Inherited Cerebellar Ataxia in Childhood: a REVIEW ARTICLE Pattern-Recognition Approach Using Brain MRI
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Inherited Cerebellar Ataxia in Childhood: a Pattern-Recognition Approach Using Brain MRI
REVIEW ARTICLE Inherited Cerebellar Ataxia in Childhood: A Pattern-Recognition Approach Using Brain MRI L. Vedolin, G. Gonzalez, C.F. Souza, C. Lourenc¸o, and A.J. Barkovich ABSTRACT SUMMARY: Ataxia is the principal symptom of many common neurologic diseases in childhood. Ataxias caused by dysfunction of the cerebellum occur in acute, intermittent, and progressive disorders. Most of the chronic progressive processes are secondary to degen- erative and metabolic diseases. In addition, congenital malformation of the midbrain and hindbrain can also be present, with posterior fossa symptoms related to ataxia. Brain MR imaging is the most accurate imaging technique to investigate these patients, and imaging abnormalities include size, shape, and/or signal of the brain stem and/or cerebellum. Supratentorial and cord lesions are also common. This review will discuss a pattern-recognition approach to inherited cerebellar ataxia in childhood. The purpose is to provide a comprehensive discussion that ultimately could help neuroradiologists better manage this important topic in pediatric neurology. ABBREVIATIONS: AR ϭ autosomal recessive; CAC ϭ cerebellar ataxia in childhood; 4H ϭ hypomyelination with hypogonadotropic hypogonadism and hypodon- tia; JSRD ϭ Joubert syndrome and related disorders; OPHN1 ϭ oligophrenin-1 taxia is an inability to coordinate voluntary muscle move- plastic/paraneoplastic disorders, immune-mediated/demyelinat- Aments that cannot be attributed to weakness or involuntary ing disorders, and drugs/toxins (antiepileptic medications, -

Neuropathology Category Code List
Neuropathology Page 1 of 27 Neuropathology Major Category Code Headings Revised 10/2018 1 General neuroanatomy, pathology, and staining 65000 2 Developmental neuropathology, NOS 65400 3 Epilepsy 66230 4 Vascular disorders 66300 5 Trauma 66600 6 Infectious/inflammatory disease 66750 7 Demyelinating diseases 67200 8 Complications of systemic disorders 67300 9 Aging and neurodegenerative diseases 68000 10 Prion diseases 68400 11 Neoplasms 68500 12 Skeletal Muscle 69500 13 Peripheral Nerve 69800 14 Ophthalmic pathology 69910 Neuropathology Page 2 of 27 Neuropathology 1 General neuroanatomy, pathology, and staining 65000 A Neuroanatomy, NOS 65010 1 Neocortex 65011 2 White matter 65012 3 Entorhinal cortex/hippocampus 65013 4 Deep (basal) nuclei 65014 5 Brain stem 65015 6 Cerebellum 65016 7 Spinal cord 65017 8 Pituitary 65018 9 Pineal 65019 10 Tracts 65020 11 Vascular supply 65021 12 Notochord 65022 B Cell types 65030 1 Neurons 65031 2 Astrocytes 65032 3 Oligodendroglia 65033 4 Ependyma 65034 5 Microglia and mononuclear cells 65035 6 Choroid plexus 65036 7 Meninges 65037 8 Blood vessels 65038 C Cerebrospinal fluid 65045 D Pathologic responses in neurons and axons 65050 1 Axonal degeneration/spheroid/reaction 65051 2 Central chromatolysis 65052 3 Tract degeneration 65053 4 Swollen/ballooned neurons 65054 5 Trans-synaptic neuronal degeneration 65055 6 Olivary hypertrophy 65056 7 Acute ischemic (hypoxic) cell change 65057 8 Apoptosis 65058 9 Protein aggregation 65059 10 Protein degradation/ubiquitin pathway 65060 E Neuronal nuclear inclusions 65100 -
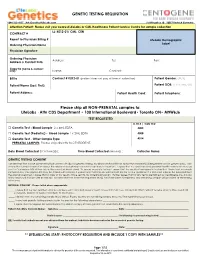
GENETIC TESTING REQUISITION Please Ship All
GENETIC TESTING REQUISITION 1-844-363-4357· [email protected] Schillingallee 68 · 18057 Rostock Germany Attention Patient: Please visit your nearest LifeLabs or CML Healthcare Patient Service Centre for sample collection LL: K012-01/ CML: CEN CONTRACT # Report to Physician Billing # LifeLabs Demographic Ordering Physician Name Label Physician Signature: Ordering Physician Address: Tel: Fax: Address & Contact Info: Copy to (name & contact info): Name: Contact: Bill to Contract # K012-01 (patient does not pay at time of collection) Patient Gender: (M/F) Patient Name (Last, First): Patient DOB: (YYYY/MM/DD) Patient Address: Patient Health Card: Patient Telephone: Please ship all NON-PRENATAL samples to: LifeLabs · Attn CDS Department • 100 International Boulevard• Toronto ON• M9W6J6 TEST REQUESTED LL TR # / CML TC# □ Genetic Test - Blood Sample 2 x 4mL EDTA 4005 □ Genetic Test (Pediatric) - Blood Sample 1 x 2mL EDTA 4008 □ Genetic Test - Other Sample Type 4014 PRENATAL SAMPLES: Please ship directly to CENTOGENE. Date Blood Collected (YYYY/MM/DD): ___________ Time Blood Collected (HH:MM)) :________ Collector Name: ___________________ GENETIC TESTING CONSENT I understand that a DNA specimen will be sent to LifeLabs for genetic testing. My physician has told me about the condition(s) being tested and its genetic basis. I am aware that correct information about the relationships between my family members is important. I agree that my specimen and personal health information may be sent to Centogene AG at their lab in Germany (address below). To ensure accurate testing, I agree that the results of any genetic testing that I have had previously completed by Centogene AG may be shared with LifeLabs. -

Atypical Development of the Cerebellum : Impact on Language Function Lynette M
University of New Mexico UNM Digital Repository Psychology ETDs Electronic Theses and Dissertations 8-28-2012 Atypical development of the cerebellum : impact on language function Lynette M. Silva Follow this and additional works at: https://digitalrepository.unm.edu/psy_etds Recommended Citation Silva, Lynette M.. "Atypical development of the cerebellum : impact on language function." (2012). https://digitalrepository.unm.edu/psy_etds/129 This Dissertation is brought to you for free and open access by the Electronic Theses and Dissertations at UNM Digital Repository. It has been accepted for inclusion in Psychology ETDs by an authorized administrator of UNM Digital Repository. For more information, please contact [email protected]. Lynette M. Silva Candidate Psychology Department This dissertation is approved, and it is acceptable in quality and form for publication: Approved by the Dissertation Committee: Steven Verney, Co-Chairperson Ron Yeo, Co-Chairperson Robert Thoma Jean Lowe ATYPICAL DEVELOPMENT OF THE CEREBELLUM: IMPACT ON LANGUAGE FUNCTION By LYNETTE M. SILVA B.A., English, Stanford University, 1996 M.S., Psychology, University of New Mexico, 2009 DISSERTATION Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy Psychology The University of New Mexico Albuquerque, New Mexico July 2012 iii Dedication For my parents, extended family, and valued friends, because it took a village. And for Martin Rodriguez, who served as my Virgil, and showed me the way. iv Acknowledgements I would like to thank Drs. Steven Verney, Ron Yeo, Robert Thoma, and Jean Lowe for their guidance and support as members of my dissertation committee. I am very thankful for the encouragement and supervision I continue to receive from Dr. -

Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel
Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel Overview Arthrogryposis or arthrogryposis multiplex congenita (AMC) is a group of nonprogressive conditions characterized by multiple joint contractures found throughout the body at birth. It usually appears as a feature of other neuromuscular conditions or part of systemic diseases. Primary cases may present prenatally with decreased fetal movements associated with joint contractures as well as brain abnormalities, decreased muscle bulk and polyhydramnios whereas secondary causes may present with isolated contractures. Congenital Myasthenic Syndromes (CMS) are a clinically and genetically heterogeneous group of disorders characterized by impaired neuromuscular transmission. Clinically they usually present with abnormal fatigability upon exertion, transient weakness of extra-ocular, facial, bulbar, truncal or limb muscles. Severity ranges from mild, phasic weakness, to disabling permanent weakness with respiratory difficulties and ultimately death. The mode of inheritance of these diseases typically follows and autosomal recessive pattern, although dominant forms can be seen. The Igenomix Arthrogryposis and Congenital Myasthenic Syndrome Precision Panel can be as a tool for an accurate diagnosis ultimately leading to a better management and prognosis of the disease. It provides a comprehensive analysis of the genes involved in this disease using next-generation sequencing (NGS) to fully understand the spectrum of relevant genes involved, and their high or intermediate penetrance. -

Early ACCESS Diagnosed Conditions List
Iowa Early ACCESS Diagnosed Conditions Eligibility List List adapted with permission from Early Intervention Colorado To search for a specific word type "Ctrl F" to use the "Find" function. Is this diagnosis automatically eligible for Early Medical Diagnosis Name Other Names for the Diagnosis and Additional Diagnosis Information ACCESS? 6q terminal deletion syndrome Yes Achondrogenesis I Parenti-Fraccaro Yes Achondrogenesis II Langer-Saldino Yes Schinzel Acrocallosal syndrome; ACLS; ACS; Hallux duplication, postaxial polydactyly, and absence of the corpus Acrocallosal syndrome, Schinzel Type callosum Yes Acrodysplasia; Arkless-Graham syndrome; Maroteaux-Malamut syndrome; Nasal hypoplasia-peripheral dysostosis-intellectual disability syndrome; Peripheral dysostosis-nasal hypoplasia-intellectual disability (PNM) Acrodysostosis syndrome Yes ALD; AMN; X-ALD; Addison disease and cerebral sclerosis; Adrenomyeloneuropathy; Siemerling-creutzfeldt disease; Bronze schilder disease; Schilder disease; Melanodermic Leukodystrophy; sudanophilic leukodystrophy; Adrenoleukodystrophy Pelizaeus-Merzbacher disease Yes Agenesis of Corpus Callosum Absence of the corpus callosum; Hypogenesis of the corpus callosum; Dysplastic corpus callosum Yes Agenesis of Corpus Callosum and Chorioretinal Abnormality; Agenesis of Corpus Callosum With Chorioretinitis Abnormality; Agenesis of Corpus Callosum With Infantile Spasms And Ocular Anomalies; Chorioretinal Anomalies Aicardi syndrome with Agenesis Yes Alexander Disease Yes Allan Herndon syndrome Allan-Herndon-Dudley -

VLDLR-Associated Cerebellar Hypoplasia
VLDLR-associated cerebellar hypoplasia Description VLDLR-associated cerebellar hypoplasia is an inherited condition that affects the development of the brain. People with this condition have an unusually small and underdeveloped cerebellum, which is the part of the brain that coordinates movement. This brain malformation leads to problems with balance and coordination (ataxia) that become apparent in infancy and remain stable over time. Children with VLDLR- associated cerebellar hypoplasia may learn to walk later in childhood, usually after the age of 6, although some are never able to walk independently. In one Turkish family, affected people walk on their hands and feet (quadrupedal locomotion). Additional features of VLDLR-associated cerebellar hypoplasia include moderate to profound intellectual disability, impaired speech (dysarthria) or a lack of speech, and eyes that do not look in the same direction (strabismus). Some affected individuals have also had flat feet (pes planus), seizures, and short stature. Studies suggest that VLDLR- associated cerebellar hypoplasia does not significantly affect a person's life expectancy. Frequency VLDLR-associated cerebellar hypoplasia is rare; its prevalence is unknown. The condition was first described in the Hutterite population in Canada and the United States. This condition has also been reported in families from Iran and Turkey. Causes As its name suggests, VLDLR-associated cerebellar hypoplasia results from mutations in the VLDLR gene. This gene provides instructions for making a protein called a very low density lipoprotein (VLDL) receptor. Starting before birth, this protein plays a critical role in guiding the movement of developing nerve cells to their appropriate locations in the brain. Mutations in the VLDLR gene prevent cells from producing any functional VLDL receptor protein. -

Cerebellar Hypoplasia Associated with Systemic Degeneration in Early Life by R
J Neurol Neurosurg Psychiatry: first published as 10.1136/jnnp.21.3.159 on 1 August 1958. Downloaded from J. Neurol. Neurosurg. Psychiat., 1958, 21, 159. CEREBELLAR HYPOPLASIA ASSOCIATED WITH SYSTEMIC DEGENERATION IN EARLY LIFE BY R. M. NORMAN and H. URICH From the Burden Neuropathological Laboratory, Frenchay Hospital, Bristol Hypoplasia predominantly affecting the lateral weeks later and the head circumference was then 144 in. lobes of the cerebellum has on several occasions The retinal veins were not engorged and there seemed to been found associated with marked underdevelop- be no indication for immediate operation. On admission ment of the griseum pontis and middle peduncle to hospital 10 weeks later, it was confirmed that the fontanelles were closed, although the shape of the head (Vogt and Astwazaturow, 1912; Brun, 1917, 1918; did not conform to any of the recognized types of Brouwer, 1924; Biemond, 1955). Brouwer named craniosynostosis. The child lay with the head retracted this condition " hypoplasia ponto-neocerebellaris " and the limbs spastic and flexed. Tonsillar herniation and emphasized the fact that the same neuronal was suspected and it was considered to be too dangerous system was affected in this prenatal malformation to carry out air studies. Parasagittal linear craniectomies as in olivo-ponto-cerebellar atrophy. Support was were performed but the cerebral gyri were not flattened Protected by copyright. thus given to the theory already put forward by and the tension not high. Two hours after having Winkler (1923) that a congenital weakness of the apparently recovered from the operation the infant derivatives of the cell bands of Essick (1912) under- developed signs of respiratory failure and an emergency the degenerations of olivo-ponto- suboccipital decompression was carried out. -

A Dictionary of Neurological Signs.Pdf
A DICTIONARY OF NEUROLOGICAL SIGNS THIRD EDITION A DICTIONARY OF NEUROLOGICAL SIGNS THIRD EDITION A.J. LARNER MA, MD, MRCP (UK), DHMSA Consultant Neurologist Walton Centre for Neurology and Neurosurgery, Liverpool Honorary Lecturer in Neuroscience, University of Liverpool Society of Apothecaries’ Honorary Lecturer in the History of Medicine, University of Liverpool Liverpool, U.K. 123 Andrew J. Larner MA MD MRCP (UK) DHMSA Walton Centre for Neurology & Neurosurgery Lower Lane L9 7LJ Liverpool, UK ISBN 978-1-4419-7094-7 e-ISBN 978-1-4419-7095-4 DOI 10.1007/978-1-4419-7095-4 Springer New York Dordrecht Heidelberg London Library of Congress Control Number: 2010937226 © Springer Science+Business Media, LLC 2001, 2006, 2011 All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, LLC, 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dissimilar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identified as such, is not to be taken as an expression of opinion as to whether or not they are subject to proprietary rights. While the advice and information in this book are believed to be true and accurate at the date of going to press, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omissions that may be made. -

A Clinical-Based Diagnostic Approach to Cerebellar Atrophy in Children
applied sciences Article A Clinical-Based Diagnostic Approach to Cerebellar Atrophy in Children Claudia Ciaccio 1,* , Chiara Pantaleoni 1, Franco Taroni 2 , Daniela Di Bella 2, Stefania Magri 2 , Eleonora Lamantea 2 , Daniele Ghezzi 2,3 , Enza Maria Valente 4,5 , Vincenzo Nigro 6 and Stefano D’Arrigo 1 1 Developmental Neurology Unit, Fondazione IRCCS Istituto Neurologico Carlo Besta, 20133 Milano, Italy; [email protected] (C.P.); [email protected] (S.D.) 2 Unit of Medical Genetics and Neurogenetics, Fondazione IRCCS Istituto Neurologico Carlo Besta, 20133 Milano, Italy; [email protected] (F.T.); [email protected] (D.D.B.); [email protected] (S.M.); [email protected] (E.L.); [email protected] (D.G.) 3 Department of Pathophysiology and Transplantation, University of Milan, 20122 Milano, Italy 4 Department of Molecular Medicine, University of Pavia, 27100 Pavia, Italy; [email protected] 5 Neurogenetics Research Centre, IRCCS Mondino Foundation, 27100 Pavia, Italy 6 Telethon Institute of Genetics and Medicine, 80078 Napoli, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-02-2394-2217 Featured Application: The study proposes a possible approach to pediatric ataxias with cerebellar atrophy, in order to optimize the diagnostic process and reach molecular confirmation. Abstract: Background: Cerebellar atrophy is a neuroradiological definition that categorizes condi- tions heterogeneous for clinical findings, disease course, and genetic defect. Most of the papers proposing a diagnostic workup for pediatric ataxias are based on neuroradiology or on the literature Citation: Ciaccio, C.; Pantaleoni, C.; and experimental knowledge, with a poor participation of clinics in the process of disease definition. -

Whole Exome Sequencing Gene Package Multiple Congenital Anomaly, Version 8.1, 31-1-2020
Whole Exome Sequencing Gene package Multiple congenital anomaly, version 8.1, 31-1-2020 Technical information DNA was enriched using Agilent SureSelect DNA + SureSelect OneSeq 300kb CNV Backbone + Human All Exon V7 capture and paired-end sequenced on the Illumina platform (outsourced). The aim is to obtain 10 Giga base pairs per exome with a mapped fraction of 0.99. The average coverage of the exome is ~50x. Duplicate and non-unique reads are excluded. Data are demultiplexed with bcl2fastq Conversion Software from Illumina. Reads are mapped to the genome using the BWA-MEM algorithm (reference: http://bio-bwa.sourceforge.net/). Variant detection is performed by the Genome Analysis Toolkit HaplotypeCaller (reference: http://www.broadinstitute.org/gatk/). The detected variants are filtered and annotated with Cartagenia software and classified with Alamut Visual. It is not excluded that pathogenic mutations are being missed using this technology. At this moment, there is not enough information about the sensitivity of this technique with respect to the detection of deletions and duplications of more than 5 nucleotides and of somatic mosaic mutations (all types of sequence changes). HGNC approved Phenotype description including OMIM phenotype ID(s) OMIM median depth % covered % covered % covered gene symbol gene ID >10x >20x >30x A4GALT [Blood group, P1Pk system, P(2) phenotype], 111400 [Blood group, P1Pk system, p phenotype], 111400 NOR poly607922 146 100 100 99 AAAS Achalasia-addisonianism-alacrimia syndrome, 231550 605378 102 100 100 100 -

Clinical, Cognitive and Behavioural Assessment in Children with Cerebellar Disorder
applied sciences Review Clinical, Cognitive and Behavioural Assessment in Children with Cerebellar Disorder Stefano D’Arrigo *, Carmela Loiacono, Claudia Ciaccio , Chiara Pantaleoni, Flavia Faccio, Matilde Taddei and Sara Bulgheroni Developmental Neurology Department, Fondazione IRCCS Istituto Neurologico C. Besta, 20133 Milan, Italy; [email protected] (C.L.); [email protected] (C.C.); [email protected] (C.P.); fl[email protected] (F.F.); [email protected] (M.T.); [email protected] (S.B.) * Correspondence: [email protected]; Tel.: +39-2-23942211 Featured Application: The study summarizes the clinical and neuropsychological evaluation in children with cerebellar disorder, highlighting the specific characteristics of the child age useful to define a diagnostic pathway. Abstract: Cerebellar disorders are characterised clinically by specific signs and symptoms, often asso- ciated with neurodevelopmental disorder. While the clinical signs of cerebellar disorders are clearly recognisable in adults and have a precise anatomo-functional correlation, in children the semiotics are less clear and vary with age because of the particular nature of the cerebellum’s maturation. Unlike other structures of the central nervous system, this begins at a later stage of foetal development and extends over a longer period of time, even after birth. As a result, the typical signs of cerebellar dysfunction will only become evident when the cerebellar functions have become integrated into the complex circuits of the central nervous system. This means that poor motor coordination in the very early years of life may not necessarily correlate with cerebellar dysfunction, and this may Citation: D’Arrigo, S.; Loiacono, C.; also be encountered in healthy children.