsy in Children
Childs Nerv Syst (2006) 22:786–809 DOI 10.1007/s00381-006-0132-5 SPECIAL ANNUAL ISSUE Imaging surgical epilepsy in children Charles Raybaud & Manohar Shroff & James T. Rutka & Sylvester H. Chuang Received: 1 February 2006 / Published online: 13 June 2006 # Springer-Verlag 2006 Abstract of the diverse pathologies concerned with epilepsy surgery in Introduction Epilepsy surgery rests heavily upon magnetic the pediatric context is provided with illustrative images. resonance imaging (MRI). Technical developments have brought significantly improved efficacy of MR imaging in Keywords MR imaging . Epilepsy. Ganglioglioma . DNT. detecting and assessing surgical epileptogenic lesions, PXA . FCD . Hypothalamic hamartoma . while more clinical experience has brought better definition Meningioangiomatosis of the pathological groups. Discussion MRI is fairly efficient in identifying develop- mental, epilepsy-associated tumors such as ganglioglioma Introduction (with its variants gangliocytoma and desmoplastic infantile ganglioglioma), the complex, simple and nonspecific forms Epilepsy surgery in children addresses severe refractory of dysembryoplastic neuroepithelial tumor, and the rare epilepsy mainly, which threatens the child’s development, pleomorphic xanthoastrocytoma. The efficacy of MR when a constant epileptogenic focus can be identified from imaging is not as good for the diagnosis of focal cortical the clinical and the electroencephalogram (EEG) data and be dysplasia (FCD), as it does not necessarily correlate with removed. Imaging must demonstrate -

Myoclonic Status Epilepticus in Juvenile Myoclonic Epilepsy
Original article Epileptic Disord 2009; 11 (4): 309-14 Myoclonic status epilepticus in juvenile myoclonic epilepsy Julia Larch, Iris Unterberger, Gerhard Bauer, Johannes Reichsoellner, Giorgi Kuchukhidze, Eugen Trinka Department of Neurology, Medical University of Innsbruck, Austria Received April 9, 2009; Accepted November 18, 2009 ABSTRACT – Background. Myoclonic status epilepticus (MSE) is rarely found in juvenile myoclonic epilepsy (JME) and its clinical features are not well described. We aimed to analyze MSE incidence, precipitating factors and clini- cal course by studying patients with JME from a large outpatient epilepsy clinic. Methods. We retrospectively screened all patients with JME treated at the Department of Neurology, Medical University of Innsbruck, Austria between 1970 and 2007 for a history of MSE. We analyzed age, sex, age at seizure onset, seizure types, EEG, MRI/CT findings and response to antiepileptic drugs. Results. Seven patients (five women, two men; median age at time of MSE 31 years; range 17-73) with MSE out of a total of 247 patients with JME were identi- fied. The median follow-up time was seven years (range 0-35), the incidence was 3.2/1,000 patient years. Median duration of epilepsy before MSE was 26 years (range 10-58). We identified three subtypes: 1) MSE with myoclonic seizures only in two patients, 2) MSE with generalized tonic clonic seizures in three, and 3) generalized tonic clonic seizures with myoclonic absence status in two patients. All patients responded promptly to benzodiazepines. One patient had repeated episodes of MSE. Precipitating events were identified in all but one patient. Drug withdrawal was identified in four patients, one of whom had additional sleep deprivation and alcohol intake. -
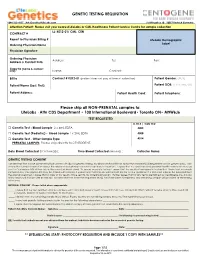
GENETIC TESTING REQUISITION Please Ship All
GENETIC TESTING REQUISITION 1-844-363-4357· [email protected] Schillingallee 68 · 18057 Rostock Germany Attention Patient: Please visit your nearest LifeLabs or CML Healthcare Patient Service Centre for sample collection LL: K012-01/ CML: CEN CONTRACT # Report to Physician Billing # LifeLabs Demographic Ordering Physician Name Label Physician Signature: Ordering Physician Address: Tel: Fax: Address & Contact Info: Copy to (name & contact info): Name: Contact: Bill to Contract # K012-01 (patient does not pay at time of collection) Patient Gender: (M/F) Patient Name (Last, First): Patient DOB: (YYYY/MM/DD) Patient Address: Patient Health Card: Patient Telephone: Please ship all NON-PRENATAL samples to: LifeLabs · Attn CDS Department • 100 International Boulevard• Toronto ON• M9W6J6 TEST REQUESTED LL TR # / CML TC# □ Genetic Test - Blood Sample 2 x 4mL EDTA 4005 □ Genetic Test (Pediatric) - Blood Sample 1 x 2mL EDTA 4008 □ Genetic Test - Other Sample Type 4014 PRENATAL SAMPLES: Please ship directly to CENTOGENE. Date Blood Collected (YYYY/MM/DD): ___________ Time Blood Collected (HH:MM)) :________ Collector Name: ___________________ GENETIC TESTING CONSENT I understand that a DNA specimen will be sent to LifeLabs for genetic testing. My physician has told me about the condition(s) being tested and its genetic basis. I am aware that correct information about the relationships between my family members is important. I agree that my specimen and personal health information may be sent to Centogene AG at their lab in Germany (address below). To ensure accurate testing, I agree that the results of any genetic testing that I have had previously completed by Centogene AG may be shared with LifeLabs. -

Identification of HRAS Mutations and Absence of GNAQ Or GNA11
Modern Pathology (2013) 26, 1320–1328 1320 & 2013 USCAP, Inc All rights reserved 0893-3952/13 $32.00 Identification of HRAS mutations and absence of GNAQ or GNA11 mutations in deep penetrating nevi Ryan P Bender1, Matthew J McGinniss2, Paula Esmay1, Elsa F Velazquez3,4 and Julie DR Reimann3,4 1Caris Life Sciences, Phoenix, AZ, USA; 2Genoptix Medical Laboratory, Carlsbad, CA, USA; 3Dermatopathology Division, Miraca Life Sciences Research Institute, Newton, MA, USA and 4Department of Dermatology, Tufts Medical Center, Boston, MA, USA HRAS is mutated in B15% of Spitz nevi, and GNAQ or GNA11 is mutated in blue nevi (46–83% and B7% respectively). Epithelioid blue nevi and deep penetrating nevi show features of both blue nevi (intradermal location, pigmentation) and Spitz nevi (epithelioid morphology). Epithelioid blue nevi and deep penetrating nevi can also show overlapping features with melanoma, posing a diagnostic challenge. Although epithelioid blue nevi are considered blue nevic variants, no GNAQ or GNA11 mutations have been reported. Classification of deep penetrating nevi as blue nevic variants has also been proposed, however, no GNAQ or GNA11 mutations have been reported and none have been tested for HRAS mutations. To better characterize these tumors, we performed mutational analysis for GNAQ, GNA11, and HRAS, with blue nevi and Spitz nevi as controls. Within deep penetrating nevi, none demonstrated GNAQ or GNA11 mutations (0/38). However, 6% revealed HRAS mutation (2/32). Twenty percent of epithelioid blue nevi contained a GNAQ mutation (2/10), while none displayed GNA11 or HRAS mutation. Eighty-seven percent of blue nevi contained a GNAQ mutation (26/30), 4% a GNA11 mutation (1/28), and none an HRAS mutation. -

Atypical Development of the Cerebellum : Impact on Language Function Lynette M
University of New Mexico UNM Digital Repository Psychology ETDs Electronic Theses and Dissertations 8-28-2012 Atypical development of the cerebellum : impact on language function Lynette M. Silva Follow this and additional works at: https://digitalrepository.unm.edu/psy_etds Recommended Citation Silva, Lynette M.. "Atypical development of the cerebellum : impact on language function." (2012). https://digitalrepository.unm.edu/psy_etds/129 This Dissertation is brought to you for free and open access by the Electronic Theses and Dissertations at UNM Digital Repository. It has been accepted for inclusion in Psychology ETDs by an authorized administrator of UNM Digital Repository. For more information, please contact [email protected]. Lynette M. Silva Candidate Psychology Department This dissertation is approved, and it is acceptable in quality and form for publication: Approved by the Dissertation Committee: Steven Verney, Co-Chairperson Ron Yeo, Co-Chairperson Robert Thoma Jean Lowe ATYPICAL DEVELOPMENT OF THE CEREBELLUM: IMPACT ON LANGUAGE FUNCTION By LYNETTE M. SILVA B.A., English, Stanford University, 1996 M.S., Psychology, University of New Mexico, 2009 DISSERTATION Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Psychology The University of New Mexico Albuquerque, New Mexico July 2012 iii Dedication For my parents, extended family, and valued friends, because it took a village. And for Martin Rodriguez, who served as my Virgil, and showed me the way. iv Acknowledgements I would like to thank Drs. Steven Verney, Ron Yeo, Robert Thoma, and Jean Lowe for their guidance and support as members of my dissertation committee. I am very thankful for the encouragement and supervision I continue to receive from Dr.